Prenatal Testing Requisition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Disease Reference Book
The Counsyl Foresight™ Carrier Screen 180 Kimball Way | South San Francisco, CA 94080 www.counsyl.com | [email protected] | (888) COUNSYL The Counsyl Foresight Carrier Screen - Disease Reference Book 11-beta-hydroxylase-deficient Congenital Adrenal Hyperplasia .................................................................................................................................................................................... 8 21-hydroxylase-deficient Congenital Adrenal Hyperplasia ...........................................................................................................................................................................................10 6-pyruvoyl-tetrahydropterin Synthase Deficiency ..........................................................................................................................................................................................................12 ABCC8-related Hyperinsulinism........................................................................................................................................................................................................................................ 14 Adenosine Deaminase Deficiency .................................................................................................................................................................................................................................... 16 Alpha Thalassemia............................................................................................................................................................................................................................................................. -

Neonatal Hemochromatosis: a Congenital Alloimmune Hepatitis
Reprinted with permission from Thieme Medical Publishers (Semin Liver Dis. 2007 Aug;27(3):243-250) Homepage at www.thieme.com Neonatal Hemochromatosis: A Congenital Alloimmune Hepatitis Peter F. Whitington, M.D.1 ABSTRACT Neonatal hemochromatosis (NH) is a rare and enigmatic disease that has been clinically defined as severe neonatal liver disease in association with extrahepatic siderosis. It recurs at an alarming rate in the offspring of certain women; the rate and pattern of recurrence led us to hypothesize that maternal alloimmunity is the likely cause at least of recurrent cases. This hypothesis led to a trial of gestational treatment to prevent the recurrence of severe NH, which has been highly successful adding strength to the alloimmune hypothesis. Laboratory proof of an alloimmune mechanism has been gained by reproducing the disease in a mouse model. NH should be suspected in any very sick newborn with evidence of liver disease and in cases of late intrauterine fetal demise. Given the pathology of the liver and the mechanism of liver injury, NH could best be classified as congenital alloimmune hepatitis. KEYWORDS: Neonatal hemochromatosis, acute liver failure, alloimmune disease, cirrhosis, hepatitis Neonatal hemochromatosis (NH) is clinically NH could best be classified as congenital alloimmune defined as severe neonatal liver disease in association hepatitis. with extrahepatic siderosis in a distribution similar to that seen in hereditary hemochromatosis.1–4 Consider- able evidence indicates that it is a gestational disease in ETIOLOGY AND PATHOGENESIS which fetal liver injury is the dominant feature. Because The name hemochromatosis implies that iron is involved of the abnormal accumulation of iron in liver and other in the pathogenesis of NH. -

GRACILE Syndrome, a Lethal Metabolic Disorder with Iron
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Am. J. Hum. Genet. 71:863–876, 2002 GRACILE Syndrome, a Lethal Metabolic Disorder with Iron Overload, Is Caused by a Point Mutation in BCS1L Ilona Visapa¨a¨,1,3 Vineta Fellman,7 Jouni Vesa,1 Ayan Dasvarma,8 Jenna L. Hutton,2 Vijay Kumar,5 Gregory S. Payne,2 Marja Makarow,5 Rudy Van Coster,9 Robert W. Taylor,10 Douglass M. Turnbull,10 Anu Suomalainen,6 and Leena Peltonen1,3,4 Departments of 1Human Genetics and 2Biological Chemistry, University of California Los Angeles School of Medicine, Los Angeles; 3Department of Molecular Medicine, National Public Health Institute, 4Department of Medical Genetics, 5Institute of Biotechnology, and 6Department of Neurology and Programme of Neurosciences, University of Helsinki, and 7Hospital for Children and Adolescents, Helsinki University Central Hospital, Helsinki; 8Murdoch Children’s Research Institute, Melbourne, Australia; 9Department of Pediatrics, Ghent University Hospital, Ghent, Belgium; and 10Department of Neurology, University of Newcastle upon Tyne, Newcastle, United Kingdom GRACILE (growth retardation, aminoaciduria, cholestasis, iron overload, lactacidosis, and early death) syndrome is a recessively inherited lethal disease characterized by fetal growth retardation, lactic acidosis, aminoaciduria, cholestasis, and abnormalities in iron metabolism. We previously localized the causative gene to a 1.5-cM region on chromosome 2q33-37. In the present study, we report the molecular defect causing this metabolic disorder, by identifying a homozygous missense mutation that results in an S78G amino acid change in the BCS1L gene in Finnish patients with GRACILE syndrome, as well as five different mutations in three British infants. -

Human Mitochondrial Pathologies of the Respiratory Chain and ATP Synthase: Contributions from Studies of Saccharomyces Cerevisiae
life Review Human Mitochondrial Pathologies of the Respiratory Chain and ATP Synthase: Contributions from Studies of Saccharomyces cerevisiae Leticia V. R. Franco 1,2,* , Luca Bremner 1 and Mario H. Barros 2 1 Department of Biological Sciences, Columbia University, New York, NY 10027, USA; [email protected] 2 Department of Microbiology,Institute of Biomedical Sciences, Universidade de Sao Paulo, Sao Paulo 05508-900, Brazil; [email protected] * Correspondence: [email protected] Received: 27 October 2020; Accepted: 19 November 2020; Published: 23 November 2020 Abstract: The ease with which the unicellular yeast Saccharomyces cerevisiae can be manipulated genetically and biochemically has established this organism as a good model for the study of human mitochondrial diseases. The combined use of biochemical and molecular genetic tools has been instrumental in elucidating the functions of numerous yeast nuclear gene products with human homologs that affect a large number of metabolic and biological processes, including those housed in mitochondria. These include structural and catalytic subunits of enzymes and protein factors that impinge on the biogenesis of the respiratory chain. This article will review what is currently known about the genetics and clinical phenotypes of mitochondrial diseases of the respiratory chain and ATP synthase, with special emphasis on the contribution of information gained from pet mutants with mutations in nuclear genes that impair mitochondrial respiration. Our intent is to provide the yeast mitochondrial specialist with basic knowledge of human mitochondrial pathologies and the human specialist with information on how genes that directly and indirectly affect respiration were identified and characterized in yeast. Keywords: mitochondrial diseases; respiratory chain; yeast; Saccharomyces cerevisiae; pet mutants 1. -

Prenatal Comprehensive Requisition
BAYLOR GENETICS PHONE CONNECT 2450 HOLCOMBE BLVD. 1.800.411.4363 GRAND BLVD. RECEIVING DOCK FAX HOUSTON, TX 77021-2024 1.800.434.9850 PRENATAL COMPREHENSIVE REQUISITION PATIENT INFORMATION (COMPLETE ONE FORM FOR EACH PERSON TESTED) / / Fetus of: Patient Last Name Patient First Name MI Date of Birth (MM / DD / YYYY) / Biological /Sex Fetus of: Patient Last Name Patient First Name MI Date of Birth (MM / DD / YYYY) Address City State Zip Phone Patient discharged from Biological Sex: the hospital/facility: Female Male Unknown Accession # Hospital / Medical Record # Yes No Gender identity (if diff erent from above): REPORTING RECIPIENTS Ordering Physician Institution Name Email (Required for International Clients) Phone Fax ADDITIONAL RECIPIENTS Name Email Fax Name Email Fax PAYMENT (FILL OUT ONE OF THE OPTIONS BELOW) SELF PAYMENT Pay With Sample Bill To Patient INSTITUTIONAL BILLING Institution Name Institution Code Institution Contact Name Institution Phone Institution Contact Email INSURANCE REQUIRED ITEMS 1. Copy of the Front/Back of Insurance Card(s) 2. ICD10 Diagnosis Code(s) 3. Name of Ordering Physician 4. Insured Signature of Authorization / / / / Name of Insured Insured Date of Birth (MM / DD / YYYY) Name of Insured Insured Date of Birth (MM / DD / YYYY) Patient's Relationship to Insured Phone of Insured Patient's Relationship to Insured Phone of Insured Address of Insured Address of Insured City State Zip City State Zip Primary Insurance Co. Name Primary Insurance Co. Phone Secondary Insurance Co. Name Secondary Insurance Co. Phone Primary Member Policy # Primary Member Group # Secondary Member Policy # Secondary Member Group # By signing below, I hereby authorize Baylor Genetics to provide my insurance carrier any information necessary, including test results, for processing my insurance claim. -
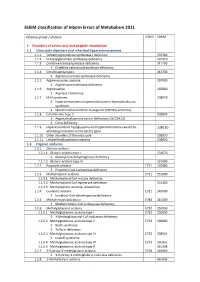
SSIEM Classification of Inborn Errors of Metabolism 2011
SSIEM classification of Inborn Errors of Metabolism 2011 Disease group / disease ICD10 OMIM 1. Disorders of amino acid and peptide metabolism 1.1. Urea cycle disorders and inherited hyperammonaemias 1.1.1. Carbamoylphosphate synthetase I deficiency 237300 1.1.2. N-Acetylglutamate synthetase deficiency 237310 1.1.3. Ornithine transcarbamylase deficiency 311250 S Ornithine carbamoyltransferase deficiency 1.1.4. Citrullinaemia type1 215700 S Argininosuccinate synthetase deficiency 1.1.5. Argininosuccinic aciduria 207900 S Argininosuccinate lyase deficiency 1.1.6. Argininaemia 207800 S Arginase I deficiency 1.1.7. HHH syndrome 238970 S Hyperammonaemia-hyperornithinaemia-homocitrullinuria syndrome S Mitochondrial ornithine transporter (ORNT1) deficiency 1.1.8. Citrullinemia Type 2 603859 S Aspartate glutamate carrier deficiency ( SLC25A13) S Citrin deficiency 1.1.9. Hyperinsulinemic hypoglycemia and hyperammonemia caused by 138130 activating mutations in the GLUD1 gene 1.1.10. Other disorders of the urea cycle 238970 1.1.11. Unspecified hyperammonaemia 238970 1.2. Organic acidurias 1.2.1. Glutaric aciduria 1.2.1.1. Glutaric aciduria type I 231670 S Glutaryl-CoA dehydrogenase deficiency 1.2.1.2. Glutaric aciduria type III 231690 1.2.2. Propionic aciduria E711 232000 S Propionyl-CoA-Carboxylase deficiency 1.2.3. Methylmalonic aciduria E711 251000 1.2.3.1. Methylmalonyl-CoA mutase deficiency 1.2.3.2. Methylmalonyl-CoA epimerase deficiency 251120 1.2.3.3. Methylmalonic aciduria, unspecified 1.2.4. Isovaleric aciduria E711 243500 S Isovaleryl-CoA dehydrogenase deficiency 1.2.5. Methylcrotonylglycinuria E744 210200 S Methylcrotonyl-CoA carboxylase deficiency 1.2.6. Methylglutaconic aciduria E712 250950 1.2.6.1. Methylglutaconic aciduria type I E712 250950 S 3-Methylglutaconyl-CoA hydratase deficiency 1.2.6.2. -

Mitokondriesykdommer
Mitokondriesykdommer Genpanel, versjon v02 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering Gen Transkript >10x Fenotype AARS NM_001605.2 100% Epileptic encephalopathy, early infantile, 29 OMIM PubMed Charcot-Marie-Tooth disease, axonal, type 2N OMIM AARS2 NM_020745.3 100% Combined oxidative phosphorylation deficiency 8 OMIM ABCB7 NM_004299.4 100% Cerebellar ataxia with or without sideroblastic anemia OMIM ACAD9 NM_014049.4 100% Mitochondrial complex I deficiency OMIM ACO2 NM_001098.2 97% Infantile cerebellar-retinal degeneration OMIM ADCK3 NM_020247.4 100% Coenzyme Q10 deficiency, primary, 4 OMIM ADCK4 NM_024876.3 100% Nephrotic syndrome, type 9, with or without seizures, mild mental retardation, retinitis pigmentosa OMIM PubMed AFG3L2 NM_006796.2 98% Spinocerebellar ataxia 28 OMIM Ataxia, spastic, 5, autosomal recessive OMIM AGK NM_018238.3 100% Sengers syndrome OMIM AIFM1 NM_004208.3 100% Cowchock syndrome OMIM Combined oxidative phosphorylation deficiency 6 OMIM Spondyloepimetaphyseal dysplasia with neurodegeneration PubMed ANO10 NM_018075.3 100% Spinocerebellar ataxia, autosomal recessive 10 OMIM APOPT1 NM_032374.4 100% Mitochondrial complex IV deficiency OMIM APTX NM_175073.2 94% Ataxia, early-onset, with oculomotor apraxia and hypoalbuminemia OMIM ATP5A1 NM_001001937.1 98% Mitochondrial complex (ATP synthase) deficiency, nuclear type 4 OMIM Combined oxidative phosphorylation deficiency 22 OMIM ATP5E NM_006886.3 -

BCS1L Gene BCS1 Homolog, Ubiquinol-Cytochrome C Reductase Complex Chaperone
BCS1L gene BCS1 homolog, ubiquinol-cytochrome c reductase complex chaperone Normal Function The BCS1L gene provides instructions for making a protein that functions in cell structures called mitochondria, which convert the energy from food into a form that cells can use. The BCS1L protein is critical for the formation of a group of proteins known as complex III. Specifically, BCS1L adds a component called Rieske Fe/S protein to the complex. In mitochondria, complex III performs one step of the multistep process known as oxidative phosphorylation, in which oxygen and simple sugars are used to create adenosine triphosphate (ATP), the cell's main energy source. As a byproduct of its action in oxidative phosphorylation, complex III produces reactive oxygen species, which are harmful molecules that can damage DNA and tissues. The reactive oxygen species produced by complex III are thought to also play a role in normal cell signaling, particularly when levels of oxygen in the body are low (hypoxia). Some researchers believe the BCS1L protein is involved in the breakdown (metabolism) of iron, although the mechanism is unknown. Health Conditions Related to Genetic Changes Björnstad syndrome At least six BCS1L gene mutations have been found to cause Björnstad syndrome, a condition characterized by a hair abnormality known as pili torti (or "twisted hair") and hearing loss. BCS1L gene mutations associated with this condition alter the BCS1L protein and impair its ability to interact with other proteins. These changes reduce BCS1L's ability to add the Rieske Fe/S protein to complex III. As a result, complex III is incomplete, and excess Rieske Fe/S protein builds up in mitochondria. -
MOLECULAR GENETICS of the GRACILE SYNDROME (Growth Retardation, Aminoaciduria, Cholestasis, Iron Overload, Lactacidosis and Early Death)
CORE Metadata, citation and similar papers at core.ac.uk Provided by Helsingin yliopiston digitaalinen arkisto MOLECULAR GENETICS OF THE GRACILE SYNDROME (Growth Retardation, Aminoaciduria, Cholestasis, Iron overload, Lactacidosis and Early death) Ilona Visapää Department of Molecular Medicine, National Public Health Institute and Department of Medical Genetics, University of Helsinki, Helsinki, Finland, and Department of Human Genetics, David Geffen School of Medicine at UCLA, Los Angeles, California, USA, and Hospital for Children and Adolescents, Helsinki University Central Hospital, Helsinki, Finland. Academic Dissertation Helsinki University Biomedical Dissertations No. 19 Helsinki Biomedical Graduate School To be publicly discussed with permission of the Medical Faculty of the University of Helsinki, in auditorium 2 of the Biomedicum Helsinki, Haartmaninkatu 8, on December 5th, 2002, at 12 noon. Helsinki 2002 Supervised by Professor Leena Peltonen-Palotie National Public Health Institute and University of Helsinki, Helsinki, Finland and David Geffen School of Medicine at UCLA, Los Angeles, California, USA Reviewed by Professor Pertti Aula University of Helsinki Helsinki, Finland Docent Kirsi Huoponen University of Turku Turku, Finland Copyright National Public Health Institute Julkaisija – Utgivare – Publisher Kansanterveyslaitos Mannerheimintie 166 00300 Helsinki Puh. vaihde (09) 47441, telefax (09) 4744 8408 Folkhälsoinstitutet Mannerheimvägen 166 00300 Helsingfors Tel. växel (09) 47441, telefax (09) 4744 8408 National Public Health Institute Mannerheimintie 166 FIN-00300 Helsinki, Finland Telephone +358 9 47441, telefax +358 9 4744 8408 Publications of the National Public Health Institute, KTL A28/2002 ISBN 951-740-323-2 (Paperback) ISBN 951-740-324-0 (PDF) ISSN 0359-3584 (printed versions) ISSN 1458-6290 (electronic versions) Helsinki University Biomedical Dissertations No. -

33 Disorders of Copper, Zinc, and Iron Metabolism Eve A
33 Disorders of Copper, Zinc, and Iron Metabolism Eve A. Roberts 33.1 Introduction Metabolic diseases associated with abnormal disposition of metals are generally rare, with the exception of hereditary hemochromatosis (HFE1) in northern European populations. They are highly disparate disorders. I 33.1 Wilson disease Wilson disease (hepatolenticular degeneration) is an autosomal recessive dis- order of copper disposition in the liver and certain other organs, notably the brain, kidneys, mammary glands, and placenta. It is associated with copper overload in the liver and secondary accumulation of copper in certain parts of the brain, cornea (Kaiser-Fleischer ring), and in the kidneys, heart, and synovia. Wilson disease can present as liver disease, progressive neurological disease, or psychiatric illness (Roberts and Schilsky 2003). The hepatic presentation usually occurs at younger ages. Wilson disease is fatal if not treated, but with ef- fective treatment, especially if commenced early (ideally in the presymptomatic stage), the outlook for a normal healthy life is excellent. If a specific treatment must be discontinued because of adverse side-effects, alternate treatment must be substituted. Treatment should be continued through pregnancy. Dietary management by itself is inadequate, but foods containing very high concen- trations of copper (shellfish, nuts, chocolate, mushrooms, and organ meats) should be avoided, especially in the 1st year of treatment. Liver transplantation is indicated for patients unresponsive to medical treatment and for those with fulminant hepatic failure. I 33.2 Menkes disease Menkes disease is a rare (1:250,000) complex disorder of copper disposition leading to systemic copper insufficiency. The major features of Menkes disease involve neurodegeneration, vascular (usually arterial) abnormalities, and ab- normal hair structure (pili torti: occasioning the disease’s alternative name of “kinky hair” syndrome). -

Bruce H. Cohen, MD Page 1 of 56
CURRICULUM VITAE PERSONAL INFORMATION Bruce H. Cohen, MD, FAAN Director; NeuroDevelopmental Science Center, Children’s Hospital Medical Center of Akron Division of Neurology, Children’s Hospital Medical Center of Akron Professor of Pediatrics, Northeast Ohio College of Medicine Place of Birth: St. Louis, Missouri, USA Citizenship: United States EDUCATION Undergraduate: Washington University Lindel and Skinker Blvd., St. Louis, MO 63105 A.B., Chemistry, Summa Cum Laude and Sigma Xi September 1974-June 1978 Medical School: Albert Einstein College of Medicine of Yeshiva University 13oo Morris Park Avenue Bronx, NY 10461 POST-GRADUATE TRAINING Pediatric Residency: Children’s Hospital of Philadelphia 34th and Civic Center Blvd., Philadelphia, PA 19104 June 17, 1982 - June 30, 1984 Pediatric Neurology Residency Neurological Institute of New York and Babies Hospital Columbia Presbyterian Medical Center 630 West 168th Street New York, NY 10032 July 1, 1984 - June 30, 1987 Pediatric Neuro-Oncology Fellowship: Children’s Hospital of Philadelphia 34th and Civic Center Blvd., Philadelphia, PA 19104 July 1, 1987 - May 31, 1989 CONTACT INFORMATION Office Address: Akron Children’s Hospital 215 W. Bowery Street, 4th Floor, Akron, OH 44308 Office Phone: 330/543-6048, 330/543-6037 Facsimile: 330/543-6045 PROFESSIONAL APPOINTMENTS Children’s Hospital Medical Center of Akron; Director of the Neurodevelopmental Science Center 2015 – present Children’s Hospital Medical Center of Akron; Interim Vice-President and Medical Director of the Rebecca D. Considine Research Institute 2019 - present Children’s Hospital Medical Center of Akron; Interim Director of the Neurodevelopmental Science Center 2014-2015 Children’s Hospital Medical Center of Akron; Director of Neurology, 2010 - 2016 Professor of Pediatrics; Tenure Track, Northeast Ohio Medical University, 2011-current Professor of Integrative Medical Sciences, Tenure Track, Northeast Ohio Medical University, 2019 - current Akron General Hospital; Department of Neurology Staff, 2014 – current Bruce H. -
Renal Manifestations of Primary Mitochondrial Disorders (Review)
BIOMEDICAL REPORTS 6: 487-494, 2017 Renal manifestations of primary mitochondrial disorders (Review) JOSEF FINSTERER1* and FULVIO SCORZA2* 1Neurological Department, Municipal Hospital Rudolfstiftung, A‑1030 Vienna, Austria; 2Paulista de Medicina School, Federal University of São Paulo, Primeiro Andar CEP, São Paulo 04039‑032, SP, Brazil Received February 8, 2017; Accepted March 31, 2017 DOI: 10.3892/br.2017.892 Abstract. The aim of the present review was to summarize hereditary optic neuropathy, coenzyme‑Q deficiency, X‑linked and discuss previous findings concerning renal manifesta- sideroblastic anemia and ataxia, myopathy, lactic acidosis, tions of primary mitochondrial disorders (MIDs). A literature and sideroblastic anemia, pyruvate dehydrogenase deficiency, review was performed using frequently used databases. The growth retardation, aminoaciduria, cholestasis, iron overload, study identified that primary MIDs frequently present as mito- lactacidosis, and early death, and hyperuricemia, pulmonary chondrial multiorgan disorder syndrome (MIMODS) at onset hypertension, renal failure in infancy and alkalosis syndrome. or in the later course of the MID. Occasionally, the kidneys The present study proposes that the frequency of renal involve- are affected in MIDs. Renal manifestations of MIDs include ment in MIDs is probably underestimated. Diagnosis of renal renal insufficiency, nephrolithiasis, nephrotic syndrome, renal involvement follows general guidelines and treatment is symp- cysts, renal tubular acidosis, Bartter‑like syndrome,