Mitochondria As Target of Endocrine-Disrupting Chemicals: Implications for Type 2 Diabetes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

4-6 Weeks Old Female C57BL/6 Mice Obtained from Jackson Labs Were Used for Cell Isolation
Methods Mice: 4-6 weeks old female C57BL/6 mice obtained from Jackson labs were used for cell isolation. Female Foxp3-IRES-GFP reporter mice (1), backcrossed to B6/C57 background for 10 generations, were used for the isolation of naïve CD4 and naïve CD8 cells for the RNAseq experiments. The mice were housed in pathogen-free animal facility in the La Jolla Institute for Allergy and Immunology and were used according to protocols approved by the Institutional Animal Care and use Committee. Preparation of cells: Subsets of thymocytes were isolated by cell sorting as previously described (2), after cell surface staining using CD4 (GK1.5), CD8 (53-6.7), CD3ε (145- 2C11), CD24 (M1/69) (all from Biolegend). DP cells: CD4+CD8 int/hi; CD4 SP cells: CD4CD3 hi, CD24 int/lo; CD8 SP cells: CD8 int/hi CD4 CD3 hi, CD24 int/lo (Fig S2). Peripheral subsets were isolated after pooling spleen and lymph nodes. T cells were enriched by negative isolation using Dynabeads (Dynabeads untouched mouse T cells, 11413D, Invitrogen). After surface staining for CD4 (GK1.5), CD8 (53-6.7), CD62L (MEL-14), CD25 (PC61) and CD44 (IM7), naïve CD4+CD62L hiCD25-CD44lo and naïve CD8+CD62L hiCD25-CD44lo were obtained by sorting (BD FACS Aria). Additionally, for the RNAseq experiments, CD4 and CD8 naïve cells were isolated by sorting T cells from the Foxp3- IRES-GFP mice: CD4+CD62LhiCD25–CD44lo GFP(FOXP3)– and CD8+CD62LhiCD25– CD44lo GFP(FOXP3)– (antibodies were from Biolegend). In some cases, naïve CD4 cells were cultured in vitro under Th1 or Th2 polarizing conditions (3, 4). -

Effect of STAT3 Inhibition on the Metabolic Switch in a Highly STAT3-Activated Lymphoma Cell Line
CANCER GENOMICS & PROTEOMICS 12 : 133-142 (2015) Effect of STAT3 Inhibition on the Metabolic Switch in a Highly STAT3-activated Lymphoma Cell Line YASUTO AKIYAMA 1* , AKIRA IIZUKA 1* , AKIKO KUME 1, MASARU KOMIYAMA 1, KENICHI URAKAMI 2, TADASHI ASHIZAWA 1, HARUO MIYATA 1, MAHO OMIYA 1, MASATOSHI KUSUHARA 3 and KEN YAMAGUCHI 4 1Immunotherapy Division, 2Cancer Diagnostics Division, 3Regional Resources Division, Shizuoka Cancer Center Research Institute, Sunto-gun, Shizuoka, Japan; 4Office of the President, Shizuoka Cancer Center Hospital, Sunto-gun, Shizuoka, Japan Abstract. Background: Signal transducer and activator of enzymes including fructose-bisphosphate aldolase A transcription (STAT)3 is involved in a metabolic shift in (ALDOA) as a metabolic marker candidate for STAT3- cancer cells, the Warburg effect through its pro-oncogenic targeting therapy using STAT3-specific shRNA gene activity. To develop efficient STAT3 inhibitors against cancer transduction. In particular, latexin expression was up- cells, novel proteomic and metabolic target molecules need regulated in four STAT3-activated cancer cell lines including to be explored using multi-omics approaches in the context of SCC-3 transduced with STAT3-specific shRNA. The up- STAT3 gene inhibition-mediated tumor growth suppression. regulation of latexin was identified in SCC-3 tumors Materials and Methods: We found that short hairpin transplanted to nude mice after treatment with STAT3 (sh)RNA-mediated STAT3 inhibition suppressed tumor inhibitor. Conclusion: Our results suggest that STAT3 growth in a highly STAT3-activated lymphoma cell line, inactivation reverses the glycolytic shift by down-regulating SCC-3 cells, and we investigated the effect of STAT3 key enzymes and that it induces up-regulation of latexin as a inhibition on metabolic switching using 2-dimensional tumor-suppressor molecule, which partially results in cancer differential gel electrophoresis and capillary electrophoresis- cell apoptosis and tumor growth suppression. -

Ubiquitin and Ubiquitin-Like Proteins Are Essential Regulators of DNA Damage Bypass
cancers Review Ubiquitin and Ubiquitin-Like Proteins Are Essential Regulators of DNA Damage Bypass Nicole A. Wilkinson y, Katherine S. Mnuskin y, Nicholas W. Ashton * and Roger Woodgate * Laboratory of Genomic Integrity, National Institute of Child Health and Human Development, National Institutes of Health, 9800 Medical Center Drive, Rockville, MD 20850, USA; [email protected] (N.A.W.); [email protected] (K.S.M.) * Correspondence: [email protected] (N.W.A.); [email protected] (R.W.); Tel.: +1-301-435-1115 (N.W.A.); +1-301-435-0740 (R.W.) Co-first authors. y Received: 29 August 2020; Accepted: 29 September 2020; Published: 2 October 2020 Simple Summary: Ubiquitin and ubiquitin-like proteins are conjugated to many other proteins within the cell, to regulate their stability, localization, and activity. These modifications are essential for normal cellular function and the disruption of these processes contributes to numerous cancer types. In this review, we discuss how ubiquitin and ubiquitin-like proteins regulate the specialized replication pathways of DNA damage bypass, as well as how the disruption of these processes can contribute to cancer development. We also discuss how cancer cell survival relies on DNA damage bypass, and how targeting the regulation of these pathways by ubiquitin and ubiquitin-like proteins might be an effective strategy in anti-cancer therapies. Abstract: Many endogenous and exogenous factors can induce genomic instability in human cells, in the form of DNA damage and mutations, that predispose them to cancer development. Normal cells rely on DNA damage bypass pathways such as translesion synthesis (TLS) and template switching (TS) to replicate past lesions that might otherwise result in prolonged replication stress and lethal double-strand breaks (DSBs). -

STAT3-Mediated Metabolic Reprograming in Cellular Transformation and Implications for Drug Resistance
MINI REVIEW published: 08 June 2015 doi: 10.3389/fonc.2015.00121 STAT3-mediated metabolic reprograming in cellular transformation and implications for drug resistance Valeria Poli* and Annalisa Camporeale* Department of Molecular Biotechnology and Health Sciences, Molecular Biotechnology Center, University of Torino, Torino, Italy Signal transducer and activator of transcription (STAT)3 mediates the signaling down- stream of cytokine and growth factor receptors, regulating the expression of target genes. It is constitutively phosphorylated on tyrosine (Y-P) in many tumors, where its transcrip- tional activity can induce a metabolic switch toward aerobic glycolysis and down-regulate mitochondrial activity, a prominent metabolic feature of most cancer cells, correlating Edited by: Gavin P. McStay, with reduced production of ROS, delayed senescence, and protection from apoptosis. New York Institute of Technology, USA STAT3 can, however, also localize to mitochondria, where its serine-phosphorylated Reviewed by: (S-P) form preserves mitochondrial oxidative phosphorylation and controls the opening Masaaki Murakami, of the mitochondrial permeability transition pore, also promoting survival and resistance Hokkaido University, Japan Yun Dai, to apoptosis in response to specific signals/oncogenes such as RAS. Thus, downstream Virginia Commonwealth University of different signals, both nuclear, Y-P STAT3, and mitochondrial, S-P STAT3, can act by and Massey Cancer Center, USA promoting cell survival and reducing ROS production. Here, we discuss -
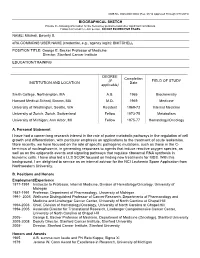
BIOGRAPHICAL SKETCH NAME: Mitchell, Beverly
OMB No. 0925-0001/0002 (Rev. 08/12 Approved Through 8/31/2015) BIOGRAPHICAL SKETCH Provide the following information for the Senior/key personnel and other significant contributors. Follow this format for each person. DO NOT EXCEED FIVE PAGES. NAME: Mitchell, Beverly S. eRA COMMONS USER NAME (credential, e.g., agency login): BMITCHELL POSITION TITLE: George E. Becker Professor of Medicine Director, Stanford Cancer Institute EDUCATION/TRAINING DEGREE Completion (if FIELD OF STUDY INSTITUTION AND LOCATION Date applicable) Smith College, Northampton, MA A.B. 1965 Biochemistry Harvard Medical School, Boston, MA M.D. 1969 Medicine University of Washington, Seattle, WA Resident 1969-72 Internal Medicine University of Zurich, Zurich, Switzerland Fellow 1973-75 Metabolism University of Michigan, Ann Arbor, MI Fellow 1975-77 Hematology/Oncology A. Personal Statement I have had a career-long research interest in the role of purine metabolic pathways in the regulation of cell growth and differentiation, with particular emphasis on applications to the treatment of acute leukemias. More recently, we have focused on the role of specific pathogenic mutations, such as those in the C- terminus of nucleophosmin, in generating responses to agents that induce reactive oxygen species, as well as on the epigenetic events and signaling pathways that regulate ribosomal RNA synthesis in leukemic cells. I have also led a LLS SCOR focused on finding new treatments for MDS. With this background, I am delighted to service as an internal advisor for the NCI Leukemia -

A Novel DNA Primase-Helicase Pair Encoded by Sccmec Elements Aleksandra Bebel†, Melissa a Walsh, Ignacio Mir-Sanchis‡, Phoebe a Rice*
RESEARCH ARTICLE A novel DNA primase-helicase pair encoded by SCCmec elements Aleksandra Bebel†, Melissa A Walsh, Ignacio Mir-Sanchis‡, Phoebe A Rice* Department of Biochemistry and Molecular Biology, University of Chicago, Chicago, United States Abstract Mobile genetic elements (MGEs) are a rich source of new enzymes, and conversely, understanding the activities of MGE-encoded proteins can elucidate MGE function. Here, we biochemically characterize three proteins encoded by a conserved operon carried by the Staphylococcal Cassette Chromosome (SCCmec), an MGE that confers methicillin resistance to Staphylococcus aureus, creating MRSA strains. The first of these proteins, CCPol, is an active A-family DNA polymerase. The middle protein, MP, binds tightly to CCPol and confers upon it the ability to synthesize DNA primers de novo. The CCPol-MP complex is therefore a unique primase- polymerase enzyme unrelated to either known primase family. The third protein, Cch2, is a 3’-to-5’ helicase. Cch2 additionally binds specifically to a dsDNA sequence downstream of its gene that is also a preferred initiation site for priming by CCPol-MP. Taken together, our results suggest that this is a functional replication module for SCCmec. *For correspondence: Introduction [email protected] Staphylococcus aureus is a dangerous human pathogen, due in part to the emergence of multi- drug-resistant strains such as MRSA (methicillin-resistant S. aureus). MRSA strains have acquired † Present address: Phage resistance to b-lactam antibiotics (including methicillin) mainly through horizontal gene transfer of a Consultants, Gdynia, Poland; mobile genomic island called staphylococcal cassette chromosome (SCC) (Moellering, 2012). ‡Umea˚ University, Umea˚ , SCCmec is a variant of SCC that carries a methicillin resistance gene, mecA. -

Enzymes Involved in Organellar DNA Replication in Photosynthetic Eukaryotes
REVIEW ARTICLE published: 17 September 2014 doi: 10.3389/fpls.2014.00480 Enzymes involved in organellar DNA replication in photosynthetic eukaryotes Takashi Moriyama1,2 and Naoki Sato1,2 * 1 Department of Life Sciences, Graduate School of Arts and Sciences, The University of Tokyo, Tokyo, Japan 2 Japan Science and Technology Agency – Core Research for Evolutional Science and Technology, Tokyo, Japan Edited by: Plastids and mitochondria possess their own genomes. Although the replication mecha- Thomas Pfannschmidt, Université nisms of these organellar genomes remain unclear in photosynthetic eukaryotes, several Joseph Fourier Grenoble, France organelle-localized enzymes related to genome replication, including DNA polymerase, Reviewed by: DNA primase, DNA helicase, DNA topoisomerase, single-stranded DNA maintenance Ján A. Miernyk, University of Missouri, USA protein, DNA ligase, primer removal enzyme, and several DNA recombination-related Mee-Len Chye, The University of enzymes, have been identified. In the reference Eudicot plant Arabidopsis thaliana, the Hong Kong, China replication-related enzymes of plastids and mitochondria are similar because many of them *Correspondence: are dual targeted to both organelles, whereas in the red alga Cyanidioschyzon merolae, plas- Naoki Sato, Department of Life tids and mitochondria contain different replication machinery components. The enzymes Sciences, Graduate School of Arts and Sciences, The University of Tokyo, involved in organellar genome replication in green plants and red algae were derived from Komaba 3-8-1, Meguro-ku, Tokyo different origins, including proteobacterial, cyanobacterial, and eukaryotic lineages. In the 153-8902, Japan present review, we summarize the available data for enzymes related to organellar genome e-mail: [email protected] replication in green plants and red algae. -

Inhibition of Mutagenic Translesion Synthesis: a Possible Strategy for Improving Chemotherapy?
VIEWPOINTS Inhibition of mutagenic translesion synthesis: A possible strategy for improving chemotherapy? Kinrin Yamanaka1☯, Nimrat Chatterjee1☯, Michael T. Hemann1,2, Graham C. Walker1* 1 Department of Biology, Massachusetts Institute of Technology, Cambridge, Massachusetts, United States of America, 2 Koch Institute, Massachusetts Institute of Technology, Cambridge, Massachusetts, United States of America ☯ These authors contributed equally to this work. * [email protected] a1111111111 Overview a1111111111 DNA damaging chemotherapy is the first line of treatment for certain cancers, but its long- a1111111111 term success is often marred by the eventual acquisition of chemoresistance. Other cancers a1111111111 a1111111111 cannot be treated because they are intrinsically resistant to such chemotherapy. These 2 types of resistance are coupled in the context of translesion synthesis (TLS), which is carried out by specialized TLS DNA polymerases that can replicate past DNA lesions but in a lower fidelity manner. First, TLS DNA polymerases permit the bypass of modified DNA bases during DNA synthesis, thereby allowing proliferation to continue in the presence of chemotherapy, an issue OPEN ACCESS of particular relevance to intrinsic drug resistance. Second, mistakes introduced by TLS poly- Citation: Yamanaka K, Chatterjee N, Hemann MT, merases copying over DNA lesions introduced during the chemotherapy lead to mutations Walker GC (2017) Inhibition of mutagenic that contribute to acquired resistance. These dual functions of mutagenic TLS polymerases translesion synthesis: A possible strategy for with respect to chemoresistance make these proteins very promising targets for adjuvant ther- improving chemotherapy? PLoS Genet 13(8): apy. The major branch of mutagenic TLS requires REV1, a Y family DNA polymerase that e1006842. https://doi.org/10.1371/journal. -

Multi‐Omics Analysis Reveals the Interaction Between The
www.nature.com/scientificreports OPEN Multi‐omics analysis reveals the interaction between the complement system and the coagulation cascade in the development of endometriosis Liang Yu1,3, Huaji Shen2,3, Xiaohan Ren1,3, Anqi Wang1, Shu Zhu1, Yafeng Zheng2* & Xiuli Wang1* Endometriosis (EMS) is a disease that shows immune dysfunction and chronic infammation characteristics, suggesting a role of complement system in its pathophysiology. To fnd out the hub genes and pathways involved in the pathogenesis of EMs, three raw microarray datasets were recruited from the Gene Expression Omnibus database (GEO). Then, a series of bioinformatics technologies including gene ontology (GO), Hallmark pathway enrichment, protein–protein interaction (PPI) network and gene co-expression correlation analysis were performed to identify hub genes. The hub genes were further verifed by the Real-time quantitative polymerase chain reaction (RT-PCR) and Western Blot (WB). We identifed 129 diferentially expressed genes (DEGs) in EMs, of which 78 were up-regulated and 51 were down-regulated. Through GO functional enrichment analysis, we found that the DEGs are mainly enriched in cell adhesion, extracellular matrix remodeling, chemokine regulation, angiogenesis regulation, epithelial cell proliferation, et al. In Hallmark pathway enrichment analysis, coagulation pathway showed great signifcance and the terms in which included the central complement factors. Moreover, the genes were dominating in PPI network. Combined co-expression analysis with experimental verifcation, we found that the up-regulated expression of complement (C1S, C1QA, C1R, and C3) was positively related to tissue factor (TF) in EMs. In this study, we discovered the over expression complement and the positive correlation between complement and TF in EMs, which suggested that interaction of complement and coagulation system may play a role within the pathophysiology of EMS. -

DNA Replication
DNA replication: • Copying genetic information for transmission to the next generation • Occurs in S phase of cell cycle • Process of DNA duplicating itself • Begins with the unwinding of the double helix to expose the bases in each strand of DNA • Each unpaired nucleotide will attract a complementary nucleotide from the medium – will form base pairing via hydrogen bonding. • Enzymes link the aligned nucleotides by phosphodiester bonds to form a continuous strand. 1 DNA replication: – First question asked was whether duplication was semiconservative or conservative • Meselson and Stahl expt • Semiconservative - – one strand from parent in each new strand • Conservative- – both strands from parent and other is all new strands 2 DNA replication: • Complementary base pairing produces semiconservative replication – Double helix unwinds – Each strand acts as template – Complementary base pairing ensures that T signals addition of A on new strand, and G signals addition of C – Two daughter helices produced after replication 3 4 Experimental proof of semiconservative replication – three possible models • Semiconservative replication – – Watson and Crick model • Conservative replication: – The parental double helix remains intact; – both strands of the daughter double helix are newly synthesized • Dispersive replication: – At completion, both strands of both double helices contain both original and newly synthesized material. 5 6 Meselson-Stahl experiments confirm semiconservative replication • Experiment allowed differentiation of parental and newly formed DNA. • Bacteria were grown in media containing either normal isotope of nitrogen (14N) or the heavy isotope (15N). • DNA banded after equilibrium density gradient centrifugation at a position which matched the density of the DNA: – heavy DNA was at a higher density than normal DNA. -

The Pdx1 Bound Swi/Snf Chromatin Remodeling Complex Regulates Pancreatic Progenitor Cell Proliferation and Mature Islet Β Cell
Page 1 of 125 Diabetes The Pdx1 bound Swi/Snf chromatin remodeling complex regulates pancreatic progenitor cell proliferation and mature islet β cell function Jason M. Spaeth1,2, Jin-Hua Liu1, Daniel Peters3, Min Guo1, Anna B. Osipovich1, Fardin Mohammadi3, Nilotpal Roy4, Anil Bhushan4, Mark A. Magnuson1, Matthias Hebrok4, Christopher V. E. Wright3, Roland Stein1,5 1 Department of Molecular Physiology and Biophysics, Vanderbilt University, Nashville, TN 2 Present address: Department of Pediatrics, Indiana University School of Medicine, Indianapolis, IN 3 Department of Cell and Developmental Biology, Vanderbilt University, Nashville, TN 4 Diabetes Center, Department of Medicine, UCSF, San Francisco, California 5 Corresponding author: [email protected]; (615)322-7026 1 Diabetes Publish Ahead of Print, published online June 14, 2019 Diabetes Page 2 of 125 Abstract Transcription factors positively and/or negatively impact gene expression by recruiting coregulatory factors, which interact through protein-protein binding. Here we demonstrate that mouse pancreas size and islet β cell function are controlled by the ATP-dependent Swi/Snf chromatin remodeling coregulatory complex that physically associates with Pdx1, a diabetes- linked transcription factor essential to pancreatic morphogenesis and adult islet-cell function and maintenance. Early embryonic deletion of just the Swi/Snf Brg1 ATPase subunit reduced multipotent pancreatic progenitor cell proliferation and resulted in pancreas hypoplasia. In contrast, removal of both Swi/Snf ATPase subunits, Brg1 and Brm, was necessary to compromise adult islet β cell activity, which included whole animal glucose intolerance, hyperglycemia and impaired insulin secretion. Notably, lineage-tracing analysis revealed Swi/Snf-deficient β cells lost the ability to produce the mRNAs for insulin and other key metabolic genes without effecting the expression of many essential islet-enriched transcription factors.