Prevalence and Risk Factors Associated with Polyparasitism in Okpokwu Benue State, Nigeria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

REQUEST for PROPOSAL Living Income Benchmarking
REQUEST FOR PROPOSAL Living Income Benchmarking (LIB) Study in Nigeria 1 1.0 General Information This document is being issued in order to solicit applications from potential [firms or consultants] to conduct a living income benchmarking study. The activity entails collecting data in four states in Nigeria, precisely in Ogun State (Odeda Local Government Area - LGA, Ijebu-Ode LGA, Ewekoro LGA, and Odogbolu LGA), Edo State (Ikpoba Okha LGA, Oredo LGA, Egor LGA), Benue State (Agatu LGA, Guma LGA, Gwer-East LGA, Gwer-West LGA, Logo LGA, Okpokwu LGA, Ogbadigbo LGA, and Kwande LGA), and Nasarawa State (Awe LGA, Doma LGA, Lafia LGA, Obi LGA). It will require at least 19 qualitative interviews (19 Focus Group Discussions and 57 Key Informant Interviews), 19 market surveys and an extensive secondary data review. Ultimately, HI anticipates the consultant to consolidate the LIBs based on cost similarities in the States, LGAs or location (Rural/Urban). The terms of reference contain background information, the desired methodology, including objectives, the timeframe, and a list of deliverables. This document also contains information about the kind of expertise that Heifer seeks for this activity and guidance on how to submit a proposal to conduct the activity. Heifer anticipates awarding a fixed award for the study and make payments based on submission and Heifer’s approval of deliverables. The award agreement will include a payment schedule with specific deliverables; all payments require 10 business days processing after approval of deliverables. 1.1 Background of Heifer International Heifer Project International (HPI) is a global non-profit working to end hunger and poverty and care for the Earth by using sustainable practices and engaging smallholder farmers in agricultural development. -

The October 13, 2010 Landslides on the Azenge Mountain in Imande Ukusu, Nkomon Disrict, Benue State, Nigeria
Environment and Ecology Research 2(3): 113-121, 2014 http://www.hrpub.org DOI: 10.13189/eer.2014.020301 The October 13, 2010 Landslides on the Azenge Mountain in Imande Ukusu, Nkomon Disrict, Benue State, Nigeria Ako Thomas Agbor*, Abba Francis Mohammed, Onoduku usman Shehu, Nuhu Waziri Musa, Alabi Adekola A., Mamodu Adegbe Department of Geology, School of Natural and Applied Sciences, Federal University of Technology, Minna, Nigeria *Correspondent author: [email protected] Copyright © 2014 Horizon Research Publishing All rights reserved. Abstract A swarm of 14 landslides occurred Landslides are geological phenomenon which occurs as a spontaneously within the Azenge Mountain on November result of ground movement, rock falls, and failure of unstable 13th, 2010 between the hours of 1 and 6 am after torrential slopes; sand and debris flow on slope and can cause a lot of rains. The landslides were studied using interviews, field damages with direct and indirect effect on human settlements observations and laboratory study of the soil samples and physical infrastructure [1]. According to [ 2 ] landslide collected from the major landslide site. Results of the study describes a wide variety of processes that result in the show that the event that was reported by many local media in downward and outward movement of slope forming Nigeria as volcanic eruption was a spontaneous massive materials including rocks, soil, artificial fills or a slope movement along the mountainous terrain of Imande combination of them. Landslides are common in areas where Ukusu, Mon village. About 1,123,918 m3 of rock and debris slope stability has been compromised. -

Information Needs of Cassava Farmers in Okpokwu Local Government Area of Benue State, Nigeria
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Library Philosophy and Practice (e-journal) Libraries at University of Nebraska-Lincoln Summer 5-21-2019 Information Needs of Cassava Farmers In Okpokwu Local Government Area of Benue State, Nigeria. Tofi imonS Ternenge CLN Benue State School of Nursing, Makurdi, [email protected] Tondo Richard Iorver Benue State School of Midwifery, Makurdi, [email protected] Egbe Francis Ebute University of Agriculture, Makurdi Follow this and additional works at: https://digitalcommons.unl.edu/libphilprac Part of the Library and Information Science Commons Ternenge, Tofi imonS CLN; Iorver, Tondo Richard; and Ebute, Egbe Francis, "Information Needs of Cassava Farmers In Okpokwu Local Government Area of Benue State, Nigeria." (2019). Library Philosophy and Practice (e-journal). 2981. https://digitalcommons.unl.edu/libphilprac/2981 INFORMATION NEEDS OF CASSAVA FARMERS IN OKPOKWU LOCAL GOVERNMENT AREA OF BENUE STATE, NIGERIA. BY TOFI, SIMON TERNENGE (CLN) Librarian II, Benue State School of Nursing, Makurdi Email: [email protected] Phone: 07036431885 TONDO, RICHARD IORVER Librarian II, Benue State School of Midwifery, Makurdi Email: [email protected] Phone: 08065067151 & EGBE, FRANCIS EBUTE Higher Library Officer, Francis Sulemanu Idachaba Library. University of Agriculture, Makurdi Phone: 09063544557 1 ABSTRACT This Research work was designed to investigate the information needs of Cassava Farmers in Okpokwu Local Government Area of Benue State. The Study adopted a survey research design. Questionnaire was used to collect data for the study, the study identified the information needs of Cassava Farmers, the sources available the them, the kinds of information, Cassava Farmers use to improve their yield, the means/sources Cassava Farmers use to get their information, problems of information dissemination to Cassava farmers and strategies to overcome problems. -

Infrastructural, Institutional and Human Capacity Requirements for the E-Wallet System of Input Distribution in Okpokwu Local Government Area, Benue State, Nigeria
IOSR Journal Of Humanities And Social Science (IOSR-JHSS) Volume 24, Issue 3, Ser. 8 (March. 2019) 29-34 e-ISSN: 2279-0837, p-ISSN: 2279-0845. www.iosrjournals.org Infrastructural, Institutional and Human Capacity Requirements for the E-Wallet System of Input Distribution in Okpokwu Local Government Area, Benue State, Nigeria 1 1 Naswem, A.A. , Iornenge, G.M and Adeyi, E 1(Department of Agricultural Extension and Communication, Federal University of Agriculture, Makurdi, Benue State, Nigeria) Abstract: The distribution of subsidized inputs to farmers in Nigeria has been an enduring problematic over the years. Various policy experiments in this regard have ended up by-passing the intended beneficiaries and distorting the market. Under the Growth Enhancement Support Scheme (GESS), the e-wallet system was introduced to ensure that subsidized inputs are delivered to farmers. Since it is an ICT-based intervention, its impact is dependent upon the availability of certain infrastructural, institutional and human capacity elements. The study aimed at assessing the availability of these elements in a typical Nigerian farming community. The study utilized a cross- sectional survey design with a structured questionnaire administered to a sample of 90 respondents. The results showed that access to steady electricity was low at 7.8%. Ownership of handsets was very high at 92.2%, but only 24.4% had access to good GSM network signals; 67.8% of the respondents had to travel for more than 3km to input collection centres. On the whole, only 41.1 were able -
AFRICAN PROGRAMME for CONTROL (APOC) Ff,Iam ONCHOCERCTASTS I I I ,I
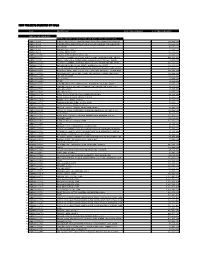
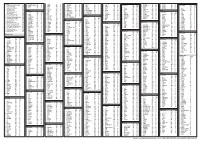
I rll I _. _-,__,__. -._ -_,- .---_ -- --,,t ORIGINAL: English COUNTRY/NOTFz Nigeria Proiect Nanqez Benue State CDTI Proiect Approval year: 1999 Launching year: 1999 Reporting Period (Month/Year) z October, 2000 - September, 2001 Date Re-submitted: January 2004 NGDO partner: UNICEF YEAR 2 PROJECT TECHNICAL REPORT TO TECHNICAL CONSULTATIVE COMMITTEE (TCC) t-.-_ .) I CL ! l3 I C,oorb I r5L I CEv CDf Bth BEt RECU --l I lt , t, 2 6 FFV. 2004 tc, \tR. i A\i APOC/DIR I i ( AFRICAN PROGRAMME FOR CONTROL (APOC) ff,iaM ONCHOCERCTASTS I i i ,i WI-lO/APOC. 26 September 2003 ANNUAL PROJECT TECHNICAL REPORT { TO TECHNICAL CONSULTATIVE COMMITTEE (TCC) ENDORSEMENT Please confirm you have read this report by signing in the appropriate space. OFFICERS to sign the report: country NIGERIA/LIBERIA National Coordinator Same: Dr. J. Y. Jiya t/r,,rnurur" \ /e Date: Zonal Oncho Coordinator Name: Dr. U. E. Udofo Signature Date: ... This report has been prepared by Name '. Mrs. Betty Jande Designation : Proiect Coo rdi nator Signature Date 2 WIIO/APOC. 26 September 2003 Table of contents Acronyms..... .1 Definitions..... ..5 FOLLOW UP ON TCC RECON|MENDATIONS I 2 Execut ive Sum mary....... SECTION l: Background information J l.l. GeNsRalINFoRMATIoN............... .3 .3 I . I .l. Desuiption of the project (brieJly) l. 1.2. P artnership........ ,4 1.2. POPULATION AND HEALTH SYSTEM....... .5 SECTION 2: lmplementation of CDT|...... .6 2.1. Psntoo oF ACTIVITIES .............. ,6 2.2. ORopRtNc, sroRAGE AND DELIVERY oF IVERMECTIN ....'...' .8 2.3. AovocRcv AND SENSITIZATIoN l0 2.4. -
New Projects Inserted by Nass
NEW PROJECTS INSERTED BY NASS CODE MDA/PROJECT 2018 Proposed Budget 2018 Approved Budget FEDERAL MINISTRY OF AGRICULTURE AND RURAL SUPPLYFEDERAL AND MINISTRY INSTALLATION OF AGRICULTURE OF LIGHT AND UP COMMUNITYRURAL DEVELOPMENT (ALL-IN- ONE) HQTRS SOLAR 1 ERGP4145301 STREET LIGHTS WITH LITHIUM BATTERY 3000/5000 LUMENS WITH PIR FOR 0 100,000,000 2 ERGP4145302 PROVISIONCONSTRUCTION OF SOLAR AND INSTALLATION POWERED BOREHOLES OF SOLAR IN BORHEOLEOYO EAST HOSPITALFOR KOGI STATEROAD, 0 100,000,000 3 ERGP4145303 OYOCONSTRUCTION STATE OF 1.3KM ROAD, TOYIN SURVEYO B/SHOP, GBONGUDU, AKOBO 0 50,000,000 4 ERGP4145304 IBADAN,CONSTRUCTION OYO STATE OF BAGUDU WAZIRI ROAD (1.5KM) AND EFU MADAMI ROAD 0 50,000,000 5 ERGP4145305 CONSTRUCTION(1.7KM), NIGER STATEAND PROVISION OF BOREHOLES IN IDEATO NORTH/SOUTH 0 100,000,000 6 ERGP445000690 SUPPLYFEDERAL AND CONSTITUENCY, INSTALLATION IMO OF STATE SOLAR STREET LIGHTS IN NNEWI SOUTH LGA 0 30,000,000 7 ERGP445000691 TOPROVISION THE FOLLOWING OF SOLAR LOCATIONS: STREET LIGHTS ODIKPI IN GARKUWARI,(100M), AMAKOM SABON (100M), GARIN OKOFIAKANURI 0 400,000,000 8 ERGP21500101 SUPPLYNGURU, YOBEAND INSTALLATION STATE (UNDER OF RURAL SOLAR ACCESS STREET MOBILITY LIGHTS INPROJECT NNEWI (RAMP)SOUTH LGA 0 30,000,000 9 ERGP445000692 TOSUPPLY THE FOLLOWINGAND INSTALLATION LOCATIONS: OF SOLAR AKABO STREET (100M), LIGHTS UHUEBE IN AKOWAVILLAGE, (100M) UTUH 0 500,000,000 10 ERGP445000693 ANDEROSION ARONDIZUOGU CONTROL IN(100M), AMOSO IDEATO - NCHARA NORTH ROAD, LGA, ETITI IMO EDDA, STATE AKIPO SOUTH LGA 0 200,000,000 11 ERGP445000694 -

Abia Adamawa Akwa Ibom
INDEPENDENT NATIONAL ELECTORAL COMMISSION 2019 GENERAL ELECTIONS HOUSE OF REPRESENTATIVES ELECTIONS HELD ON 23RD FEBRUARY AND 9TH MARCH 2019 LIST OF MEMBERS-ELECT OF THE HOUSE OF REPRESENTATIVES STATE SN CONSTITUENCY CANDIDATE GENDER PARTY REMARKS ABIA 1 ABA NORTH / ABA SOUTH OSSY EHIRIODO OSSY PRESTIGE M APGA CHINEDU 8 2 AROCHUKWU / OHAFIA NKOLE UKO NDUKWE M PDP 3 BENDE BENJAMIN OKEZIE KALU M APC 4 IKWUANO / UMUAHIA SAMUEL IFEANYI ONUIGBO M PDP NORTH / UMUAHIA SOUTH 5 ISIALA NGWA NORTH / DARLINGTON NWOKOCHA M PDP SOUTH 6 ISUIKWUATO / NKEIRUKA C. ONYEJEOCHA F APC UMUNEOCHI 7 OBINGWA / OSISIOMA / SOLOMON ADAELU M PDP UGWUNAGBO 8 UKWA EAST / UKWA WEST UZOMA NKEM ABONTA M PDP ADAMAWA 8 9 DEMSA / LAMURDE / KWAMOTI BITRUS LAORI M PDP NUMAN 10 FUFORE / SONG MUHAMMED MUSTAFA SAIDU M PDP 11 GANYE / JADA / MAYO ABDULRAZAK SA’AD NAMDAS M APC BELWA / TOUNGO 12 YOLA NORTH / YOLA ABDULRAUF ABDULKADIR MODIBBO M APC SOUTH/ GIREI 13 GOMBI / HONG YUSUF BUBA YAKUB M APC 14 GUYUK / SHELLENG GIBEON GOROKI M PDP 15 MADAGALI / MICHIKA ZAKARIA DAUDA NYAMPA M PDP 16 MAIHA / MUBI NORTH / JAAFAR ABUBAKAR MAGAJI M APC MUBI SOUTH AKWA IBOM 10 17 ABAK / ETIM EKPO / IKA ANIEKAN JOHN UMANAH M PDP 18 EKET / ESIT EKET / IBENO IFON PATRICK NATHAN M PDP / ONNA 19 IKOT EKPENE / ESSIEN IKONG NSIKAK OKON M PDP UDIM / OBOT AKARA 20 ETINAN / NSIT IBOM / NSIT ONOFIOK AKPAN LUKE M PDP UBIUM 21 UYO / URUAN /NSIT ATAI / ENYONG MICHAEL OKON M PDP ASUTAN / IBESIKPO 22 ITU /IBIONO IBOM ARCHIBONG HENRY OKON M PDP 23 IKONO / INI EMMANUEL UKPONG-UDO EFFIONG M PDP 24 IKOT ABASI / MKPAT -
States and Lcdas Codes.Cdr
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -

Co-Endemicity, Poly-Parasitism and Poverty:Need for Baseline Research and Evidence Based Intervention
IOSR Journal Of Humanities And Social Science (IOSR-JHSS) Volume 21, Issue 1, Ver. V (Jan. 2016) PP 07-17 e-ISSN: 2279-0837, p-ISSN: 2279-0845. www.iosrjournals.org Co-Endemicity, Poly-Parasitism and Poverty:Need For Baseline Research and Evidence Based Intervention. Aju-Ameh, Celina Onyawoibi. 1Faculty of Natural Sciences, Department of zoology. University of Jos, Plateau State, Nigeria. Abstract: The unseen complexity behind the emerging trend of co-endemicity and poly parasitism along with the incapacitating forces of poverty is ably set to hinder the people of Benue state from attaining their full potential.This article though not an exhaustive list seeks to explore some of the challenges needing urgent and aggressive attention. The limitations of the available data(fabricated and captured), the dearth of information and the challenging effort made at gathering evidence of better quality is clearly expressed. There is no significant difference in the living conditions of the urban poor and rural poor who are the majority. Common to both groups are lack of access to quality education, housing, clean water and health care. The three pandemic diseases Aids/HIV, Tuberculosis, Malaria [ATM] and five of the neglected tropical diseases are all endemic in this state and in some places co-exist, an assault that needs evidence based intervention. As unfathomable as the realities on ground are, I have gone through the maze to provide a panoramic view of some of these diseases, in some cases the risk factors and the extent to which obstacles hinder effective control and management of these diseases in the food basket of the nation- Benue state, Nigeria. -

Impact of Extension Services on Cassava Farming in Benue State, Nigeria
International Journal of Business, Humanities and Technology Vol. 2 No. 6; October 2012 Impact of Extension Services on Cassava Farming in Benue State, Nigeria Victoria Ada Okwoche Department of Agricultural Extension and Communication University of Agriculture P.M.B. 2373, Makurdi, Benue State, Nigeria. Benjamin Chijioke Asogwa Department of Agricultural Economics University of Agriculture P.M.B. 2373, Makurdi, Benue State, Nigeria. Abstract The study assessed the impact of access to extension services on cassava farming in Benue State, Nigeria. Data were collected from 180 randomly sampled cassava farmers from nine local government areas in Benue State using a structured questionnaire. Data collected were analysed using descriptive statistics and inferential statistics. The study showed that only 47.78% of the farmers had access to extension services. The study showed that there was a significant relationship between farmers’ access to extension services and profitability of farming. Farmers who had access to extension services ha higher profits. Access to extension services had significant impact on the profitability of cassava farming in the study area. The study recommended that extension agents should put more effort in reaching cassava farmers that have not had contact with them so as to pass useful information to them in order to increase their profitability. Cassava farmers should be encouraged by extension agents to subscribe to the various cassava farmers group. Cassava farmers should be mobilized to establish cooperative society in order to enjoy government provision of capital under poverty alleviation programmes. Adequate mobility should be provided for the extension agents for effective coverage of the areas of information need. -

Cameroun Countries State Main Roads XXX LGA (Local Governmental Area) Hydrography
Cholera - Nigeria hotspots location by state Platform Cholera Benue State West and Central Africa Plateau Nasarawa Taraba Guma ObangeddeAgatu Gbajimba Hotspots typology in the State Yagba Markurdi Hotspot type T.1: High priority area with a high frequency Okpogu Logo Gwer West Ukum and a long duration. Apa Naka Tarka Wannune Ugba Zaki Biam Kogi Buruku Hotspot type T.2: Medium priority area with a moderate frequency Oturkpo Gwer East Bukuru and a long duration Gboko Gboko Aliade Katsina-Ala Awajir Ohimini Oturkpo Hotspots distribution in the State Katsina Ala Konshisha Otukpa Ushongo Okpokwu Konshisha Ogbadibo Obi Kornya 1 2 Vandeikya Adikpo Hotspot Type 1 Hotspots Type 2 Oju Oju Igumale Vande Ikya Kwande Ado Markurdi Guma Enugu Obi Cross River Ebonyi Legend Cameroun Countries State Main roads XXX LGA (Local Governmental Area) Hydrography XXX Cities (State capital, LGA capital, and other towns) 0 70 140 280 420 560 Kilometers Date of production: January 21, 2016 Source: Ministries of Health of the countries members of the Cholera platform Contact : Cholera project - UNICEF West and Central Africa Regionial Office (WCARO) Feedback : Coordination : Julie Gauthier | [email protected] Information management : Alca Kuvituanga | [email protected] : of support the With The epidemiological data is certified and shared by national authorities towards the cholera platform members. Geographical names, designations, borders presented do not imply any official recognition nor approval from none of the cholera platform members .