Guidelines Aplastic Anemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

Treatment of MDS in 2014 and Beyond Treatment Goals in MDS
5/22/2014 Treatment of MDS in 2014 and Beyond Treatment goals in MDS • Get rid of it May 17, 2014 • If you can’t do that, make life better and longer – Improve blood counts Gail J. Roboz, M.D. – Improve quality of life Director, Leukemia Program – Decrease time to progression/leukemia Associate Professor of Medicine Hematopoietic Growth Factors: Hematopoietic Growth Factors: What are they? What are they? • Erythropoietin (EPO,Procrit®, Epogen®) – red • Synthetic versions of proteins normally • Granulocyte colony stimulating factor (GCSF, made in the body to stimulate growth of red Neupogen®) – white cells, white cells and platelets • Granulocyte-macrophage colony stimulating • Promote growth and differentiation factor (GM-CSF, Leukine®) – white • Thrombopoietin (TPO, romiplostim, Nplate®) – • Inhibitors of apoptosis (cell death) platelets • Darbepoietin (Aranesp®) • Peg-filgrastim (Neulasta®) • Note, these are not FDA-approved for MDS Erythropoietin (epo) in MDS Erythropoietin (epo) in MDS • Anemia is presents in >80% of MDS pts at dx • Often high endogenous epo levels • Transfusions help, but many issues • Many different doses and schedules • Recombinant EPO is FDA-approved for treating • Higher response rates with epo + G-CSF if anemia associated with kidney failure epo ≤500 mU/mL and transfusions <2 • Has been used since about 1990 in MDS U/month • Response rates in about 15-30% of patients • Poor probability of response if epo >500 • Many different studies including >1000 patients mU/mL and transfusions >2 U/month • Part of the NCCN MDS treatment guidelines 1. Casadevall N, et al. Blood. 2004;104:321-327. 2. Hellstrom-Lindberg E. Br J Haematol. 1995;89:67-71. -

S. No. Name of the Firm Date of Permission No. Name of the Indication Dosage Form & Strength
List of new drugs (r-DNA origin) approved for mannufacture and marketing in India for the Year 2021 S. No. Name of the firm Date of Permission No. Name of the Indication Dosage Form & Strength Rheumatoid Arthritis (RA)–Etanercept in combination with methotrexate is indicated for the treatment of moderate to severe active rheumatoid arthritis in adults when the response to disease-modifying antirheumatic drugs, including methotrexate (unless contraindicated), has been inadequate.Etanercept can be given as monotherapy in case of intolerance to methotrexate or when continued treatment with methotrexate is inappropriateEtanercept is also indicated in the treatment of severe, active and progressive rheumatoid arthritis in adults not previously treated with methotrexate. Etanercept, alone or in combination with methotrexate, has been shown to reduce the rate of progression of joint damage as measured by X-ray and to improve physical functionJuvenile Idiopathic Arthritis (JIA) – Treatment of polyarthritis (rheumatoid factor positive or negative)and extended oligoarthritis in children and adolescents from the age of 2 years who have had aninadequate response to, or who have proved intolerant of, methotrexate.Treatment of psoriatic arthritis in adolescents from the age of 12 years who have had an inadequate response to, or who have proved intolerant of, methotrexate.Treatment of enthesitis-related arthritis in adolescents from the age of 12 years who have had an inadequate response Solution for subcutaneous Injection (single use)Pre- Mylan Pharmaceuticals to, or who have proved intolerant of, conventional therapy.Etanercept has not been studied in children aged less than 2 filled syringe:(i). 50 mg/mL in Prefilled Syringes(ii). -

Novel Concepts of Treatment for Patients with Myelofibrosis And
cancers Review Novel Concepts of Treatment for Patients with Myelofibrosis and Related Neoplasms Prithviraj Bose * , Lucia Masarova and Srdan Verstovsek Department of Leukemia, University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA; [email protected] (L.M.); [email protected] (S.V.) * Correspondence: [email protected] Received: 30 August 2020; Accepted: 1 October 2020; Published: 9 October 2020 Simple Summary: Myelofibrosis (MF) is an advanced form of a group of rare, related bone marrow cancers termed myeloproliferative neoplasms (MPNs). Some patients develop myelofibrosis from the outset, while in others, it occurs as a complication of the more indolent MPNs, polycythemia vera (PV) or essential thrombocythemia (ET). Patients with PV or ET who require drug treatment are typically treated with the chemotherapy drug hydroxyurea, while in MF, the targeted therapies termed Janus kinase (JAK) inhibitors form the mainstay of treatment. However, these and other drugs (e.g., interferons) have important limitations. No drug has been shown to reliably prevent the progression of PV or ET to MF or transformation of MPNs to acute myeloid leukemia. In PV, it is not conclusively known if JAK inhibitors reduce the risk of blood clots, and in MF, these drugs do not improve low blood counts. New approaches to treating MF and related MPNs are, therefore, necessary. Abstract: Janus kinase (JAK) inhibition forms the cornerstone of the treatment of myelofibrosis (MF), and the JAK inhibitor ruxolitinib is often used as a second-line agent in patients with polycythemia vera (PV) who fail hydroxyurea (HU). In addition, ruxolitinib continues to be studied in patients with essential thrombocythemia (ET). -

Nplate (Romiplostim) Discard Any Unused Portion of the Single-Use Vial
HIGHLIGHTS OF PRESCRIBING INFORMATION Do not shake during reconstitution; protect reconstituted Nplate from These highlights do not include all the information needed to use Nplate light; administer reconstituted Nplate within 24 hours. (2.2) safely and effectively. See full prescribing information for Nplate. The injection volume may be very small. Use a syringe with graduations to 0.01 mL. (2.2) ® Nplate (romiplostim) Discard any unused portion of the single-use vial. (2.2) For subcutaneous injection ---------------------DOSAGE FORMS AND STRENGTHS---------------------- 250 mcg or 500 mcg of deliverable romiplostim in single-use vials ( 3) Initial U.S. Approval: 2008 ---------------------------RECENT MAJOR CHANGES--------------------------- -------------------------------CONTRAINDICATIONS ---------------------------- Indications and Usage (1) 07/2011 None (4) Dosage and Administration, Nplate Distribution removal 12/2011 -----------------------WARNINGS AND PRECAUTIONS------------------------ Program (2) In patients with MDS, Nplate increases blast cell counts and increases Warnings and Precautions: Progression of Myelodysplastic the risk of progression to acute myelogenous leukemia. (5.1) Syndromes (5.1) 07/2011 Thrombotic/thromboembolic complications may result from increases in Warnings and Precautions: Thrombotic/Thromboembolic platelet counts with Nplate use. Portal vein thrombosis has been Events (5.2) 07/2011 reported in patients with chronic liver disease receiving Nplate. Use Warning and Precaution: Bone Marrow Reticulin Formation with additional caution in ITP patients with chronic liver disease. (5.2) and Fibrosis (5.3) 12/2011 Discontinuation of Nplate may result in worsened thrombocytopenia Warnings and Precautions: Laboratory Monitoring (5.6) 12/2011 than was present prior to Nplate therapy. Monitor complete blood Warnings and Precautions: Nplate Distribution removal 12/2011 counts (CBCs), including platelet counts, for at least 2 weeks following Program (5.7) Nplate discontinuation. -

Romiplostim Reverts the Thrombocytopenia in Dengue Hemorrhagic Fever
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector letter Romiplostim reverts the 160 thrombocytopenia in den- gue hemorrhagic fever 140 120 To the Editor: First-genera- /L) tion thrombopoietic agents were 9 100 recombinant forms of human thrombopoietin (TPO), but their 80 development was discontinued due to the onset of neutralizing auto- 60 Platelet count (×10 antibodies cross-reacting with 40 endogenous TPO. Second-gen- eration thrombopoiesis-stimulat- 20 ing molecules (romiplostim and 0 eltrombopag), have completed 0 10 20 0 40 50 55 60 70 80 90 100 110 120 10 140 150 160 170 180 190 200 210 220 20 phase III trials in primary im- Time in days mune thrombocytopenia, whereas 9 phase II and III trials are ongoing Figure 1. Platelet count (x10 /L) by day. Arrows denote doses of romiplostim (4 µg/kg). in other conditions characterized by thrombocytopenia.1 Dengue gen and IgM antibodies were pres- DHF in which romiplostim has is the most prevalent arthropod- ent; the bone marrow had hypo- been successfully used. An immune borne virus affecting humans to- plasia and no evidence of myeloma mechanism of thrombocytopenia day causing a spectrum of disease, was found. The patient was treated due to increased platelet destruc- ranging from a mild febrile illness with intravenous hydrocortisone tion appears to be operative in pa- to a life-threatening dengue hem- (300 mg/day) and subcutaneous tients with DHF;9 however, in the orrhagic fever (DHF).2 The main filgrastim (300 ug/day), with the case that we are reporting, the previ- hematological findings of dengue neutropenia resolving 4 days later. -
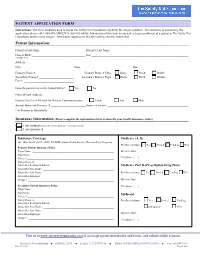
Patient's Name
PATIENT APPLICATION FORM Instructions: This form should be used to assess The Safety Net Foundation eligibility for Amgen products. For assistance in completing this application, please call 1-888-SN-AMGEN (1-888-762-6436). Submission of this form is required to begin enrollment of a patient in The Safety Net Foundation sponsored by Amgen. Information supplied on this form will be strictly confidential. Patient Information: Patient’s First Name: ______________________________ Patient’s Last Name: ____________________________________________________ Date of Birth: ____________________________________ Sex: _________________________________________________________________ (MMDDYYYY) Address: ____________________________________________________________________________________________________________ City: ___________________________________ State: __________________________________ Zip: _________________________________ Primary Phone #: _________________________ Primary Phone # Type: Home Work Mobile Secondary Phone #: _______________________ Secondary Phone # Type: Home Work Mobile Fax #: _________________________________ Does the patient live in the United States?: Yes No Patient Email Address: _________________________________________________________________________________________________ Patient’s Preferred Method for Written Communications: Email Fax Mail Annual Household Income: $ _______________________ Source of Income: ______________________________________________________ # of Persons in Household: _________________________ -

Romiplostim (Nplate), Eltrombopag (Promacta)
Clinical Policy: romiplostim (Nplate), eltrombopag (Promacta) Reference Number: CP.CPA.104 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal See Important Reminder at the end of this policy for important regulatory and legal information. Description The following are thrombopoietin receptor agonists requiring prior authorization: romiplostim (Nplate™), eltrombopag (Promacta®). FDA approved indication Nplate and Promacta are indicated for the treatment of thrombocytopenia in patients with chronic immune (idiopathic) thrombocytopenic purpura (ITP) who have had an insufficient response to corticosteroids, immunoglobulins or splenectomy. Limitation of use: Nplate and Promacta • Should be used only in patients with ITP whose degree of thrombocytopenia and clinical condition increase the risk for bleeding. • Should not be used in an attempt to normalize platelet counts. Policy/Criteria Provider must submit documentation (which may include office chart notes and lab results) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Nplate or Promacta is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Chronic Idiopathic Thrombocytopenic Purpura (ITP) (must meet all): 1. Diagnosis of ITP (chronic, relapsed, or refractory) with an increased risk for bleeding based on the degree of thrombocytopenia and clinical condition; 2. Request is for Promacta or Nplate; 3. Dose does not exceed: 10 mcg/kg/week (Nplate); 75 mg/day (Promacta). Approval duration: Promacta: Length of benefit Nplate: 6 months or to member’s renewal period, whichever is longer. B. Chronic Hepatitis C Thrombocytopenia (must meet all): 1. Diagnosis of thrombocytopenia in patients with chronic hepatitis C; 2. -

Standard Specialty PA and QL List January 2015
Standard Specialty PA and QL List January 2015 Standard PA or PA with QL Programs Therapeutic Category Drug Name Quantity Limit Anti-infectives Antiretrovirals, Hepatitis B BARACLUDE (entecavir) 1 tab/day BARACLUDE (entecavir) Soln 630 ml/30days HEPSERA (adefovir) 1 tab/day TYZEKA (telbivudine ) 1 tab/day Antiretrovirals, HIV FUZEON (enfuvirtide) 60 vials or 1 kit/30 days SELZENTRY (maraviroc) None TRUVADA (emtricitabine/tenofovir) None Cardiology Antilipemic JUXTAPID (lomitapide) 20 mg 3 tabs/day JUXTAPID (lomitapide) 5 mg, 10 mg 1 tab/day KYNAMRO (mipomersen) 4 syringes/28 days Pulmonary Arterial Hypertension ADCIRCA (tadalafil) 2 tabs/day ADEMPAS (riociguat) 90 tabs/30 days FLOLAN (epoprostenol) None LETAIRIS (ambrisentan) 1 tab/day OPSUMIT (macitentan) 1 tab/day ORENITRAM (treprostinil diolamine) None REMODULIN (treprostinil) None REVATIO (sildenafil) 3 tabs or vials/day TRACLEER (bosentan) 2 tabs/day TYVASO (treprostinil) 1 ampule/day VELETRI (epoprostenol) None VENTAVIS (iloprost) 9 ampules/day Vasopressors NORTHERA (droxidopa) None Central Nervous System Anticonvulsants SABRIL (vigabatrin) None Depressant XYREM (sodium oxybate) 3 bottles (540 mL)/30 days Neurotoxins BOTOX (onabotulinumtoxinA) None DYSPORT (abobotulinumtoxinA) None MYOBLOC (rimabotulinumtoxinB) None XEOMIN (incobotulinumtoxinA) None Parkinson's APOKYN (apomorphine) None Sleep Disorder HETLIOZ (tasimelteon) 1 cap/day Dermatology Alkylating Agents VALCHLOR (mechlorethamine) Gel None Endocrinology & Metabolism Gonadotropins ELIGARD (leuprolide) 22.5 mg (3-month) 1 -

Nplate® (Romiplostim)
Nplate® (romiplostim) (Subcutaneous) Document Number: IC-0089 Last Review Date: 02/02/2021 Date of Origin: 01/01/2012 Dates Reviewed: 12/2011, 02/2013, 02/2014, 12/2014, 10/2015, 09/2016, 12/2016, 03/2017, 06/2017, 12/2017, 03/2018, 06/2018, 10/2018, 01/2019, 12/2019, 02/2020, 02/2021 I. Length of Authorization Coverage will be provided for 3 months and may be renewed, unless otherwise specified. • Coverage for use to treat Hematopoietic Syndrome of Acute Radiation Syndrome (HSARS) cannot be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: − Nplate 125 mcg SDV for injection: 4 vials per 28 days − Nplate 250 mcg SDV for injection: 20 vials per 28 days − Nplate 500 mcg SDV for injection: 12 vials per 28 days B. Max Units (per dose and over time) [HCPCS Unit]: • ITP: 125 billable units weekly • MDS: 100 billable units weekly • HSARS: 125 billable units x 1 dose III. Initial Approval Criteria 1,3,13,14 Coverage is provided in the following conditions: Universal Criteria 1 • Patient is not on any other thrombopoietin receptor agonist or mimetic (e.g., lusutrombopag, eltrombopag, avatrombopag, etc.) or fostamatinib; AND • Must not be used in an attempt to normalize platelet counts; AND • Laboratory value for platelet count is current (i.e., drawn within the previous 28 days); AND Immune (idiopathic) thrombocytopenia (ITP) † Ф 1,412 Proprietary & Confidential © 2021 Magellan Health, Inc. • The patient is at increased risk for bleeding as indicated by platelet count less than 30 × 109/L (30,000/mm³); AND o Patient has acute ITP; AND . -

A Phase Ib/II Clinical Study of BBI608 in Combination with Sorafenib Or BBI503 in Combination with Sorafenib in Adult Patients with Hepatocellular Carcinoma
TITLE: A Phase Ib/II Clinical Study of BBI608 in Combination with Sorafenib or BBI503 in Combination with Sorafenib in Adult Patients with Hepatocellular Carcinoma PROTOCOL NUMBER: BBI608-503-103HCC STUDY DRUGS: BBI503 BBI608 SPONSOR: Boston Biomedical, Inc. 640 Memorial Drive Cambridge, MA 02139 Telephone: (617) 674-6800 Fax: (617) 674-8662 MEDICAL MONITOR: Waldo Ortuzar, MD SAFETY FAX: (617) 674-8662 SAFETY CONTACT: (617) 674-8722 DATE OF PROTOCOL: September 12, 2014 DATE OF AMENDMENT: December 15, 2016 AMENDMENT: 2 Confidential Page: 1 Boston Biomedical, Inc December 15, 2016 Clinical Protocol BBI608-503-103HCC SYNOPSIS Study Title: A Phase Ib/II Clinical Study of BBI608 in Combination with Sorafenib, or BBI503 in Combination with Sorafenib in Adult Patients with Hepatocellular Carcinoma Study Number: BBI608-503-103HCC Study Phase: Phase Ib/II Study Drugs: BBI608 and BBI503, novel investigational, small molecule, anticancer drugs that target cancer stem cells. Primary Objectives: Phase Ib: To determine the safety, tolerability, and recommended Phase II dose (RP2D) of BBI608 administered in combination with sorafenib and of BBI503 administered in combination with sorafenib in adult patients with advanced hepatocellular carcinoma who have not received prior systemic chemotherapy. Phase II: To evaluate the tolerability, safety. and preliminary anti-tumor activity in patients with advanced hepatocellular carcinoma randomized to receive treatment with sorafenib in combination with BBI608, sorafenib in combination with BBI503, or sorafenib alone; BBI608 and BBI503 would be administered at their respective RP2D dose levels for combination administration with sorafenib, which were determined during phase Ib. Secondary To determine the pharmacokinetic profile of BBI608 administered in Objectives: combination with sorafenib and of BBI503 administered in combination with sorafenib. -

Eltrombopag Versus Romiplostim in Treatment of Children With
www.nature.com/scientificreports OPEN Eltrombopag versus romiplostim in treatment of children with persistent or chronic immune Received: 5 July 2017 Accepted: 16 December 2017 thrombocytopenia: a systematic Published: xx xx xxxx review incorporating an indirect- comparison meta-analysis Jiaxing Zhang1,2, Yi Liang3, Yuan Ai4, Xiaosi Li5, Juan Xie2, Youping Li1, Wenyi Zheng6 & Rui He6 In absence of direct comparison, we conducted an indirect-comparison meta-analysis to evaluate the efcacy and safety of thrombopoietin-receptor agonists(TPO-RAs) in treatment of pediatric persistent or chronic immune thrombocytopenia(ITP). PubMed, Embase, Cochrane Library, Clinical Trials.gov, China National Knowledge Infrastructure, and Chinese Biomedical Literature Database were searched from their earliest records to May 2017. Randomized controlled trials comparing the TPO- RAs with placebo in pediatric ITP were included. Outcomes included overall response rate(primary), durable response, overall or clinically signifcant bleeding, the proportion of patients receiving rescue medication, and safety. Five randomized placebo-controlled studies(N = 261) were analyzed. The overall response[Risk Ratio(RR) 0.57, 95% confdence interval(CI) 0.21–1.56], the incidence of adverse events (RR 0.96, 95%CI 0.66–1.39), durable response(RR 2.48, 95%CI 0.31–19.97), and the proportion of patients receiving rescue treatment(RR 0.73, 95%CI 0.20–2.73) were similar between eltrombopag and romiplostim group. Nevertheless, eltrombopag might have lower risk of overall bleeding(RR 0.43, 95%CI 0.23–0.80) and clinically signifcant bleeding(RR 0.33, 95%CI 0.12–0.89) than romiplostim. This meta-analysis suggests that eltrombopag might be similar to romiplostim in efcacy and safety, but seems to reduce the risk of bleeding compared to romiplostim.