Pharmacokinetics of Polatuzumab Vedotin in Combination with R/G‑CHP in Patients with B‑Cell Non‑Hodgkin Lymphoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients
antibodies Review Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients Andrew T. Lucas 1,2,3,*, Ryan Robinson 3, Allison N. Schorzman 2, Joseph A. Piscitelli 1, Juan F. Razo 1 and William C. Zamboni 1,2,3 1 University of North Carolina (UNC), Eshelman School of Pharmacy, Chapel Hill, NC 27599, USA; [email protected] (J.A.P.); [email protected] (J.F.R.); [email protected] (W.C.Z.) 2 Division of Pharmacotherapy and Experimental Therapeutics, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 3 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-919-966-5242; Fax: +1-919-966-5863 Received: 30 November 2018; Accepted: 22 December 2018; Published: 1 January 2019 Abstract: The rapid advancement in the development of therapeutic proteins, including monoclonal antibodies (mAbs) and antibody-drug conjugates (ADCs), has created a novel mechanism to selectively deliver highly potent cytotoxic agents in the treatment of cancer. These agents provide numerous benefits compared to traditional small molecule drugs, though their clinical use still requires optimization. The pharmacology of mAbs/ADCs is complex and because ADCs are comprised of multiple components, individual agent characteristics and patient variables can affect their disposition. To further improve the clinical use and rational development of these agents, it is imperative to comprehend the complex mechanisms employed by antibody-based agents in traversing numerous biological barriers and how agent/patient factors affect tumor delivery, toxicities, efficacy, and ultimately, biodistribution. -

Australian Public Assessment for Polatuzumab Vedotin
Australian Public Assessment Report for Polatuzumab vedotin Proprietary Product Name: Polivy Sponsor: Roche Products Pty Ltd December 2019 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) • The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health and is responsible for regulating medicines and medical devices. • The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance) when necessary. • The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. • The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. • To report a problem with a medicine or medical device, please see the information on the TGA website <https://www.tga.gov.au>. About AusPARs • An Australian Public Assessment Report (AusPAR) provides information about the evaluation of a prescription medicine and the considerations that led the TGA to approve or not approve a prescription medicine submission. • AusPARs are prepared and published by the TGA. • An AusPAR is prepared for submissions that relate to new chemical entities, generic medicines, major variations and extensions of indications. • An AusPAR is a static document; it provides information that relates to a submission at a particular point in time. • A new AusPAR will be developed to reflect changes to indications and/or major variations to a prescription medicine subject to evaluation by the TGA. -

Antibody–Drug Conjugates
Published OnlineFirst April 12, 2019; DOI: 10.1158/1078-0432.CCR-19-0272 Review Clinical Cancer Research Antibody–Drug Conjugates: Future Directions in Clinical and Translational Strategies to Improve the Therapeutic Index Steven Coats1, Marna Williams1, Benjamin Kebble1, Rakesh Dixit1, Leo Tseng1, Nai-Shun Yao1, David A. Tice1, and Jean-Charles Soria1,2 Abstract Since the first approval of gemtuzumab ozogamicin nism of activity of the cytotoxic warhead. However, the (Mylotarg; Pfizer; CD33 targeted), two additional antibody– enthusiasm to develop ADCs has not been dampened; drug conjugates (ADC), brentuximab vedotin (Adcetris; Seat- approximately 80 ADCs are in clinical development in tle Genetics, Inc.; CD30 targeted) and inotuzumab ozogami- nearly 600 clinical trials, and 2 to 3 novel ADCs are likely cin (Besponsa; Pfizer; CD22 targeted), have been approved for to be approved within the next few years. While the hematologic cancers and 1 ADC, trastuzumab emtansine promise of a more targeted chemotherapy with less tox- (Kadcyla; Genentech; HER2 targeted), has been approved to icity has not yet been realized with ADCs, improvements treat breast cancer. Despite a clear clinical benefit being dem- in technology combined with a wealth of clinical data are onstrated for all 4 approved ADCs, the toxicity profiles are helping to shape the future development of ADCs. In this comparable with those of standard-of-care chemotherapeu- review, we discuss the clinical and translational strategies tics, with dose-limiting toxicities associated with the mecha- associated with improving the therapeutic index for ADCs. Introduction in antibody, linker, and warhead technologies in significant depth (2, 3, 8, 9). Antibody–drug conjugates (ADC) were initially designed to leverage the exquisite specificity of antibodies to deliver targeted potent chemotherapeutic agents with the intention of improving Overview of ADCs in Clinical Development the therapeutic index (the ratio between the toxic dose and the Four ADCs have been approved over the last 20 years (Fig. -

Federal Register Notice 5-1-2020 Pdf Icon[PDF – 358
Federal Register / Vol. 85, No. 85 / Friday, May 1, 2020 / Notices 25439 confidential by the respondent (5 U.S.C. schedules. Other than examination DEPARTMENT OF HEALTH AND 552(b)(4)). reports, it provides the only financial HUMAN SERVICES Current actions: The Board has data available for these corporations. temporarily revised the instructions to The Federal Reserve is solely Centers for Disease Control and the FR Y–9C report to accurately reflect responsible for authorizing, supervising, Prevention the revised definition of ‘‘savings and assigning ratings to Edges. The [CDC–2020–0046; NIOSH–233–C] deposits’’ in accordance with the Federal Reserve uses the data collected amendments to Regulation D in the on the FR 2886b to identify present and Hazardous Drugs: Draft NIOSH List of interim final rule published on April 28, potential problems and monitor and Hazardous Drugs in Healthcare 2020 (85 FR 23445). Specifically, the develop a better understanding of Settings, 2020; Procedures; and Risk Board has temporarily revised the activities within the industry. Management Information instructions on the FR Y–9C, Schedule HC–E, items 1(b), 1(c), 2(c) and glossary Legal authorization and AGENCY: Centers for Disease Control and content to remove the transfer or confidentiality: Sections 25 and 25A of Prevention, HHS. withdrawal limit. As a result of the the Federal Reserve Act authorize the ACTION: Notice and request for comment. revision, if a depository institution Federal Reserve to collect the FR 2886b chooses to suspend enforcement of the (12 U.S.C. 602, 625). The obligation to SUMMARY: The National Institute for six transfer limit on a ‘‘savings deposit,’’ report this information is mandatory. -

Polatuzumab Vedotin + Obinutuzumab + Lenalidomide in Patients with Relapsed/Refractory Follicular Lymphoma: Interim Analysis of a Phase Ib/II Trial
Polatuzumab vedotin + obinutuzumab + lenalidomide in patients with relapsed/refractory follicular lymphoma: interim analysis of a phase Ib/II trial Catherine Diefenbach,1 Brad Kahl,2 Lalita Banerjee,3 Andrew McMillan,4 Rod Ramchandren,5,6 Fiona Miall,7 Javier Briones,8 Raul Cordoba,9 Eva Maria Gonzalez-Barca,10 Carlos Panizo,11 Jamie Hirata,12 Naomi Chang,13 Lisa Musick,12 Pau Abrisqueta14 1Perlmutter Cancer Center at NYU Langone Health, New York, NY, USA; 2Division of Oncology, Washington University, St Louis, MO, USA; 3Oncology Centre, Maidstone and Tunbridge Wells NHS Trust, Kent, UK; 4Centre for Clinical Haematology, Nottingham University Hospitals NHS Trust, Nottingham, UK; 5Division of Oncology, University of Tennessee, Knoxville, TN, USA; 6Barbara Ann Karmanos Cancer Institute, Detroit, MI, USA; 7Department of Haematology, University Hospitals of Leicester NHS Trust, Leicester, UK; 8Department of Hematology, Hospital Santa Creu i Sant Pau, Barcelona, Spain; 9Fundación Jiménez Díaz, Madrid, Spain; 10Institut Català D'Oncologia, Barcelona, Spain; 11Clínica Universidad de Navarra, Pamplona, Spain; 12Genentech, Inc., South San Francisco, CA, USA; 13F. Hoffmann-La Roche Ltd, Mississauga, Canada; 14Department of Hematology, Vall d'Hebron Institute of Oncology (VHIO), Hospital Universitari Vall d'Hebron, Barcelona, Spain 1 Catherine Diefenbach http://bit.ly/2JjV5Jn Disclosures CD holds stock in Gilead Sciences; has a consulting/advisory role for Seattle Genetics, Bayer, Bristol-Myers Squibb, Genentech/Roche, and Merck; has received research funding from Seattle Genetics, Genentech, Incyte, LAM Therapeutics, Merck, Bristol-Myers Squibb, Millennium, and MEI Pharma. BK has a consulting/advisory role for Roche, Genentech, Celgene, AbbVie, Pharmacyclics, and Acerta Pharma; has received research funding from Genentech, Acerta Pharma, and BeiGene; has provided expert testimony for Genentech. -

A Phase Ib/II Study Evaluating the Safety and Efficacy Of
Official Title: A Phase Ib/II Study Evaluating the Safety and Efficacy of Obinutuzumab in Combination With Atezolizumab Plus Polatuzumab Vedotin in Patients With Relapsed or Refractory Follicular Lymphoma and Rituximab in Combination With Atezolizumab Plus Polatuzumab Vedotin in Patients With Relapsed or Refractory Diffuse Large B-Cell Lymphoma NCT Number: NCT02729896 Document Date: Protocol Version 8: 07-November-2018 PROTOCOL TITLE: A PHASE Ib/II STUDY EVALUATING THE SAFETY AND EFFICACY OF OBINUTUZUMAB IN COMBINATION WITH ATEZOLIZUMAB PLUS POLATUZUMAB VEDOTIN IN PATIENTS WITH RELAPSED OR REFRACTORY FOLLICULAR LYMPHOMA AND RITUXIMAB IN COMBINATION WITH ATEZOLIZUMAB PLUS POLATUZUMAB VEDOTIN IN PATIENTS WITH RELAPSED OR REFRACTORY DIFFUSE LARGE B-CELL LYMPHOMA PROTOCOL NUMBER: BO29561 VERSION NUMBER: 8 EUDRACT NUMBER: 2015-004845-25 IND NUMBER: 128036 TEST PRODUCT: Obinutuzumab (RO5072759) Rituximab (RO0452294) Atezolizumab (RO5541267) Polatuzumab vedotin (RO5541077) MEDICAL MONITOR: , Ph.D. SPONSOR: F. Hoffmann-La Roche Ltd DATE FINAL: Version 1: 12 November 2015 DATES AMENDED: Version 2: 14 January 2016 Version 3: 28 June 2016 Version 4: 17 November 2016 Version 5: 4 May 2017 Version 6: 21 December 2017 Version 7: 1 May 2018 Version 8: See electronic date stamp below. PROTOCOL AMENDMENT APPROVAL Approver's Name Title Date and Time (UTC) Company Signatory 07-Nov-2018 02:00:10 CONFIDENTIAL This clinical study is being sponsored globally by F. Hoffmann-La Roche Ltd of Basel, Switzerland. However, it may be implemented in individual countries by Roche’s local affiliates, including Genentech, Inc. in the United States. The information contained in this document, especially any unpublished data, is the property of F. -

Antibody–Drug Conjugates: the Last Decade
pharmaceuticals Review Antibody–Drug Conjugates: The Last Decade Nicolas Joubert 1,* , Alain Beck 2 , Charles Dumontet 3,4 and Caroline Denevault-Sabourin 1 1 GICC EA7501, Equipe IMT, Université de Tours, UFR des Sciences Pharmaceutiques, 31 Avenue Monge, 37200 Tours, France; [email protected] 2 Institut de Recherche Pierre Fabre, Centre d’Immunologie Pierre Fabre, 5 Avenue Napoléon III, 74160 Saint Julien en Genevois, France; [email protected] 3 Cancer Research Center of Lyon (CRCL), INSERM, 1052/CNRS 5286/UCBL, 69000 Lyon, France; [email protected] 4 Hospices Civils de Lyon, 69000 Lyon, France * Correspondence: [email protected] Received: 17 August 2020; Accepted: 10 September 2020; Published: 14 September 2020 Abstract: An armed antibody (antibody–drug conjugate or ADC) is a vectorized chemotherapy, which results from the grafting of a cytotoxic agent onto a monoclonal antibody via a judiciously constructed spacer arm. ADCs have made considerable progress in 10 years. While in 2009 only gemtuzumab ozogamicin (Mylotarg®) was used clinically, in 2020, 9 Food and Drug Administration (FDA)-approved ADCs are available, and more than 80 others are in active clinical studies. This review will focus on FDA-approved and late-stage ADCs, their limitations including their toxicity and associated resistance mechanisms, as well as new emerging strategies to address these issues and attempt to widen their therapeutic window. Finally, we will discuss their combination with conventional chemotherapy or checkpoint inhibitors, and their design for applications beyond oncology, to make ADCs the magic bullet that Paul Ehrlich dreamed of. Keywords: antibody–drug conjugate; ADC; bioconjugation; linker; payload; cancer; resistance; combination therapies 1. -

New Drug Updates Brendan Mangan, Pharmd Clinical Pharmacy Specialist Hospital of the University of Pennsylvania
11/9/2020 Disclosures • There are no relevant financial interests to disclose for myself or my spouse/partner from within the last 12 months New Drug Updates Brendan Mangan, PharmD Clinical Pharmacy Specialist Hospital of the University of Pennsylvania 1 2 Objectives New Drugs Explain the pharmacology of each new medication Malignant Hematology Medical Oncology Define indications, adverse effects and pertinent drug interactions Outline supportive care measures and clinical pearls Selinexor Tazemotostat Isatuximab-irfc Avapritinib Discuss the results of clinical trials and place in therapy Belantamab mafodotin-blmf Pexidartinib Fedratinib Entrectinib Polatuzumab vedotin-piiq Tafasitamab-cxix Zanubrutinib 3 4 Selinexor (XPOVIO®) Approval: July 3, 2019 Novel agent Exportin 1 inhibitor ▫ Reversibly inhibits nuclear export of tumor suppressor proteins, growth regulators, and mRNAs of oncogenic proteins XPOVI™ [Prescribing Information] Newton, MA. Karyopharm Therapeutics. 2019. Picture: xpovio.com 5 6 1 11/9/2020 Selinexor Selinexor Indication Adverse Effects Clinical Pearls • In combination with dexamethasone for relapse refractory multiple myeloma after failing 4 prior therapies Thrombocytopenia (74%) GCSF and prophylactic antimicrobials Recommended Neutropenia (34%) Prophylactic anti-emetics First Reduction Second Reduction Third Reduction Starting Dosage Nausea (72%)/Vomiting (41%) IV fluids and electrolyte repletion may be Diarrhea (44%) warranted monitor closely 80 mg Discontinue Days 1 and 3 of each Anorexia (53%)/Weight loss (47%) Correct sodium levels for concurrent 100 mg once weekly 80 mg once weekly 60 mg once weekly week (160 mg weekly Hyponatremia (39%) hyperglycemia (>150 mg/dL) total) Infections (52%) TPO agonist may be warranted for Neurological toxicity (30%) thrombocytopenia GCSF = Granulocyte colony-stimulating factor XPOVI™ [Prescribing Information] Newton, MA. -

Immunotherapies Shape the Treatment Landscape for Hematologic Malignancies Jane De Lartigue, Phd
Feature Immunotherapies shape the treatment landscape for hematologic malignancies Jane de Lartigue, PhD he treatment landscape for hematologic of TIL therapy has been predominantly limited to malignancies is evolving faster than ever melanoma.1,3,4 before, with a range of available therapeutic Most recently, there has been a substantial buzz Toptions that is now almost as diverse as this group around the idea of genetically engineering T cells of tumors. Immunotherapy in particular is front and before they are reintroduced into the patient, to center in the battle to control these diseases. Here, increase their anti-tumor efficacy and minimize we describe the latest promising developments. damage to healthy tissue. This is achieved either by manipulating the antigen binding portion of the Exploiting T cells T-cell receptor to alter its specificity (TCR T cells) The treatment landscape for hematologic malig- or by generating artificial fusion receptors known as nancies is diverse, but one particular type of therapy chimeric antigen receptors (CAR T cells; Figure 1). has led the charge in improving patient outcomes. The former is limited by the need for the TCR to be Several features of hematologic malignancies may genetically matched to the patient’s immune type, make them particularly amenable to immunother- whereas the latter is more flexible in this regard and apy, including the fact that they are derived from has proved most successful. corrupt immune cells and come into constant con- CARs are formed by fusing part of the single- tact with other immune cells within the hemato- chain variable fragment of a monoclonal antibody poietic environment in which they reside. -

Event Analysis of Polatuzumab Vedotin‐Induced Peripheral
Citation: CPT Pharmacometrics Syst. Pharmacol. (2017) 6, 401–408; doi:10.1002/psp4.12192 VC 2017 ASCPT All rights reserved ORIGINAL ARTICLE Time-to-Event Analysis of Polatuzumab Vedotin-Induced Peripheral Neuropathy to Assist in the Comparison of Clinical Dosing Regimens DLu1*, WR Gillespie2, S Girish1, P Agarwal1,CLi1, J Hirata1, Y-W Chu1, M Kagedal1, L Leon1, V Maiya1 and JY Jin1 Polatuzumab vedotin, an antibody-drug conjugate containing monomethyl auristatin E, was associated with an incidence of grade 2 peripheral neuropathy (PN) of 55–72% in patients with indolent non-Hodgkin lymphoma in a phase II study, when dosed 1.8–2.4 mg/kg every 3 weeks until progression or for a maximum of 17 cycles. To quantify the correlation of conjugate exposure and treatment duration with PN risk, a time-to-event model was developed using data from phase I and II studies. The model suggested that PN risk increased with conjugate exposure and treatment cycles, and a trend for increased risk with body weight and albumin concentration. When capping the treatment duration to six to eight cycles, the risk ratio of a dose of 2.4 mg/kg vs. 1.8 mg/kg was 1.29; the predicted incidence of grade 2 PN at 1.8–2.4 mg/kg dose levels was 17.8–37.2%, which is comparable with other antimicrotubule agents for lymphoma treatment. CPT Pharmacometrics Syst. Pharmacol. (2017) 6, 401–408; doi:10.1002/psp4.12192; published online 8 March 2017. Study Highlights WHAT IS THE CURRENT KNOWLEDGE ON THE WHAT THIS STUDY ADDS TO OUR KNOWLEDGE TOPIC? þ Pola-induced PN increased with conjugate exposure þ The PN risk factors related to patient baseline char- and treatment duration. -

Antibodies for the Treatment of Brain Metastases, a Dream Or a Reality?
pharmaceutics Review Antibodies for the Treatment of Brain Metastases, a Dream or a Reality? Marco Cavaco, Diana Gaspar, Miguel ARB Castanho * and Vera Neves * Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Av. Prof. Egas Moniz, 1649-028 Lisboa, Portugal * Correspondence: [email protected] (M.A.R.B.C.); [email protected] (V.N.) Received: 19 November 2019; Accepted: 28 December 2019; Published: 13 January 2020 Abstract: The incidence of brain metastases (BM) in cancer patients is increasing. After diagnosis, overall survival (OS) is poor, elicited by the lack of an effective treatment. Monoclonal antibody (mAb)-based therapy has achieved remarkable success in treating both hematologic and non-central-nervous system (CNS) tumors due to their inherent targeting specificity. However, the use of mAbs in the treatment of CNS tumors is restricted by the blood–brain barrier (BBB) that hinders the delivery of either small-molecules drugs (sMDs) or therapeutic proteins (TPs). To overcome this limitation, active research is focused on the development of strategies to deliver TPs and increase their concentration in the brain. Yet, their molecular weight and hydrophilic nature turn this task into a challenge. The use of BBB peptide shuttles is an elegant strategy. They explore either receptor-mediated transcytosis (RMT) or adsorptive-mediated transcytosis (AMT) to cross the BBB. The latter is preferable since it avoids enzymatic degradation, receptor saturation, and competition with natural receptor substrates, which reduces adverse events. Therefore, the combination of mAbs properties (e.g., selectivity and long half-life) with BBB peptide shuttles (e.g., BBB translocation and delivery into the brain) turns the therapeutic conjugate in a valid approach to safely overcome the BBB and efficiently eliminate metastatic brain cells. -
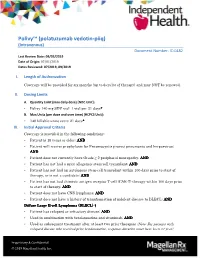
Polivy™ (Polatuzumab Vedotin-Piiq) (Intravenous) Document Number: IC-0482 Last Review Date: 09/03/2019 Date of Origin: 07/01/2019 Dates Reviewed: 07/2019, 09/2019
Polivy™ (polatuzumab vedotin-piiq) (Intravenous) Document Number: IC-0482 Last Review Date: 09/03/2019 Date of Origin: 07/01/2019 Dates Reviewed: 07/2019, 09/2019 I. Length of Authorization Coverage will be provided for six months (up to 6 cycles of therapy) and may NOT be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • Polivy 140 mg SDV vial: 1 vial per 21 days**** B. Max Units (per dose and over time) [HCPCS Unit]: • 140 billable units every 21 days**** III. Initial Approval Criteria Coverage is provided in the following conditions: • Patient is 18 years or older; AND • Patient will receive prophylaxis for Pneumocystis jiroveci pneumonia and herpesvirus; AND • Patient does not currently have Grade ≥ 2 peripheral neuropathy; AND • Patient has not had a prior allogeneic stem-cell transplant; AND • Patient has not had an autologous stem-cell transplant within 100 days prior to start of therapy, or is not a candidate; AND • Patient has not had chimeric antigen receptor T-cell (CAR-T) therapy within 100 days prior to start of therapy; AND • Patient does not have CNS lymphoma; AND • Patient does not have a history of transformation of indolent disease to DLBCL; AND Diffuse Large BB----cellcellcellcell Lymphoma ((DLBCDLBCDLBCL)L)L)L) ††† • Patient has relapsed or refractory disease; AND • Used in combination with bendamustine and rituximab; AND • Used as subsequent treatment after at least two prior therapies (Note: For patients with relapsed disease who received prior bendamustine, response duration must have been >1 year) Proprietary & Confidential © 2019 Magellan Health, Inc. ††† FDA Approved Indication(s), ‡‡‡ Compendia Recommended Indication(s) IV.