Report of Market Conduct Examination
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Directors Guild of America, Inc. National Commercial Agreement of 2017
DIRECTORS GUILD OF AMERICA, INC. NATIONAL COMMERCIAL AGREEMENT OF 2017 TABLE OF CONTENTS Page WITNESSETH: 1 ARTICLE 1 RECOGNITION AND GUILD SHOP 1-100 RECOGNITION AND GUILD SHOP 1-101 RECOGNITION 2 1-102 GUILD SHOP 2 1-200 DEFINITIONS 1-201 COMMERCIAL OR TELEVISION COMMERCIAL 4 1-202 GEOGRAPHIC SCOPE OF AGREEMENT 5 1-300 DEFINITIONS OF EMPLOYEES RECOGNIZED 1-301 DIRECTOR 5 1-302 UNIT PRODUCTION MANAGERS 8 1-303 FIRST ASSISTANT DIRECTORS 9 1-304 SECOND ASSISTANT DIRECTORS 10 1-305 EXCLUSIVE JURISDICTION 10 ARTICLE 2 DISPUTES 2-101 DISPUTES 10 2-102 LIQUIDATED DAMAGES 11 2-103 NON-PAYMENT 11 2-104 ACCESS AND EXAMINATION OF BOOKS 11 AND RECORDS ARTICLE 3 PENSION AND HEALTH PLANS 3-101 EMPLOYER PENSION CONTRIBUTIONS 12 3-102 EMPLOYER HEALTH CONTRIBUTIONS 12 i 3-103 LOAN-OUTS 12 3-104 DEFINITION OF SALARY FOR PENSION 13 AND HEALTH CONTRIBUTIONS 3-105 REPORTING CONTRIBUTIONS 14 3-106 TRUST AGREEMENTS 15 3-107 NON-PAYMENT OF PENSION AND HEALTH 15 CONTRIBUTIONS 3-108 ACCESS AND EXAMINATION OF BOOKS 16 RECORDS 3-109 COMMERCIAL INDUSTRY ADMINISTRATIVE FUND 17 ARTICLE 4 MINIMUM SALARIES AND WORKING CONDITIONS OF DIRECTORS 4-101 MINIMUM SALARIES 18 4-102 PREPARATION TIME - DIRECTOR 18 4-103 SIXTH AND SEVENTH DAY, HOLIDAY AND 19 LAYOVER TIME 4-104 HOLIDAYS 19 4-105 SEVERANCE PAY FOR DIRECTORS 20 4-106 DIRECTOR’S PREPARATION, COMPLETION 20 AND TRAVEL TIME 4-107 STARTING DATE 21 4-108 DIRECTOR-CAMERAPERSON 21 4-109 COPY OF SPOT 21 4-110 WORK IN EXCESS OF 18 HOURS 22 4-111 PRODUCTION CENTERS 22 ARTICLE 5 STAFFING, MINIMUM SALARIES AND WORKING CONDITIONS -

Img Signature Travel Insurancesm
IMG SIGNATURE TRAVEL INSURANCESM BENEFITS SIGNATURE TRAVEL INSURANCE BENEFITS SIGNATURE TRAVEL INSURANCE Available – if purchased within 20 days of initial trip Trip Cancellation Trip cost insured (up to $100,000) Pre-existing Condition Waiver payment Trip Interruption 150% of trip cost insured Common Carrier AD&D Up to $100,000 Travel Delay Up to $1,000 ($250 per day max after delay of 6 hrs) Search & Rescue Up to $10,000 Missed Connection Up to $500 (after a delay of 3 hours) Sports Equipment Rental Up to $2,000 ($500 Day Max) Change Fee Up to $300 Waives excluded sports/ Included Reimbursement of Miles or recreation activities Up to $75 Reward Points Rental Car Damage Up to $40,000 Lost/Baggage Up to $2,500 Coverage Type Primary Baggage Delay Up to $500 Cancel for Any Reason Up to 75% of the trip cost insured if purchased Emergency Medical Up to $100,000 (UPGRADE) within 20 days of initial trip payment Interrupt for Any Reason Up to 75% of the trip cost insured Emergency Dental Up to $1,000 (UPGRADE) TRAVEL COVERAGE BAGGAGE & EQUIPMENT COVERAGE TRIP CANCELLATION/INTERRUPTION BAGGAGE AND PERSONAL EFFECTS You can be reimbursed for unused travel arrangements, as well as up to $75 for fees If your baggage or personal effects are lost, stolen or damaged, we will cover the to rebank frequent flyer miles, for reasons such as death or covered sickness or injury loss or cost of repair. If your baggage is delayed for more than 24 hours after you of you, family member, traveling companion, business partner or child caregiver; being reach your -

In the Supreme Court of Missouri En Banc ) ) ) ) Appeal
Electronically Filed - SUPREME COURT OF MISSOURI December 21, 2016 06:20 PM IN THE SUPREME COURT OF MISSOURI EN BANC OWNERS INSURANCE COMPANY, ) ) APPELLANT, ) ) VS. ) APPEAL NO. SC95843 ) VICKI CRAIG and CHRIS CRAIG, ) ) RESPONDENTS. ) APPEAL FROM THE CIRCUIT COURT OF GREENE COUNTY STATE OF MISSOURI THE HONORABLE JASON R. BROWN CIRCUIT JUDGE SUBSTITUTE REPLY BRIEF OF APPELLANT OWNERS INSURANCE COMPANY Russell F. Watters #25758 [email protected] T. Michael Ward #32816 [email protected] BROWN & JAMES, P.C. 800 Market Street, Suite 1100 St. Louis, Missouri 63101 314-421-3400 314-421-3128 (Facsimile) Attorneys for Appellant Owners Insurance Company Electronically Filed - SUPREME COURT OF MISSOURI December 21, 2016 06:20 PM TABLE OF CONTENTS TABLE OF AUTHORITIES ...................................................................................................... iii REPLY STATEMENT OF FACTS .............................................................................................. 1 REPLY ARGUMENT ............................................................................................................... 3 I. The trial court erred in entering summary judgment for Defendants Vicki Craig and Chris Craig, and in denying summary judgment for Owners Insurance Company, because Owners was entitled to reduce the sum due Defendants on their claim for underinsured motorist coverage, in that the Owners policy clearly and unambiguously provided for a $50,000 deduction from the $250,000 each person limit of liability for underinsured motorist coverage -

2020 Annual Report
2020 ANNUAL REPORT Shelter Insurance Companies 1817 West Broadway • Columbia, MO 65218 1-800-SHELTER (1-800-743-5837) ShelterInsurance.com Facebook: ShelterInsurance Twitter: Shelter_ins YouTube: ShelterIns Instagram: Shelter_ins LinkedIn: Shelter-Insurance-Companies STRONG SHELTER Shelter’s 75th Anniversary Shelter Insurance® is celebrating 75 years in 2021. In 2018, those who came before us was in need of an update, it made sense Executive Vice Presidents Teresa Magruder and Dan Clapp to tie the renovation to the 75th anniversary. The new area is called established an interdepartmental committee and started planning the Inspiration Garden and features a wall naming employees and efforts for Shelter’s diamond anniversary. Some efforts kicked off in agents who have passed away as well as a unique rock sculpture and 2020, with the majority of events and activities taking place in 2021. a water feature. A bronze plaque includes Shelter’s 75th anniversary logo and a dedication honoring those we have lost. The plaque was Logo installed in October 2020 and visitors are encouraged to visit this peaceful and lovely place when at the corporate headquarters in The Shelter logo was enhanced for the anniversary and is featured Columbia, Missouri. throughout the website, ads, employee volunteer t-shirts, company car decals and more. Celebrating 75 Years Giving Special 75th anniversary elements will be added to normal activities throughout 2021 including the Garden Concerts and the Holiday Shelter is providing eligible employees 8 hours of paid volunteer Tree Lighting. A golf tournament in the Summer and a special leave during the anniversary year. Plans are also underway to sponsor Celebration Day in the Fall are also planned. -

Built on Strength Building Fortomorrow
ANNUAL REPORT 2015 Shelter Insurance Companies BUILT ON STRENGTH BUILDING FORTOMORROW ® Contents 2 A Word to Our Policyholders 4 Company News 12 Dedication to Our Communities 19 Company Overview 32 Directors & Officers Mission Statement Shelter Insurance® will be a dynamic group of Companies focused on providing financially secure insurance protection and services to individuals and businesses, a quality working environment, emphasis on easy-to-use services, a commitment to continuous improvement, and a passion for pleasing our customers. 2015 ANNUAL REPORT SHELTER INSURANCE COMPANIES 1 Reflections from the Chair of Shelter’s Board of Directors The theme of this year’s Annual Report is Built on Strength…Building for Tomorrow. I believe this theme is perfect for a year that included significant physical changes to Shelter’s facilities as well as the continued building of new brands and Companies within our group. The commitment to innovation within our Companies is only possible because of the strong financial foundation Shelter enjoys today. On behalf of the Board of Directors, we applaud the spirit of innovation building in our agents and employees, led by our Management Team. In this report you’ll learn more about our foray into the world of Agile development processes from an IT perspective. We’re updating and improving our facilities, providing employees a more modern Don McCubbin, Chairman of the workspace that improves energy efficiencies and ergonomics. The Companies and brands Board of Directors, retired from we’re building will improve our geographic expansion efforts and our new product Shelter in 2012 as an Executive distribution opportunities will expand growth potential significantly. -
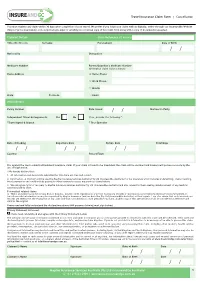
Cancellation Claim Form
Travel Insurance Claim Form | Cancellation You must register any claim within 30 days after completion of your travel. We prefer if you lodge your claim with us digitally, either through our InsureandGo Website (https://quote.insureandgo.com.au/policylogin.aspx) or emailing us a scanned copy of this claim form along with a copy of documents requested. Claimant Details Claim Reference (if known) Title (Mr/Mrs etc) Surname Forename(s) Date of Birth / / Nationality Occupation Medicare Number Parent/Guardian’s Medicare Number (If medical claim is for a minor) Home Address ' Home Phone ' Work Phone ' Mobile State Postcode Email Policy Details Policy Number Date Issued / / Number in Party Independent Travel Arrangements: Yes No If no, provide the following *: *Travel Agent & Branch * Tour Operator Date of Booking Departure Date Return Date Total Days / / / / / / Country Resort/Town It is against the law to submit a fraudulent insurance claim. If your claim is found to be fraudulent the claim will be declined and Insurers will pursue recovery by the use of legal action. I/We hereby declare that: 1. All information and documents submitted for this claim are true and correct. 2. Information on this form will be used by Mapfre Insurance Services Australia Pty Ltd (InsureandGo Australia) for my insurance which includes underwriting, claims handling, fraud prevention and could include passing to other insurers to access my previous claims history. 3. We subrogate rights of recovery to Mapfre Insurance Services Australia Pty Ltd (InsureandGo Australia) and also consent to them seeking reimbursement of any medical expenses paid by them. For medical related claims: 4. -
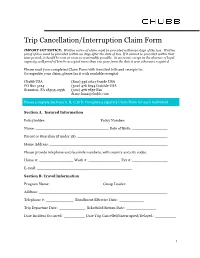
Trip Cancellation/Interruption Claim Form
Trip Cancellation/Interruption Claim Form IMPORTANT NOTICE: Written notice of claim must be provided within 90 days of the loss. Written proof of loss must be provided within 90 days after the date of loss. If it cannot be provided within that time period, it should be sent as soon as reasonably possible. In no event, except in the absence of legal capacity, will proof of loss be accepted more than one year from the date it was otherwise required. Please mail your completed Claim Form with itemized bills and receipts to: (to expedite your claim, please fax it with readable receipts) Chubb USA (800) 336 0627 Inside USA PO Box 5124 (302) 476 6194 Outside USA Scranton, PA 18505-0556 (302) 476 7857 Fax [email protected] Please complete Sections A, B, C, & D. Complete a separate Claim Form for each individual. Section A. Insured Information Policyholder: Policy Number: Name: Date of Birth: Parent or Guardian (if under 18): Home Address: Please provide telephone and facsimile numbers, with country and city codes. Home #: Work #: Fax #: E-mail: Section B. Travel Information Program Name: Group Leader: Address: Telephone #: Enrollment Effective Date: Trip Departure Date: Scheduled Return Date: Date Incident Occurred: Date Trip Cancelled/Interrupted/Delayed: 1 Section C. Reason for Claim (provide additional pages if necessary): Section D. Physician or Provider Name of physician or provider: Phone #: Address: Diagnosis or nature of illness or injury: Date of illness (first symptom) or injury: Date first consulted for this condition: Hospital -

We're Your Shield. We're Your Shelter
We’re your Shield. We’re your Shelter. Shelter Insurance® - Count on our Team. Shelter Insurance Companies 2010 Annual Report Table of Contents 2010 Overview President’s Letter .............................................................................................1 Corporate Oversight Discussion .........................................................................2 Corporate Oversight Chart ................................................................................3 2010 in Review ...........................................................................................4-11 Companywide Information ..............................................................................12 A Family of Companies ...................................................................................13 Financial Results ....................................................................................... 14-25 Directors and Officers .....................................................................................26 Community Involvement ............................................................................ 27-32 Shelter Privacy Protection Policy ......................................................................33 2010 AnnuAl RepoRt President’s Letter Page 1 To Our Policyholders: The year 2010 brought about the continued recovery of investable asset values as the Dow Jones Industrial Average ended the year at 11,578, a remarkable improvement over the mid 6,000 in March 2009. Short term and bond interest rates, however, remained -

1 United States Fire Insurance Company
United States Fire Insurance Company Administrative Office: 5 Christopher Way, Eatontown, NJ 07724 (Hereinafter referred to as “the Company”) TRAVEL PROTECTION PLAN This Certificate of Insurance describes the insurance benefits underwritten by United States Fire Insurance Company, herein referred to as the Company and also referred to as We, Us and Our. The insurance benefits vary from program to program. Please refer to the accompanying Confirmation of Benefits, which provides the Insured, also referred to as You or Your, with specific information about the program You purchased. You should contact the Company immediately if You believe that the Confirmation of Benefits is incorrect. Signed for United States Fire Insurance Company By: Marc J. Adee Chairman and CEO Insurance provided by this Certificate is subject to all of the terms and conditions of the Group Policy. If there is a conflict between the Policy and this Certificate, the Policy will govern. If You are not satisfied for any reason, You may return Your Certificate to Travel Insurance Services within 15 days after receipt. Your premium will be refunded, provided You have not already departed on the Trip or filed a claim. When so returned, the coverage under the Certificate is void from the beginning. Renewal: Coverage under this Certificate is not renewable. SHORT TERM COVERAGE NON-RENEWABLE TABLE OF CONTENTS SCHEDULE OF BENEFITS SECTION I. COVERAGES SECTION II. DEFINITIONS SECTION III INSURING PROVISIONS SECTION IV. GENERAL EXCLUSIONS SECTION V. GENERAL PROVISIONS SECTION VI COORDINATION OF BENEFITS SCHEDULE OF BENEFITS Maximum Benefit Amount/Principal Sum Part A – Travel Arrangement Protection Trip Cancellation ................................................... -
DB MF PW RCSTD 0314.Pdf
DB/MF/PW/RCSTD/0314 10 things to do before you go Important 1. Check the Foreign and Commonwealth Office (FCO) travel Under the new travel directive from the European Union (EU), advice online at www.gov.uk/knowbeforeyougo. you are entitled to claim compensation from your airline if any of the following happen. 2. Get travel insurance and check that the cover is appropriate. 1. You are not allowed to board or your flight is cancelled. If you check-in on time but you are not allowed to board 3. Get a good guidebook and get to know the place you are because there are too many passengers for the number of going to. Find out about local laws and customs. seats available or your flight is cancelled, the airline operating the flight must offer you financial compensation. 4. Make sure you have a valid passport and any visas you need. 2. There are long delays. If you are delayed for two hours or more, the airline must 5. Check what vaccinations you need at least six weeks before offer you meals and refreshments, hotel accommodation you go. and communication facilities. If you are delayed for more than five hours, the airline must also offer to refund your 6. Check to see if you need to take extra health precautions ticket. (visit www.nhs.uk/travelhealth) 3. Your baggage is damaged, lost or delayed. 7. Make sure whoever you book your trip through is a If your checked-in baggage is damaged or lost by an EU member of the Association of British Travel Agents (ABTA) airline, you must make a claim to the airline within seven or the Air Travel Organisers' Licensing scheme (ATOL). -

Property and Casualty Insurance
CHAPTER 26.1-39 PROPERTY AND CASUALTY INSURANCE 26.1-39-01. Rescission of fire insurance contract for alteration increasing risk. An alteration in the use or condition of a thing insured from that to which it is limited by the policy, if made without the consent of the insurer, by means within the control of the insured, and if it increases the risk, entitles an insurer to rescind a fire insurance contract. 26.1-39-02. Rescission of fire contract not permitted if risk not increased. An alteration in the use or condition of a thing insured from that to which it is limited by the policy, which does not increase the risk, does not affect a fire insurance contract. 26.1-39-03. When fire contract unaffected though risk increased. A fire insurance contract is not affected by any act of the insured subsequent to the execution of the policy, if the act does not violate its provisions, even though it increases the risk and is the cause of a loss. 26.1-39-04. Measure of indemnity on fire policy. If there is no valuation in the policy, the measure of indemnity in an insurance against fire is the full amount stated in the policy. If there is a valuation in the policy, the valuation is conclusive between the parties in the adjustment either of a partial or a total loss if the insured has some interest at risk and there is no fraud on the insured's part. In the event of a partial loss, the insurer is liable only for the proportion of the amount insured as the loss bears to the value of the whole interest of the insured in the property insured. -

Shelter Life Insurance Policyholder Privacy Policy Notice
Rev. 8-2015 FACTS WHAT DOES SHELTER LIFE INSURANCE COMPANY DO WITH YOUR PERSONAL INFORMATION? Why? Financial companies choose how they share your personal information. Federal law gives consumers the right to limit some but not all sharing. Federal law also requires us to tell you how we collect, share, and protect your personal information. Please read this notice carefully to understand what we do. What? The types of personal information we collect and share depend on the product or service you have with us. This information can include: • Social security number • Credit-based insurance scores • Insurance claim history • Medical information • Checking account information • Employment information When you are no longer our customer, we continue to share your information as described in this notice. How? All financial companies need to share customers' personal information to run their everyday business. In the section below, we list the reasons financial companies can share their customers' personal information; the reasons Shelter Life Insurance Company chooses to share; and whether you can limit this sharing. Does Shelter Life Can you limit this Reasons we can share your personal information Insurance Company sharing? share? For our everyday business purposes – such as to process your transactions, maintain your Yes No account(s), respond to court orders and legal investigations, or report to the credit bureaus For our marketing purposes – Yes No To offer our products and services to you For joint marketing with other financial companies