Legislative Update
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

House Committee on Energy and Environment
HOUSE COMMITTEE ON ENERGY AND ENVIRONMENT February 6, 2020 Hearing Room D 01:00 PM MEMBERS PRESENT: Rep. Karin Power, Chair Rep. Daniel Bonham, Vice-Chair Rep. Janeen Sollman, Vice-Chair Rep. Ken Helm Rep. E. Werner Reschke Rep. Andrea Salinas Rep. Sheri Schouten Rep. David Brock Smith Rep. Marty Wilde STAFF PRESENT: Beth Reiley, LPRO Analyst Isabel Hernandez, Committee Assistant EXHIBITS: Exhibits from this meeting are available here MEASURES/ISSUES: HB 4093 – Public Hearing HB 4024 – Public Hearing HB 4049 – Public Hearing 00:00:08 Meeting Called to Order 00:00:09 Chair Power 00:00:20 HB 4093 - Public Hearing 00:00:21 Chair Power 00:00:22 EXHIBIT 1: witness registration 00:00:44 Rep. Vikki Breese-Iverson, House District 55 00:02:13 Rep. Mark Owens, House District 60 00:06:00 EXHIBIT 2-3: Matt Krumenauer, Vice President, Special Projects, U.S. Endowment for Forestry and Communities, Inc. 00:09:16 Bruce Daucsavage, Malheur Lumber Co. 00:13:14 Rep. Reschke 00:16:20 EXHIBIT 4: Annalisa Bhatia, Senior Legislative Advisor, Oregon Department of Environmental Quality 00:21:53 Rep. Wilde 00:25:30 Vice-Chair Bonham 00:26:22 Vice-Chair Sollman 00:30:26 Rep. Helm 00:32:00 EXHIBIT 5: Mike Eliason, General Counsel & Director of Government Affairs, Oregon Forest & Industries Council This recording log is in compliance with Senate and House Rules. For complete contents, refer to the digital audio recording. HEE 02/06/2020 Page 2 of 4 00:34:59 Dylan Kruse, Director of Government Affairs, Sustainable Northwest 00:38:59 Kristan Mitchell, Executive Director, Oregon Refuse and Recycling Association 00:47:53 The following is submitted for the record without public testimony: EXHIBIT 6: Alison Briggs-Ungerer, Chair, Association of Oregon Recyclers EXHIBIT 7: Carlton Owen, President and CEO, U.S. -

BIPOC Caucus Condemns Passage of Texas Abortion
PRESS RELEASE OREGON HOUSE DEMOCRATS For Immediate Release For more information, Contact: Sep. 2, 2021 Hannah Kurowski: [email protected] CORRECTION: BIPOC Caucus Condemns Passage of SB 8, Calls for Protection of Abortion as Essential Health Care CORRECTION The following members of the BIPOC Caucus sign onto this statement: • Senators: Lew Frederick, Kayse Jama, James Manning • Representatives: Teresa Alonso Leon, Wlnsvey Campos, Andrea Valderrama, Mark Meek, Khanh Pham, Ricki Ruiz, Andrea Salinas, Tawna Sanchez SALEM, OR -- The Legislative Black, Indigenous, People of Color (BIPOC) Caucus released the following statement after the Texas Governor signed into law Senate Bill 8 (SB 8) to ban abortions after six weeks, as well as encourages private citizens to act as bounty hunters: “Roe vs Wade enshrined reproductive health care as a constitutionally protected right. In Oregon, we have a long history of protecting reproductive rights and removing barriers to accessing abortion because we know abortion is healthcare. "If SB 8 remains in effect without intervention from courts, any abortion providers who remain operational are facing a crushing wave of lawsuits that they will likely be unable to litigate. This back-door ban presents harm to people facing severe restrictions on important health care protections. "BIPOC communities are most often forced to resort to unsafe abortions due to reproductive healthcare restrictions, a symptom of institutionalized white supremacy and patriarchy. SB 8 once again disproportionately takes away our constitutional right to make decisions about our own bodies as a worst case scenario, and forces those with the resources to travel across state lines for healthcare access as a best case scenario. -
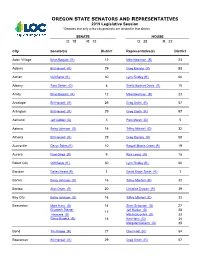
OREGON STATE SENATORS and REPRESENTATIVES 2019 Legislative Session * Denotes That Only a Few City Precincts Are Located in That District
OREGON STATE SENATORS AND REPRESENTATIVES 2019 Legislative Session * Denotes that only a few city precincts are located in that district SENATE HOUSE D: 18 R: 12 D: 38 R: 22 City Senator(s) District Representative(s) District Adair Village Brian Boquist (R) 12 Mike Nearman (R) 23 Adams Bill Hansell (R) 29 Greg Barreto (R) 58 Adrian Cliff Bentz (R ) 30 Lynn Findley (R) 60 Albany Sara Gelser (D) 8 Shelly Boshart Davis (R) 15 Amity Brian Boquist (R) 12 Mike Nearman (R) 23 Antelope Bill Hansell (R) 29 Greg Smith (R) 57 Arlington Bill Hansell (R) 29 Greg Smith (R) 57 Ashland Jeff Golden (D) 3 Pam Marsh (D) 5 Astoria Betsy Johnson (D) 16 Tiffiny Mitchell (D) 32 Athena Bill Hansell (R) 29 Greg Barreto (R) 58 Aumsville Denyc Boles (R) 10 Raquel Moore-Green (R) 19 Aurora Fred Girod (R) 9 Rick Lewis (R) 18 Baker City Cliff Bentz (R ) 30 Lynn Findley (R) 60 Bandon Dallas Heard (R) 1 David Brock Smith (R) 1 Banks Betsy Johnson (D) 16 Tiffiny Mitchell (D) 32 Barlow Alan Olsen (R) 20 Christine Drazan (R) 39 Bay City Betsy Johnson (D) 16 Tiffiny Mitchell (D) 32 Beaverton Mark Hass (D) 14 Sheri Schouten (D) 27 Elizabeth Steiner Jeff Barker (D) 28 17 Hayward (D) Mitch Greenlick (D) 33 Ginny Burdick (D) 18 Ken Helm (D) 34 Margaret Doherty (D) 35 Bend Tim Knopp (R) 27 Cheri Helt (R) 54 Boardman Bill Hansell (R) 29 Greg Smith (R) 57 City Senator(s) District Representative(s) District Bonanza Dennis Linthicum (R) 28 Werner Reschke (R) 56 Brookings Dallas Heard (R) 1 David Brock Smith (R) 1 Brownsville Lee Beyer (D) 6 Marty Wilde (D) 11 Burns Cliff Bentz (R ) 30 Lynn Findley (R) 60 Butte Falls Dennis Linthicum (R) 28 55 Vacant Seat Canby Alan Olsen (R) 20 Christine Drazan (R) 39 Cannon Beach Betsy Johnson (D) 16 Tiffiny Mitchell (D) 32 Canyon City Cliff Bentz (R ) 30 Lynn Findley (R) 60 Canyonville Dallas Heard (R) 1 Gary Leif (R) 2 Carlton Brian Boquist (R) 12 Ron Noble (R) 24 Cascade Locks Chuck Thomsen (R) 26 Anna Williams (D) 52 Cave Junction Herman Baertschiger Jr. -

House Committee on Energy and Environment
HOUSE COMMITTEE ON ENERGY AND ENVIRONMENT February 4, 2020 Hearing Room D 01:00 PM MEMBERS PRESENT: Rep. Karin Power, Chair Rep. Daniel Bonham, Vice-Chair Rep. Janeen Sollman, Vice-Chair Rep. Ken Helm Rep. E. Werner Reschke Rep. Andrea Salinas Rep. Sheri Schouten Rep. David Brock Smith Rep. Marty Wilde STAFF PRESENT: Beth Reiley, LPRO Analyst Isabel Hernandez, Committee Assistant EXHIBITS: Exhibits from this meeting are available here MEASURES/ISSUES: Organizational Meeting Adoption of Committee Rules HB 4066 – Public Hearing HB 4135 – Public Hearing HB 4067 – Public Hearing 00:00:27 Meeting Called to Order 00:00:28 Chair Power 00:00:36 Adoption of Committee Rules - Organizational Meeting 00:00:37 EXHIBIT 1: Chair Power 00:00:44 MOTION: VICE-CHAIR BONHAM MOVES ADOPTION OF COMMITTEE RULES 00:01:11 VOTE: 9-0-0 AYE: HELM, RESCHKE, SALINAS, SCHOUTEN, BROCK SMITH, WILDE, BONHAM, SOLLMAN, POWER 00:02:01 Rep. Marty Wilde, House District 11 00:02:13 Rep. Sheri Schouten, House District 27 00:02:18 Rep. E. Werner Reschke, House District 56 00:02:24 Rep. Janeen Sollman, House District 30 00:02:37 Rep. Andrea Salinas, House District 38 00:02:49 Rep. David Brock Smith, House District 1 00:02:59 Rep. Ken Helm, House District 34 This recording log is in compliance with Senate and House Rules. For complete contents, refer to the digital audio recording. HEE 02/04/2020 Page 2 of 4 00:03:16 Rep. Daniel Bonham, House District 59 00:03:41 Rep. Karin Power, House District 41 00:04:33 HB 4066 - Public Hearing 00:04:34 EXHIBIT 2: Chair Power 00:04:35 EXHIBIT 3: witness registration 00:05:06 Matt Donegan, Chair, Oregon Wildfire Response Council 00:10:07 Rep. -

Speaker Appointments to Interim Committees
Tina Kotek 900 Court Street NE Speaker of the House Salem, OR 97301 Oregon House of Representatives MEMORANDUM TO: Timothy G. Sekerak, Chief Clerk of the House FROM: Tina Kotek, Speaker of the House RE: Appointments – Interim Committees DATE: August 16, 2019 Effective immediately and pursuant to House Rule 8.05, I am making the following appointments: 2019-20 House Interim Standing Committees Agriculture and Land Use Committee Economic Development Committee Brian Clem, Chair John Lively, Chair Susan McLain, Vice-Chair Daniel Bonham, Vice-Chair Bill Post, Vice-Chair Julie Fahey, Vice-Chair Shelly Boshart Davis Greg Barreto David Brock Smith Christine Drazan Ken Helm Ken Helm Anna Williams Pam Marsh Caddy McKeown Susan McLain Kim Wallan Brad Witt Business and Labor Committee Education Committee Jeff Barker, Chair Margaret Doherty, Chair Greg Barreto, Vice-Chair Teresa Alonso Leon, Vice Chair Janelle Bynum, Vice-Chair Cheri Helt, Vice Chair Daniel Bonham Daniel Bonham Shelly Boshart Davis Diego Hernandez Vikki Breese-Iverson Courtney Neron Brian Clem Jeff Reardon Margaret Doherty Janeen Sollman Paul Evans Kim Wallan Julie Fahey Paul Holvey Veterans and Emergency Preparedness Energy and Environment Committee Committee Karin Power, Chair Paul Evans, Chair Janeen Sollman, Vice-Chair Rick Lewis, Vice-Chair E. Werner Reschke, Vice-Chair Mark Meek, Vice-Chair Lynn Findley Lynn Findley Ken Helm Courtney Neron Andrea Salinas Kim Wallan Sheri Schouten Marty Wilde Marty Wilde Jack Zika Jack Zika Health Care Committee Human Services and Housing Committee -

Today We Are Unified in Calling on Residents and Visitors to Our
Today we are unified in calling on residents and visitors to our respective communities to refrain from violence in the exercise of our First Amendment rights to free speech and to peaceably assemble. Black Lives Matter. Violence has no place in civic engagement and protest. Throughout 2020, and in too many years prior, we have born witness to instances of racial injustice, police brutality and the rise of white supremacist rhetoric throughout our country, and right here at home. Even now we are experiencing unhelpful and inflammatory comments and acts, from many quarters, including the highest office in the land. The overwhelming majority of our community who have risen to protest for social justice and against racial inequities have done so peacefully, in keeping with public health guidelines and within the bounds protected by our state and federal constitutions. Unfortunately, there are some individuals who have chosen violence over peaceful protest, violence towards other protestors, violence towards police officers and even an instance of deadly violence experienced recently in downtown Portland. While we recognize the outrage toward racial injustice is the foundation for the past 100+ days of protest, we call on everyone in our community seeking to confront racial injustice and to demand police accountability to forgo the path of violence. We invite every member of our respective communities to continue to engage with our governments, to hold us accountable and to contribute to and facilitate a transformation away from racist systems and towards a more equitable, just community. Similarly, we ask those who may want to demonstrate to do so peacefully and safely. -

1% 2% 4% 2% 29% 8% 5%
November 3, 2020 Election 8QR৽FLDO5HVXOWV Summary of City Measures Types of City Measures Results of City Measures 2% Bonds 2% 8% Annexation Other 4% 31% 29% Marijuana Charter Failed Amendments 71% Passed 29% Bonds 2% 5% Fees Gas Tax All Local Government Measures 1% Regional 14% RFPD/Fire 37% Districts Cities 14% Other Special Districts 16% School 18% Districts Counties All Measures by Local Governments Local Government Type Number of Measures Passed Failed Cities 38 71% 29% Counties 19 53% 47% School Districts/Community 17 82% 18% Colleges RFPD/Fire Districts 15 73% 27% Other Special Districts 14 71% 29% Regional 1 0% 100% Bond Measures by Local Governments Local Government Type Number of Bond Measures Passed Failed Cities 1 100% 0% Counties 1 100% 0% School Districts/Community 14 86% 14% Colleges RFPD/Fire Districts 1 100% 0% Other Special Districts 2 100% 0% Regional 0 N/A N/A Levy Measures by Local Governments Local Government Type Number of Levy Measures Passed Failed Cities 11 64% 36% Counties 2 0% 100% School Districts/Community 3 100% 0% Colleges RFPD/Fire Districts 8 75% 25% Other Special Districts 8 75% 25% Regional 0 N/A N/A Details of City Measures Banks Annexation Annexes 1.03 acres of continuous land to the City of Banks. Pass Yes No 585 67% 282 33% Bend Bond $190 Million; For traffic flow, East-West connections, neighborhood safety improvements. Pass Yes No 33,154 58% 23,847 42% Charter Charter Coquille Cove Amendment Amendment Amends charter to allow nomination of Adopts new charter for Cove city candidates by paying a fee as an government. -

Oregon Coalition of Local Health Officials 2021
OREGON COALITION OF LOCAL HEALTH OFFICIALS 2021 Legislative Toolkit – Senate and House Health Committees 2021 Senate Health Committee Membership Human Services, Mental Health and Recovery Meeting Times: 3:15pm, Tuesday and Thursday Sen. Sara Gelser, Chair Sen. Dick Anderson, Vice Chair Sen. Kate Lieber Sen. Art Robinson Sen. Kathleen Taylor Health Care Meeting Times: 1:00pm, Monday and Wednesday Sen. Deb Patterson, Chair Sen. Tim Knopp, Vice Chair Sen. James Manning, Jr. Sen. Dallas Heard Sen. Lee Beyer Joint Ways & Means Committee Sen. Betsy Johnson, Co-Chair Sen. Elizabeth Steiner Hayward, Co-Chair Sen. Fred Girod, Co-Vice Chair Sen. Lew Frederick Sen. Chuck Thomsen Sen. Kathleen Taylor Sen. Tim Knopp Sen. Kate Lieber Sen. Bill Hansell Sen. Chris Gorsek Sen. Dick Anderson Sen. Jeff Golden Joint Ways & Means on Human Services Sub-Committee Sen. Kate Lieber, Co-Chair Sen. Tim Knopp Sen. Sara Gelser OREGON COALITION OF LOCAL HEALTH OFFICIALS 2021 Legislative Toolkit – Senate and House Health Committees 2021 House Health Committees Membership Health Care Committee Meeting Times: 3:15pm Tuesdays and Thursday Rep. Rachel Prusak, Chair Rep. Cedric Hayden, Vice Chair Rep. Andrea Salinas, Vice Chair Rep. Teresa Alonso Leon Rep. Wlnsvey Campos Rep. Maxine Dexter Rep. Christine Drazan Rep. Raquel Moore-Green Rep. Ron Noble Rep. Sheri Schouten Health Care House Subcommittee on COVID-19 Meeting Times: 3:15pm Mondays and Wednesdays Rep. Maxine Dexter, Chair Rep. Cedric Hayden, Vice Chair Rep. Wlnsvey Campos Rep. Raquel Moore-Green Rep. Andrea Salinas Human Services Committee Meeting Times: 3:15pm Mondays and Wednesdays Rep. Anna Williams, Chair Rep. Gary Leif, Vice Chair Rep. -

OREGON STATE LEGISLATURE July 23, 2020 the Honorable William
OREGON STATE LEGISLATURE July 23, 2020 The Honorable William Barr Attorney General U.S. Department of Justice Washington, D.C. 20530 The Honorable Chad Wolf Acting Secretary Department of Homeland Security Washington, D.C. 20528 Dear Sirs, As representatives from communities across the State of Oregon, we are writing to request that you immediately remove federal personnel from the streets of Portland unless authorized by the city’s elected officials. We are aligned with members of our federal delegation, including Senators Jeff Merkley and Ron Wyden and Congress members Suzanne Bonamici and Earl Blumenauer, Governor Kate Brown, our Attorney General Ellen Rosenblum, and Portland’s mayor, Ted Wheeler, in our shared assessment that the uninvited presence of federal agents is an abuse of power. Upon assuming office, we each took a vow to defend the Constitutions of the United States and the State of Oregon. We take that responsibility to heart. Confronted with clear evidence that federal agents are engaging in unconstitutional activities resulting in significant harm to individuals and our community as a whole, we are obligated to respond. We refuse to allow our streets to be a playground for political theatrics intended to deflect attention from the president’s failure to control a deadly pandemic. We will not stand by while violent actions exacerbate conditions on our streets. Accordingly, we demand the immediate withdrawal of federal operatives from the City of Portland. Regards, Representative Pam Marsh, HD 05 Representative Alissa Keny-Guyer, HD 46 Capitol Address: 900 Court St NE, Salem, OR 97301 Contact: Rep Pam Marsh, Phone: (503) 986-1405, [email protected] Speaker Tina Kotek, HD 44 Senate Majority Leader Rob Wagner, SD 19 House Majority Leader Barbara Smith Senator Elizabeth Steiner Hayward MD, SD 17 Warner, HD 45 Representative Dan Rayfield, HD 16 Senator Lew Frederick, SD 22 Representative Tawna Sanchez, HD 43 Senator James I. -

OPHA Bill HB2337 Info Sheet Racism Is a Public Health Crisis
OPHA Bill HB2337 Info Sheet Racism is a Public Health Crisis Purpose • Declare racism as a public health crisis in Oregon. • Acknowledge Oregon’s racist history and its current day impact on policies and systems that perpetuate in- stitutional racism which causes harm, trauma, illness and death to Black, Indigenous, and people of color (BIPOC) Oregonians, and the need to heal these injustices through accelerated intentional actions. • Articulate investments and strategies needed to address health inequities among BIPOC Oregonians and Oregon Tribes: Invest in the following key strategies: 1. The collection of race, ethnicity, language, and disability (REAL-D) data is critical for better understanding population health by systematically measuring more granular level data to reveal the unique inequities faced by specific communities across the state. In turn, this data informs future investments in addressing health inequi- ties to focus efforts specifically where they are needed most and thereby more effectively and efficiently use and save state resources. a. Expands the collection of REAL-D data to all state agencies, subcontractors and vendors as practica- ble. b. Clarifies representation on advisory committees that informs updates to data collection standards are diverse and include at minimum: BIPOC community members, the nine federally recognized Oregon Tribes (if there is interest in participating), people with disabilities, and people with limited English profi- ciency. 2. Local public health authorities provide data to Oregon Health Authority (OHA) to develop a statewide mobile health unit plan. These units will focus on providing basic health, behavioral health, oral health, and connection to other wraparound services specifically for BIPOC communities. -

2020 Contributions
State Candidate Names Committee Amount Party Office District CA Holmes, Jim Jim Holmes for Supervisor 2020 $ 700 O County Supervisor 3 CA Uhler, Kirk Uhler for Supervisor 2020 $ 500 O County Supervisor 4 CA Gonzalez, Lena Lena Gonzalez for Senate 2020 $ 1,500 D STATE SENATE 33 CA Lee, John John Lee for City Council 2020 - Primary $ 800 O City Council 12 CA Simmons, Les Simmons for City Council 2020 $ 1,000 D City Council 8 CA Porada, Debra Porada for City Council 2020 $ 500 O City Council AL CA California Manufacturers & Technology Association Political Action Committee $ 5,000 CA Desmond, Richard Rich Desmond for Supervisor 2020 $ 1,200 R County Supervisor 3 CA Hewitt, Jeffrey Jeffrey Hewitt for Board of Supervisors Riverside County 2018 $ 1,200 O County Supervisor 5 CA Gustafson, Cindy Elect Cindy Gustafson Placer County Supervisor, District 5 - 2020 $ 700 O County Supervisor 5 CA Cook, Paul Paul Cook for Supervisor 2020 $ 1,000 R County Supervisor 1 CA Flores, Dan Dan Flores for Supervisor 2020 $ 500 County Supervisor 5 CA California Taxpayers Association - Protect Taxpayers Rights $ 800,000 CA Latinas Lead California $ 500 CA Wapner, Alan Wapner for Council $ 1,000 City Council CA Portantino, Anthony Portantino for Senate 2020 $ 2,000 D STATE SENATE 25 CA Burke, Autumn Autumn Burke for Assembly 2020 $ 2,000 D STATE HOUSE 62 CA California Republican Party - State Account $ 15,000 R CA Fong, Vince Vince Fong for Assembly 2020 $ 1,500 D STATE HOUSE 34 CA O'Donnell, Patrick O'Donnell for Assembly 2020 $ 4,700 D STATE HOUSE 70 CA Sacramento Metropolitan Chamber Political Action Committee $ 2,500 CA Patterson, Jim Patterson for Assembly 2020 $ 1,500 R STATE HOUSE 23 CA Arambula, Joaquin Dr. -

Medicaid Advisory Committee
Division of Health Policy and Analytics MEDICAID ADVISORY COMMITTEE When: January 27, 2021, 9:00am-12:00pm Join on your computer or mobile app Click here to join the meeting Or call in (audio only) +1 971-277-2343,,924842358# United States, Portland Phone Conference ID: 924 842 358# When What Who Welcome and introductions; review Leslee Huggins and Jeremiah Rigsby, 9:00 and approve December minutes MAC Co-Chairs Anna Lansky, Deputy Director, Office of 9:10 DHS Agency Update Developmental Disability Services (DHS) David Inbody, CCO Operations Manager 9:25 OHA Agency Update (OHA) Jeff Scroggin, Sr. Policy Advisor, OHA 9:40 Legislative Update Government Relations Advancing Consumer Experience 10:10 Lavinia Goto, Subcommittee Chair Subcommittee Update 10:30 Break Health-related Services Spending Anona Gund, Transformation Analyst, OHA 10:40 Trend for CCOs Transformation Center 11:10 OHPB Retreat - Discussion Jeremiah Rigsby and Leslee Huggins 11:20 Public Comment 11:30 Wrap up / adjourn Next Meeting: February 24, 2021 9:00 am -12:00 TBD OREGON MEDICAID ADVISORY COMMITTEE (MAC) December 2, 2020 9:00 AM – 12:00 PM MEMBERS IN ATTENDANCE: Adrienne Daniels, Daniel Alrick, Dave Inbody, Jeremiah Rigsby, Karun Virtue, Lavinia Goto, Leslee Huggins, Tamara Bakewell, Brandy Charlan, Kevin Alfaro-Martinez MEMBERS ABSENT: Anna Lansky, Miguel Angel-Herrada Quorum? Yes PRESENTERS: Sarah Dobra, Lisa Bui, Veronica Guerra, Joelle Archibald, Lauren Kustudick, Oceana Gonzales, Sarah Dobra, Joell Archibald, Dustin Zimmerman STAFF: Jackie Wetzel, Tom Cogswell, Margie Fernando TOPIC Key Discussion Points Jeremiah Rigsby welcomed everyone to the meeting, and members introduced themselves. There was a motion to approve the minutes of 10/28/20; All votes were in favor of approval of the Welcome and Introductions 9/30/20 minutes.