Western District of Pennsylvania Addresses Enforceability of the Regular Use Exclusion in Light of the Gallagher Decision
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MORGAN STATE FOOTBALL HISTORY & RECORDS MSU RECORD BOOK RUSHING Rushing Yards - Career 2,727 Ali Culpepper 605 Atts
MORGAN STATE FOOTBALL HISTORY & RECORDS MSU RECORD BOOK RUSHING Rushing Yards - Career 2,727 Ali Culpepper 605 atts. 1998-01 Rushing Yards - Game 2,548 Robert Hammonds 590 atts. 1971-74 (min. 125 yards) 2,539 John Sykes 536 1967-71 271 Herb Walker 29 atts. Holy Cross 2014 2,539 John Sykes 536 atts. 1969-71 251 Jason Jackson 22 atts Savannah State 2005 2,422 Devan James 474 atts. 2006-09 229 Ali Culpepper 32 atts. B-Cookman 2001 2,197 Chad Simpson 423 atts. 2006-07 221 Chad Simpson 41 atts. W-Salem St. 2007 2,086 Alphonso Harris 457 atts. 1982-85 219 Devan James 36 atts. Howard 2008 2,048 Lloyd McCleave 487 atts. 1975-78 215 Chad Simpson 32 atts. Norfolk State 2007 1,986 Herb Walker Jr. 375 atts. 2014-17 212 Ali Culpepper 44 atts. Hampton 2001 1,858 Jason Jackson 341 atts. 2004-05 203 Herb Walker 22 atts. Florida A&M 2014 1,690 Travis Davidson 350 atts. 2011-12 203 Craig Nelson 29 att. Bowie State 2004 1,510 T.J. Stallings 311 atts. 1999-02 201 Bobby Hammond 29 atts. N.C. A&T 1973 1,451 James Fields 323 atts. 1980-82 195 Chad Simpson 25 atts. Towson 2007 1,424 Andre Thomas 314 atts. 1992-95 192 Chad Simpson 26 atts. Norfolk State 2006 1,380 Tony Phillips 304 atts. 1992-93 182 John Sykes 29 atts. N.C. Central 1970 1,337 Jimmy Joe 301 atts. 1969-71 181 Chad Simpson 33 atts. N.C. -

December 4, 2020 Pittsburgh Catholic Issue
12/4/2020 https://pittsburghcatholic.org/?format=print&post-type=post&order-date=desc&order-menu=asc&statuses%5B%5D=publish&taxonomies%5Btags%5… Posts with Tag: Featured, from pittsburghcatholic.org. Printed on December 4, 2020 Hope through the Holy Family: Dec. 13 event DECEMBER 4, 2020 Categories: News Tags: Diocesan News, Featured This Advent, after a year of unprecedented trials and uncertainties, the Holy Family’s journey to Bethlehem is a reminder that Christ never forgets His people. That is the theme of Advent Hope: A Journey with the Holy Family, a virtual event featuring Bishop David Zubik and Father Boniface Hicks, OSB. Father Hicks is the general manager and on-air host of We Are One Body Catholic radio (WAOB 106.7 FM), and speaks on the spiritual life at Catholic conferences, retreats and courses. The event will take place from 7- 8:30 p.m. on December 13, 2020, the third Sunday of Advent, or Gaudete Sunday, when Catholics reect on the joy of Christ’s coming. It will be livestreamed from St. Anthony Chapel in Pittsburgh’s Troy Hill, home to the largest collection of Christian relics in the world outside of the Vatican. The idea grew from the desire to create a communal faith experience this Advent, at a time when many in- person traditions are cancelled because of the pandemic. “We realized that we needed to have a virtual event to help people keep their eyes on Jesus during this Advent season,” said Judene Indovina, diocesan director of Catholic Identity. Father Hicks will reect on what it means to travel the dicult road to Bethlehem with Mary and Joseph, condent that the joy of Christ’s coming is near. -
2007 FB Guide.Indd
Left facing page GOBLUERAIDERS.COM 145 LeftBlue facing Raider page History Division I in today’s terms with a 57-7 win over Memphis State. In the fi nal game of the 1925 season, the Middle Tennessee Teachers College (as it was known from 1925 to 1942) took its longest road trip of the team’s existence. The Normals made their way to central Florida to take on Stetson. The Hatters won the game 10-0 in a contest played on a natural surface of sand. In 1926, Frank Faulkinberry began his fi rst season at the helm. Not only did Faulkinberry serve as football coach, he was also the school’s basketball and baseball coach as well as a professor. He produced an overall 32-24-4 record during his seven years as head coach. In a game against North Alabama in 1927, 76 points were put up by MTSTC, which still stands as the most points Johnny “Red” Floyd Stadium was constructed in 1933 as Horace Jones Field. The facility had portable scored in one game. bleachers for about the fi rst 15 years until a major renovation put concrete grandstands in place in the In 1929, the football team played its 1940s. fi rst ten-game schedule, going 6-3-1 on 1910s to World War I. Although he returned the season. In 1912, the Middle Tennessee Nor- in 1919, a young man by the name of mal School strapped up and donned Johnny “Red” Floyd took over for him 1930s the pads for the fi rst time as L. -

Stealers OFFENSE 48 Rawser, John CB 51 Ball, Lorry LB LE68L.C
MIAMI DOLPHINSvs.PITTSBURGHSTEELIRS DOLPHINS DECEMBER 3,1973 — ORANGE BOWL, MIAMI STEELERS NO. NAME POS. NO. NAME PUS. 1 Yapremian, Gwo K 5 Honesty, terry OS 10Strock, Den OB OFFENSE DEFENSE 10 Qerelo, Roy K 12Grin., Bob OR 12 Sradshaw, Tqrry OS 13Scott, Jake $ WR 42 Paul Warfield 82 Bo Rather 34 Ron Sellers LE83 Vern Den Herder 72 Bob Heinz Ti Gilliarn,Jo. OS 15Morrall, Earl 89 Charley Wade LI75 Manny Fernandez 65 Maulty Moore 20 BItter. Rocky RB 23 Wagner, Mike 20Seiple, Larry P-T[ LI79 Wayne Moore 77 Ooug Cruson 76 Willie Young RI72 Bob Heinz 10 Larry Woods $ 21Kiick, Jim 24 Thama*,James CS-S RB LG67 Bob Kuechenberg64 Ed Newman RE84 Bill Stanfill 72 Bob Heinz 25 Shank tin, Ron 22Morris, Mercury RB LIB59 Doug Swift 51 Larry Ball C62 Jim Langer 55 lrv Goode 36 Peenos'i, Preston RB 23Leigh, Charles RB MIB85 Nick Buoniconti 53 Sob Mâtheson RG66 Larry little 55 try Goode 27 Edwards, Glen S 25Foley, urn CB 57 Mike Kolen 58 Bruce Bannon RI73 Norm Evans 77 Doug Crusan RIB 29 Dockery, John CS 26Mumphord, Lloyd CS TE 88 Jim Mandich LCB26 Lloyd Mumphord 25 Tim Foley RB 20Smith, Tom RB 80 Mary Fleming 20 LarrySeiple 32 Harris, Franco RCB45 Curtis Johnson 48 Henry Stuckey 34Sellers, Ron WR WR86 Marlin Briscoe 81 Howard Twilley 33 Puque, John RB FS13 Jake Scoff 49 Charles Babb 34 Russell, Andy LB 36Nottingham, Don RB QB12 Bob Griese 15 Earl Morrall 10Don Strock 35 Davis, Steve RB 39Csonka, Larry RB RB22 Mercury Morris 21 Jim Kiick 23Charles Leigh 5540 Dick Anderson 49 Charles Babb 38 Bradley, Ed LB 40Anderson, Dick 5 RB39 Larry Csonka 36 Don Nottingham 29Tom Smith 39 WaLden, Bobby P 42Worfield, Paul WR 41 Meyer, Dennis S 45Johnson, Curtis CB 43 Lewis, Frank WR 48Stuckey, Henry CB 47 Blount, Mel CB 49Bobb, Charles S Steelors DEFENSE Stealers OFFENSE 48 Rawser, John CB 51 Ball, Lorry LB LE68L.C. -

2013 Steelers Media Guide 5
history Steelers History The fifth-oldest franchise in the NFL, the Steelers were founded leading contributors to civic affairs. Among his community ac- on July 8, 1933, by Arthur Joseph Rooney. Originally named the tivities, Dan Rooney is a board member for The American Ireland Pittsburgh Pirates, they were a member of the Eastern Division of Fund, The Pittsburgh History and Landmarks Foundation and The the 10-team NFL. The other four current NFL teams in existence at Heinz History Center. that time were the Chicago (Arizona) Cardinals, Green Bay Packers, MEDIA INFORMATION Dan Rooney has been a member of several NFL committees over Chicago Bears and New York Giants. the past 30-plus years. He has served on the board of directors for One of the great pioneers of the sports world, Art Rooney passed the NFL Trust Fund, NFL Films and the Scheduling Committee. He was away on August 25, 1988, following a stroke at the age of 87. “The appointed chairman of the Expansion Committee in 1973, which Chief”, as he was affectionately known, is enshrined in the Pro Football considered new franchise locations and directed the addition of Hall of Fame and is remembered as one of Pittsburgh’s great people. Seattle and Tampa Bay as expansion teams in 1976. Born on January 27, 1901, in Coultersville, Pa., Art Rooney was In 1976, Rooney was also named chairman of the Negotiating the oldest of Daniel and Margaret Rooney’s nine children. He grew Committee, and in 1982 he contributed to the negotiations for up in Old Allegheny, now known as Pittsburgh’s North Side, and the Collective Bargaining Agreement for the NFL and the Players’ until his death he lived on the North Side, just a short distance Association. -
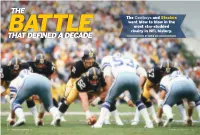
That Defined a Decade by David Lee Getty Images
THE The Cowboys and Steelers went blow to blow in the most star-studded BATTLE rivalry in NFL history. THAT DEFINED A DECADE BY DAVID LEE GETTY IMAGES 80 • VINTAGE COLLECTOR 24 VINTAGE COLLECTOR 24 • 81 #12. LYNN SWANN’S he Cleveland Browns dominated the NFL in the 1940s and ’50s. The CIRCUS CATCH Green Bay Packers bullied the league through the ’60s. But after the The 12th greatest play on the list hap- AFL and NFL finally merged, the 1970s was a decade of struggle between pened just two games after the Hail Mary the Dallas Cowboys and Pittsburgh Steelers that wouldn’t be settled in Super Bowl X between the Cowboys until January 1979. and Steelers. It was a clash of north vs. south, NFC vs. AFC, Noll vs. Landry, Bradshaw vs. Staubach, the Hail “It was a mistake,” Lynn Swann said on TMary and The Immaculate Reception. the NFL Films presentation of the play’s Through the decade, Dallas won 105 regular-season games and 14 postseason games. The Steelers won 99 in the ranking. “Obviously Mark Washington regular season and 14 in the postseason. The Steelers made it to the AFC Championship Game six times and went 4-0 tipped the ball away. If I actually caught it in Super Bowls. The Cowboys reached the NFC Championship Game seven times and were 2-3 in Super Bowls. without it being tipped, I might have run it Of the 48 total players selected to the NFL’s 1970s All-Decade Team, 14 are Cowboys or Steelers—nearly one- into the end zone for a touchdown.” third of the list. -

Pittsburgh Steelers Game Release Week 15 Cincinnati Bengals
WEEK 15 - BENGALS VS. STEELERS | 1 PITTSBURGH STEELERS 3400 South Water Street • Pittsburgh, PA 15203 412-432-7820 • Fax: 412-432-7878 PITTSBURGH STEELERS GAME RELEASE WEEK 15 CINCINNATI BENGALS GAME INFORMATION 2020 REGULAR SCHEDULE (11-2) Monday, December 21 Paul Brown Stadium Day Date Opponent Location TV Time/Result 8:15 p.m. ET Cincinnati, OH (65,535) Mon. Sept. 14 New York Giants MetLife Stadium W, 26-16 ESPN Steve Levy (play-by-play) Sun. Sept. 20 Denver Heinz Field W, 26-21 Locally WTAE-TV Brian Griese (analysis) Louis Riddick (analysis) Sun. Sept. 27 Houston Heinz Field W, 28-21 Lisa Salters (field reporter) Sun. Oct. 4 BYE WEEK* Steelers Radio Network (48 affiliates) Bill Hillgrove (play-by-play) Sun. Oct. 11 Philadelphia Heinz Field W, 39-28 102.5 WDVE-FM (Pittsburgh) Tunch Ilkin (analysis) Sun. Oct. 18 Cleveland Heinz Field W, 38-7 970 WBGG-AM (Pittsburgh) Craig Wolfley (analysis) Missi Matthews (field reporter) Sun. Oct. 25 Tennessee* Nissan Stadium W, 27-24 THE SERIES Sun. Nov. 1 Baltimore* M&T Bank Stadium W, 28-24 All-Time Steelers lead, 67-35 Last: Steelers Win, 36-10 (Nov. 15, 2020) Sun. Nov. 8 Dallas AT&T Stadium W, 24-19 Home Steelers lead, 35-16 Last: Steelers Win, 36-10 (Nov. 15, 2020) Sun. Nov. 15 Cincinnati Heinz Field W, 36-10 Away Steelers lead, 32-19 Last: Steelers Win, 16-10 (Nov. 24, 2019) Sun. Nov. 22 Jacksonville EverBank Field W, 27-3 THE COACHES Wed. Dec. 2 Baltimore# Heinz Field W, 19-14 Mon. -

The Following Players Comprise the 1975 Season APBA Pro Football Player Card Set
1975 APBA PRO FOOTBALL SET ROSTER The following players comprise the 1975 season APBA Pro Football Player Card Set. The regular starters at each position are listed first and should be used most frequently. Realistic use of the players below will generate statistical results remarkably similar to those from real life. IMPORTANT: When a Red "K" appears in the R-column as the result on any kind of running play from scrimmage or on any return, roll the dice again, refer to the K-column, and use the number there for the result. When a player has a "K" in his R-column, he can never be used for kicking or punting. If the symbol "F-K" or "F-P" appears on a players card, it means that you use the K or P column when he recovers a fumble. ATLANTA 4-10 BALTIMORE 10-4 BUFFALO 8-6 CHICAGO 4-10 OFFENSE OFFENSE OFFENSE OFFENSE WR: Ken Burrow WR: Roger Carr WR: Bob Chandler WR: Bob Grim Alfred Jenkins TC OC Glenn Doughty J.D. Hill Bo Rather OC Wallace Francis OA Freddie Scott John Holland TC OC Steve Schubert TC OC Tackle: Len Gotshalk Tackle: George Kunz Tackle: Donnie Green Tackle: Jeff Sevy Brent Adams Dave Taylor Dave Foley Lionel Antoine Nick Bebout Ed George Halvor Hagen Bob Asher Guard: Dennis Havig Guard: Elmer Collett Jeff Winans Guard: Mark Nordquist Larron Jackson Robert Pratt OC Guard: Joe DeLamielleure Noah Jackson Royce Smith Bob Van Duyne Reggie McKenzie OC Revie Sorey Center: Jeff Van Note Ken Huff Jeff Yeates Bob Newton Paul Ryczek Center: Ken Mendenhall Bill Adams Center: Dan Peiffer TE: Jim Mitchell Forrest Blue Center: Mike Montler Dan Neal Greg McCrary OC TE: Raymond Chester Willie Parker TE: Bob Parsons (2) PA KB KOB QB: Steve Bartkowski Jimmie Kennedy OC TE: Paul Seymour Greg Latta Kim McQuilken QB: Bert Jones Reuben Gant Gary Butler Pat Sullivan Marty Domres QB: Joe Ferguson QB: Gary Huff HB: Haskel Stanback Bill Troup Gary Marangi Bob Avellini Mack Herron (2) TA OB HB: Lydell Mitchell HB: O.J. -

Nfl & Uso Mark 40Th Anniversary; Seahawks
FOR IMMEDIATE RELEASE NFL Contact: NFL-13 3/22/06 Pete Abitante, (212) 450-2065 [email protected] USO Contact: Erica Stone, (703) 908-6471 [email protected] NFL & USO MARK 40TH ANNIVERSARY; SEAHAWKS’ FISHER, FALCONS’ KERNEY & STEELERS’ STARKS TO VISIT TROOPS IN BALKANS & PERSIAN GULF REGIONS The National Football League and the USO (United Service Organizations) will celebrate the 40th anniversary of their partnership this spring with a tour that will soon head to the Balkans and the Persian Gulf Region to provide a morale boost to troops stationed far from home. Defensive ends BRYCE FISHER of the NFC champion Seattle Seahawks and PATRICK KERNEY of the Atlanta Falcons, and tackle MAX STARKS of the Super Bowl XL champion Pittsburgh Steelers will meet and greet service members at various locations in the region. Armed Forces Entertainment (AFE) is providing logistical support for the trip. In 1966, the NFL became the first sports organization to send players to Vietnam and other parts of the Far East on “goodwill tours” to visit U.S. troops. The first group of players to embark on a USO tour overseas included four future Hall of Famers: WILLIE DAVIS, FRANK GIFFORD, SAM HUFF and JOHNNY UNITAS. In 2004, the NFL donated $250,000 to the USO for the construction of the Pat Tillman USO Center in Afghanistan, located at Bagram Air Base near Kabul. LARRY IZZO of the New England Patriots and WARRICK DUNN of the Falcons attended the opening of the center last April in Afghanistan. A former Arizona Cardinals safety, Tillman was killed during Army Ranger combat operations in Afghanistan in 2004. -

Pittsburgh Steelers Game Release Week 17 Cleveland Browns
WEEK 17 - BROWNS VS. STEELERS | 1 PITTSBURGH STEELERS COMMUNICATIONS Burt Lauten - Director of Communications Michael Bertsch - Communications Manager Angela Tegnelia - Communications Coordinator PITTSBURGH STEELERS Alissa Cavaretta - Communications Assistant/Social Media 3400 South Water Street • Pittsburgh, PA 15203 Thomas Chapman - Communications Intern 412-432-7820 • Fax: 412-432-7878 PITTSBURGH STEELERS GAME RELEASE WEEK 17 CLEVELAND BROWNS GAME INFORMATION 2020 REGULAR SCHEDULE (12-3) Sunday, January 3 FirstEnergy Stadium Day Date Opponent Location TV Time/Result 1 p.m. ET Cleveland, OH Mon. Sept. 14 New York Giants MetLife Stadium W, 26-16 Capacity 67,895 // Natural Grass Sun. Sept. 20 Denver Heinz Field W, 26-21 CBS Ian Eagle (play-by-play) Locally KDKA-TV Charles Davis (analysis) Sun. Sept. 27 Houston Heinz Field W, 28-21 Evan Washburn (analysis) Sun. Oct. 4 BYE WEEK* Steelers Radio Network (48 affiliates) Bill Hillgrove (play-by-play) Sun. Oct. 11 Philadelphia Heinz Field W, 39-28 102.5 WDVE-FM (Pittsburgh) Tunch Ilkin (analysis) Sun. Oct. 18 Cleveland Heinz Field W, 38-7 970 WBGG-AM (Pittsburgh) Craig Wolfley (analysis) Missi Matthews (field reporter) Sun. Oct. 25 Tennessee* Nissan Stadium W, 27-24 THE SERIES Sun. Nov. 1 Baltimore* M&T Bank Stadium W, 28-24 All-Time Steelers lead, 25-6 Last: Steelers Win, 26-24 (Nov. 3, 2019) Sun. Nov. 8 Dallas AT&T Stadium W, 24-19 Home Steelers lead, 15-2 Last: Steelers Win, 26-24 (Nov. 3, 2019) Sun. Nov. 15 Cincinnati Heinz Field W, 36-10 Away Steelers lead, 10-4 Last: Steelers Win, 20-17 (Nov. -

Steelersprdept
WEEK 11 - STEELERS AT JAGUARS | 1 PITTSBURGH STEELERS COMMUNICATIONS Burt Lauten - Director of Communications Michael Bertsch - Communications Manager Angela Tegnelia - Communications Coordinator PITTSBURGH STEELERS Alissa Cavaretta - Communications Assistant/Social Media 3400 South Water Street • Pittsburgh, PA 15203 Thomas Chapman - Communications Intern 412-432-7820 • Fax: 412-432-7878 PITTSBURGH STEELERS GAME RELEASE WEEK 11 JACKSONVILLE JAGUARS GAME INFORMATION 2020 REGULAR SCHEDULE (9-0) Sunday, November 22 TIAA Bank Field Day Date Opponent Location TV Time/Result 1 p.m. ET Jacksonville, FL Mon. Sept. 14 New York Giants MetLife Stadium W, 26-16 Capacity 67,164 // Natural Grass Sun. Sept. 20 Denver Heinz Field W, 26-21 CBS Ian Eagle (play-by-play) Locally WKDKA-TV Charles Davis (analysis) Sun. Sept. 27 Houston Heinz Field W, 28-21 Evan Washburn (field reporter) Sun. Oct. 4 BYE WEEK* Steelers Radio Network (48 affiliates) Bill Hillgrove (play-by-play) Sun. Oct. 11 Philadelphia Heinz Field W, 39-28 102.5 WDVE-FM (Pittsburgh) Tunch Ilkin (analysis) Sun. Oct. 18 Cleveland Heinz Field W, 38-7 970 WBGG-AM (Pittsburgh) Craig Wolfley (analysis) Missi Matthews (field reporter) Sun. Oct. 25 Tennessee* Nissan Stadium W, 27-24 THE SERIES Sun. Nov. 1 Baltimore* M&T Bank Stadium W, 28-24 All-Time Jaguars lead, 14-12 Last: Steelers Win, 20-16 (Nov. 18, 2018) Sun. Nov. 8 Dallas AT&T Stadium W, 24-19 Home Jaguars lead, 7-6 Last: Jaguars Win, 45-42 (Jan. 14, 2018) Sun. Nov. 15 Cincinnati Heinz Field W, 36-10 Away Jaguars lead, 7-6 Last: Steelers Win, 20-16 (Nov. -

Pittsburgh Steelers Vs. Indianapolis Colts Game Release
WEEK 16 - STEELERS VS. COLTS | 1 PITTSBURGH STEELERS COMMUNICATIONS Burt Lauten - Director of Communications Michael Bertsch - Communications Manager Angela Tegnelia - Communications Coordinator PITTSBURGH STEELERS Alissa Cavaretta - Communications Assistant/Social Media 3400 South Water Street • Pittsburgh, PA 15203 Thomas Chapman - Communications Intern 412-432-7820 • Fax: 412-432-7878 PITTSBURGH STEELERS GAME RELEASE WEEK 16 INDIANAPOLIS COLTS GAME INFORMATION 2020 REGULAR SCHEDULE (11-3) Sunday, December 27 Heinz Field Day Date Opponent Location TV Time/Result 1 p.m. ET Pittsburgh, PA Mon. Sept. 14 New York Giants MetLife Stadium W, 26-16 Capacity 68,400 // Natural Grass Sun. Sept. 20 Denver Heinz Field W, 26-21 CBS Jim Nantz (play-by-play) Locally KDKA-TV Tony Romo (analysis) Sun. Sept. 27 Houston Heinz Field W, 28-21 Tracy Wolfson (field reporter) Sun. Oct. 4 BYE WEEK* Steelers Radio Network (48 affiliates) Bill Hillgrove (play-by-play) Sun. Oct. 11 Philadelphia Heinz Field W, 39-28 102.5 WDVE-FM (Pittsburgh) Tunch Ilkin (analysis) Sun. Oct. 18 Cleveland Heinz Field W, 38-7 970 WBGG-AM (Pittsburgh) Craig Wolfley (analysis) Missi Matthews (field reporter) Sun. Oct. 25 Tennessee* Nissan Stadium W, 27-24 THE SERIES Sun. Nov. 1 Baltimore* M&T Bank Stadium W, 28-24 All-Time Steelers lead, 25-6 Last: Steelers Win, 26-24 (Nov. 3, 2019) Sun. Nov. 8 Dallas AT&T Stadium W, 24-19 Home Steelers lead, 15-2 Last: Steelers Win, 26-24 (Nov. 3, 2019) Sun. Nov. 15 Cincinnati Heinz Field W, 36-10 Away Steelers lead, 10-4 Last: Steelers Win, 20-17 (Nov.