A Matter of Life and Healthy Life
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Agenda Annex
FORM 2 SHEFFIELD CITY COUNCILAgenda Annex Full Council Report of: Chief Executive ________________________________________________________________ Report to: Council ________________________________________________________________ Date: 4th March 2016 ________________________________________________________________ Subject: Polling District and Polling Place Review ________________________________________________________________ Author of Report: John Tomlinson 27 34091 ________________________________________________________________ Summary: Following the recent ward boundary changes the Authority is required to allocate Polling Districts and Polling Places. ________________________________________________________________ Reasons for Recommendations: The recommendations have been made dependent on the following criteria: 1. All polling districts must fall entirely within all Electoral areas is serves 2. A polling station should not have more than 2,500 electors allocated to it. ________________________________________________________________ Recommendations: The changes to polling district and polling place boundaries for Sheffield as set out in this report are approved. ________________________________________________________________ Background Papers: None Category of Report: OPEN Form 2 – Executive Report Page 1 January 2014 Statutory and Council Policy Checklist Financial Implications YES Cleared by: Pauline Wood Legal Implications YES Cleared by: Gillian Duckworth Equality of Opportunity Implications NO Cleared by: Tackling Health -

Sheffield Street Tree Strategy Development Group
Sheffield Street Tree Strategy Development Group i-Tree Eco Stratified Inventory Report November 2019 The Authors James Watson - Treeconomics Reviewed By: Danielle Hill - Treeconomics This assessment was carried out by Treeconomics 1 Executive Summary In this report, the street trees in Sheffield have been assessed based on the benefits that they provide to society. These trees, which form part of Sheffield’s natural capital, are generally recognised and appreciated for their amenity, presence and stature in the cityscape and surroundings. However, society is often unaware of the many other benefits (or ecosystem services) that trees provide to those living in our towns and cities. The trees in and around our urban areas (together with woodlands, shrubs, hedges, open grass, green space and wetland) are collectively known as the ‘urban forest’. This urban forest improves our air, protects watercourses, saves energy, and improves economic sustainability1. There are also many health and well-being benefits associated with being in close proximity to trees and there is a growing research base to support this2. Sheffield’s street trees are a crucial part of the city’s urban forest, rural areas and woodlands. Many of the benefits that Sheffield’s urban forest provides are offered through its street trees. Economic valuation of the benefits provided by our natural capital3 (including the urban forest) can help to mitigate for development impacts, inform land use changes and reduce any potential impact through planned intervention to avoid a net loss of natural capital. Such information can be used to help make better management decisions. Yet, as the benefits provided by such natural capital are often poorly understood, they are often undervalued in the decision making process. -

Arbourthorne Ward 2012 Local Election Result Results for the Arbourthorne Ward 2012 Local Election
Sheffield City Council - Arbourthorne Ward 2012 Local Electio... hps://www.sheffield.gov.uk/your-city-council/elections/electio... You are here: Home : Your City Council : Elections : Election Results : 2012 : Arbourthorne Arbourthorne Ward 2012 Local Election Result Results for the Arbourthorne Ward 2012 Local Election. Labour hold the seat Jennyfer Marie Andrea Barnard, Green Party. Votes: 276 Julie Dore. Labour Party. Votes: 2303 Allan David Sheridan, UK Independence Party (UK I P). Votes: 544 Peter Smith, The Conservative Party. Votes: 299 Patricia White, Liberal Democrat. Votes: 275 Electorate: 13116 Turnout: 28.18% Powered by Translate Urdu Translation Modified: May 4, 2012 1:42:30 PM 1 of 1 10/05/2012 20:06 Sheffield City Council - Beauchief and Greenhill Ward 2012 Loc... hps://www.sheffield.gov.uk/your-city-council/elections/electio... You are here: Home : Your City Council : Elections : Election Results : 2012 : Beauchief and Greenhill Beauchief and Greenhill Ward 2012 Local Election Result Results for the Beauchief and Greenhill Ward 2012 Local Election. Labour gain the seat Steve Ayris, Liberal Democrat. Votes: 1642 Peter Boardman, UK Independence Party (UK I P). Votes: 534 Michelle Lesley Grant, The Conservative Party. Votes: 345 Christina Hespe, Green Party. Votes: 296 Roy Munn, Labour Party. Votes: 2393 Electorate: 13969 Turnout: 38.14% Powered by Translate Urdu Translation Modified: May 4, 2012 12:33:42 PM 1 of 1 10/05/2012 20:07 Sheffield City Council - Beighton Ward 2012 Local Election Result hps://www.sheffield.gov.uk/your-city-council/elections/electio... You are here: Home : Your City Council : Elections : Election Results : 2012 : Beighton Beighton Ward 2012 Local Election Result Results for the Beighton Ward 2012 Local Election. -

Neighbourhoods Update Page 13 Page Nicki Doherty Director of Delivery Care Outside of Hospital + Dr Anthony Gore Clinical Director Care Outside of Hospital
Neighbourhoods Update Page 13 Nicki Doherty Director of Delivery Care Outside of Hospital + Dr Anthony Gore Clinical Director Care Outside of Hospital NHS Sheffield CCG Agenda Item 7 Page 14 What is a Neighbourhood.. a geographical population of around 30-50,000 people Page 15 supported by joined up health, social, voluntary sector and wider services to support people to remain independent , safe and well in their community. Why Neighbourhoods? • General Practice at Scale Page 16 • Wider integrated working across the health and social care system • Targeting Care to priority patient groups • Managing Resources • Empowering Neighbourhoods 16 Neighbourhoods Across Sheffield 4 in Central City 4 in Hallam & South High Green 3 in North 5 in West Upper Don Valley SAPA - North2 - West4 North2 Darnall - Peak Edge GPA1 - SSHG Dovercourt Surgery 70 GPA1 Duke Medical Centre 29 West 6 Hillsborough East Bank Medical Centre 68 Manor Park Medical Centre 67 Townships II Norfolk Park Medical Practice 56 - Hillsborough Park Health Centre 18 - Upper Don Valley Student Page 17 White House Surgery 39 Porter Valley North 2 Townships I Burngreave Surgery 12 - Porter Valley Dunninc Road Surgery 48 City Centre Carrfield Firth Park Surgery 25 SSHG Page Hall Medical Centre 9 Pitsmoor Surgery 58 Sheffield Medical Centre 62 Peak Edge Carrfield Shiregreen Medical Centre 82 Carrfield Medical Centre 73 The Flowers Health Centre 27 Gleadless Medical Centre 40 Upwell Street Surgery 32 Upper Don Valley SAPA Heeley Green Surgery 80 Wincobank Medical Centre 13 Deepcar Medical -
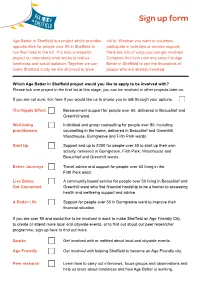
Sign up Form
Sign up form Age Better in Sheffield is a project which provides old in. Whether you want to volunteer, opportunities for people over 50 in Sheffield to participate in activities or receive support, live their lives to the full. It is also a research there are lots of ways you can get involved. project to understand what works to reduce Complete this form now and send it to Age loneliness and social isolation. Together we can Better in Sheffield to join the thousands of make Sheffield a city we are all proud to grow people who are already involved. Which Age Better in Sheffield project would you like to apply to be involved with? Please tick one project in the first list at this stage, you can be involved in other projects later on. If you are not sure, tick here if you would like us to phone you to talk through your options. The Ripple Effect Bereavement support for people over 50, delivered in Beauchief and Greenhill ward. Well-being Individual and group counselling for people over 50, including practitioners counselling in the home, delivered in Beauchief and Greenhill, Woodhouse, Burngreave and Firth Park wards. Start Up Support and up to £200 for people over 50 to start up their own activity, delivered in Burngreave, Firth Park, Woodhouse and Beauchief and Greenhill wards. Better Journeys Travel advice and support for people over 50 living in the Firth Park ward. Live Better, A community based service for people over 50 living in Beauchief and Get Connected Greenhill ward who find financial hardship to be a barrier to accessing health and wellbeing support and advice. -

Christ Church Dore Newsletter May 2020
Christ Church Dore Newsletter May 2020 Walking Group Church Newsletter April 2020 The doors were locked, but Jesus came and stood among them and He said ‘Peace be We hope you are all well and, if allowed, are finding with you’. opportunities to perhaps do some walking? We are fortunate and are still able to enjoy a walk most John Chapter 20 v26 days but appreciate not everyone is in the same situation. For us an unexpected benefit of the current situation is that we have been exploring lots of the less used tracks around and across Blacka Moor, Totley Moor and Houndkirk Moor. We’ve plenty of ideas for new walks within a 5 minutes car journey from church, once lockdown is lifted! Another benefit has been paying much more attention to the progress of spring than usual. The woods are just bursting with life and it is great to hear in the church service chat rooms people swapping details of where to walk to find the best bluebells! With our love Online services every Sunday – check your emails and church web site for Hazel and David Sunday and mid week services. Previous online services are available on the church website. http://www.dorechurch.org.uk/services/ virtual-church-service In this period of lock down, days may seem the same but do not miss Friday 8th May is the 75th Anniversary of VE Day Thursday 21st May is Ascension Day Sunday 31st May is Pentecost 1 Signs of hope and thanks seen in and around Dore and Totley Do all the good you can. -

Agenda Item 3
Agenda Item 3 Minutes of the Meeting of the Council of the City of Sheffield held in the Council Chamber, Town Hall, Pinstone Street, Sheffield S1 2HH, on Wednesday 5 December 2012, at 2.00 pm, pursuant to notice duly given and Summonses duly served. PRESENT THE LORD MAYOR (Councillor John Campbell) THE DEPUTY LORD MAYOR (Councillor Vickie Priestley) 1 Arbourthorne Ward 10 Dore & Totley Ward 19 Mosborough Ward Julie Dore Keith Hill David Barker John Robson Joe Otten Isobel Bowler Jack Scott Colin Ross Tony Downing 2 Beauchiefl Greenhill Ward 11 East Ecclesfield Ward 20 Nether Edge Ward Simon Clement-Jones Garry Weatherall Anders Hanson Clive Skelton Steve Wilson Nikki Bond Roy Munn Joyce Wright 3 Beighton Ward 12 Ecclesall Ward 21 Richmond Ward Chris Rosling-Josephs Roger Davison John Campbell Ian Saunders Diana Stimely Martin Lawton Penny Baker Lynn Rooney 4 Birley Ward 13 Firth Park Ward 22 Shiregreen & Brightside Ward Denise Fox Alan Law Sioned-Mair Richards Bryan Lodge Chris Weldon Peter Price Karen McGowan Shelia Constance Peter Rippon 5 Broomhill Ward 14 Fulwood Ward 23 Southey Ward Shaffaq Mohammed Andrew Sangar Leigh Bramall Stuart Wattam Janice Sidebottom Tony Damms Jayne Dunn Sue Alston Gill Furniss 6 Burngreave Ward 15 Gleadless Valley Ward 24 Stannington Ward Jackie Drayton Cate McDonald David Baker Ibrar Hussain Tim Rippon Vickie Priestley Talib Hussain Steve Jones Katie Condliffe 7 Central Ward 16 Graves Park Ward 25 Stockbridge & Upper Don Ward Jillian Creasy Ian Auckland Alison Brelsford Mohammad Maroof Bob McCann Philip Wood Robert Murphy Richard Crowther 8 Crookes Ward 17 Hillsborough Ward 26 Walkey Ward Sylvia Anginotti Janet Bragg Ben Curran Geoff Smith Bob Johnson Nikki Sharpe Rob Frost George Lindars-Hammond Neale Gibson 9 Darnall Ward 18 Manor Castle Ward 27 West Ecclesfield Ward Harry Harpham Jenny Armstrong Trevor Bagshaw Mazher Iqbal Terry Fox Alf Meade Mary Lea Pat Midgley Adam Hurst 28 Woodhouse Ward Mick Rooney Jackie Satur Page 5 Page 6 Council 5.12.2012 1. -

Sheffield City Council Place Report to West and North
SHEFFIELD CITY COUNCIL PLACE REPORT TO WEST AND NORTH PLANNING AND DATE 31/08/2010 HIGHWAYS COMMITTEE REPORT OF DIRECTOR OF DEVELOPMENT SERVICES ITEM SUBJECT APPLICATIONS UNDER VARIOUS ACTS/REGULATIONS SUMMARY RECOMMENDATIONS SEE RECOMMENDATIONS HEREIN THE BACKGROUND PAPERS ARE IN THE FILES IN RESPECT OF THE PLANNING APPLICATIONS NUMBERED. FINANCIAL IMPLICATIONS N/A PARAGRAPHS CLEARED BY BACKGROUND PAPERS CONTACT POINT FOR ACCESS Vernon Faulkner TEL 0114 2734183 NO: AREA(S) AFFECTED CATEGORY OF REPORT OPEN 2 Application No. Location Page No. 10/02474/FUL 488 Redmires Road Sheffield 6 S10 4LG 10/02434/FUL Ewden Barn Bank Lane 12 Sheffield S36 3ZL 10/02110/FUL Chestnut Grove Curtilage Of 485 Loxley Road 18 Sheffield S6 6RP 10/01805/FUL 5 St Mark Road Sheffield 33 S36 2TF 10/01530/RG3 Land Between Buckenham Street Clun Street And 41 Ellesmere Road Sheffield 10/01372/FUL Storrs Farm, Storrs Lane And Broad Oak, Stopes Road 64 Sheffield S6 6GY 10/01225/FUL Site Of Clinical Psychology Unit Northern General Hospital 73 Herries Road Sheffield S5 7AU 10/01128/FUL 69 Norwood Road Sheffield 87 S5 7BP 3 10/01017/CHU 261 Ellesmere Road North And 163 Scott Road Sheffield 99 S4 7DP 4 5 SHEFFIELD CITY COUNCIL Report Of The Head Of Planning, Transport And Highways, Development, Environment And Leisure To The NORTH & WEST Planning And Highways Area Board Date Of Meeting: 31/08/2010 LIST OF PLANNING APPLICATIONS FOR DECISION OR INFORMATION *NOTE* Under the heading “Representations” a Brief Summary of Representations received up to a week before the Area Board date is given (later representations will be reported verbally). -

Beauchief & Greenhill to Dore & Totley(PDF)
LCg 275 TAb 64 Leeshall Wood LF 2,654 PE 1,837 LF 2,654 PE 1,837 LEb 95 LEb 95 BeauchiefLi ttale Cnomdm onGreenhill Ward: Lib Dem Proposed Boundary (4th August 2014) LCc 721 OC 1,497 LCc 721 PA 2,052 PA 2,052 Gleadless Valley Ward PG 2,273 PG 2,273 0.48% OC 1,497 14,921 Millhouses ¯ LCd 0 PF 2,209 PF 2,209 Ecclesall Ward Hemsworth 8.14% 16,058 LEc 2,534 LEc 2,534 LEa 2 LEa 2 Hutcliff Wood Abbey Dale Bolehill Backmoor PCb 2,525 PCb 2,525 OE 2,059 OEb 538 PCa 420 PCa 420 OEa 1,521 Graves Park Ward Ecclesall Wood -2.24% 14,517 Summerhouse Wood Abbeydale BC 1,387 BC 1,387 JEa 1,286 JEa 1,286 LEd 413 LEd 413 Meadow Head Cobnar Wood PD 1,140 PD 1,140 BB 836 BB 836 PB 1,541 PB 1,541 Little Norton Norton Parkbank Wood Broomfield Wood BD 2,170 BD 2,170 Ladies' Spring Wood Beauchief and Greenhill Ward -1.87% BE 2,445 BE 2,445 Greenhill 14,572 JA 3,290 JA 3,290 Hazlebarrow Farm Nether Wood Jordanthorpe BA 3,018 BA 3,018 Twentywellsick Wood BF 1,489 BF 1,489 BGc 168 BGc 168 Long Wood Batemoor Bradway Bank Lower Bradway BGb 25 BGb 25 Dore and Totley Ward JBb 2,609 JBb 2,609 2.89% BGa 2,394 BGa 2,394 Nor Wood 15,280 Lowedges Totley Rise Upper Bradway JBa 547 JBa 547 Bradway The Dore And Totley Golf Course Scale: 1:6,090 Proposed Ward Boundary Bowshaw Farm Sheffield City Council Policy, Performance & Communications Tel: (0114) 2930239 Proposed Polling Districts © Crown copyright and database rights 2014 Ordnance Survey 100018816 Performance & Research Team ZA 734 ZCa 108 EDb 526 ZA 734 EDb 526 EDb 526 Steel Bank EDb 526 ZI 1,852 ZI 1,852 ZGb 450 ZGb -

On the Disturbances in the District of the Valley of The
Downloaded from http://pygs.lyellcollection.org/ by guest on September 28, 2021 mittee, for their kind assistance in making the arrangements for the meeting. The following communications were then made to the Society :— ON THE DISTURBANCES IN THE DISTRICT OP THE VALLEY OF THE DON. BY REV. WM. THORP, OF WOMERSLEY. Upon the last visit of the Society to Sheffield, I had the pleasure of describing some of the geological features of the neighbouring district, and particularly those of the country between Rotherham and Sheffield. I have again taken the liberty of giving a brief mining notice of the disturbances of the same district, because they are not only of such enor mous magnitude as to be of great interest to the geologist, but a knowledge of them is necessary to the successful min ing operations of that neighbourhood. Upon the former occasion, it was contended by one party that not only were the strata on the North side of the Don elevated above those of the South side, to the amount of 600 yards in vertical height; but that also there had been a horizontal lateral movement of the beds of the North side, in an eastward direction, to the length of five or six miles.^ * The proofs then adduced in support of a lateral movement were—1. That the various beds come from the North, up to the edge of the valley of the Don, but do not preserve their Northerly and Southerly direction across the valley, but are found several miles to the West; e. g.^the Silkstone coal ranges to Dropping Well, near Kimberworth, and is not found at the same depth until we arrive six miles West, at SheflSeld town. -

(25) Manor Park Sheffield He
Bus service(s) 24 25 Valid from: 18 July 2021 Areas served Places on the route Woodhouse Heeley Retail Park Stradbroke Richmond (25) Moor Market Manor Park SHU City Campus Sheffield Heeley Woodseats Meadowhead Lowedges Bradway What’s changed Service 24/25 (First) - Timetable changes. Service 25 (Stagecoach) - Timetable changes. Operator(s) Some journeys operated with financial support from South Yorkshire Passenger Transport Executive How can I get more information? TravelSouthYorkshire @TSYalerts 01709 51 51 51 Bus route map for services 24 and 25 26/05/2016# Catclie Ð Atterclie Rivelin Darnall Waverley Crookes Sheeld, Arundel Gate Treeton Ð Crosspool Park Hill Manor, Castlebeck Av/Prince of Wales Rd Ð Sheeld, Arundel Gate/ Broomhill Ð SHU City Campus Sandygate Manor, Castlebeck Av/Castlebeck Croft Sheeld, Fitzwilliam Gate/Moor Mkt Ð Manor Park, Manor Park Centre/ Ð Harborough Av 24 Nether Green Hunters Bar Sharrow Lowfield, Woodhouse, Queens Rd/ 25 Cross St/ Retail Park Tannery St Fulwood Greystones 24, 25 Nether Edge 24 25 High Storrs 25 Richmond, Heeley, Chesterfield Rd/Beeton Rd Hastilar Rd South/ 25 Richmond Rd Heeley, Chesterfield Rd/Heeley Retail Park Woodhouse, Woodhouse, Gleadless Stradbroke Rd/ Skelton Ln/ Ringinglow Sheeld Rd Skelton Grove Beighton Gleadless Valley Hackenthorpe Millhouses Norton Lees Birley Woodseats, Chesterfield Rd/Woodseats Library Herdings Charnock Owlthorpe Waterthorpe Woodseats, Chesterfield Rd/Bromwich Rd Abbeydale Beauchief High Lane Norton 24, 25 Westfield database right 2016 Dore 25 Abbeydale Park Mosborough and Greenhill Ridgeway yright p o c Halfway own 24, 25 r C Bradway, Prospect Rd/Everard Av data © 24 25 24 y e 24 v Sur e Lowedges, Lowedges Rd/The Grennel Mower c dnan Bradway, Longford Rd r O Totley Apperknowle Marsh Lane Eckington ontains C 6 = Terminus point = Public transport = Shopping area = Bus route & stops = Rail line & station = Tram route & stop Hail & ride Along part of the route you can stop the bus at any safe and convenient point - but please avoid parked vehicles and road junctions. -

Burngreave & Fir Vale
Burngreave & Fir Vale Summary of Evaluation Work SECTION ONE - BACKGROUND Burngreave and Firvale Sure Start programme was agreed December 2000. Staff were in post April 2001 services were delivered May/June 2001. AREA DESCRIPTION The Burngreave and Firvale Sure Start area is diverse and encompasses a range of different languages, cultures and religions. There is a transient population within the area which includes two Mother and Baby Units that take parents from outside of Sheffield and two Women’s Refuges. The area also houses the largest asylum seeking population in Sheffield. The area is a ‘New Deal For Communities’ area and is therefore seeing much regeneration. There are many new projects and schemes springing up, all seeking to recruit new workers and involve local people. The area suffers from poor media coverage due to gun crime and a drugs culture. The area has a negative image and services are struggling to recruit to the area. Since 2002 Burngreave and Firvale Sure Start programme has never been fully staffed and we have had to have agency staff for a number of services. Other services such as health services and New Deal are struggling to recruit to the area. The area is seen as a difficult area to work.. Burngreave and Firvale Sure Start programme is the largest in Sheffield being approved with 1049 under 4’s at the time - numbers are presently 1150. Although it is the largest programme in the city, Burngreave and Firvale Sure Start does not have the largest revenue budget or get the same amount of funding per child as other Sure Start programmes in the city.