Deep Phenotyping of Myalgic Encephalomyelitis/Chronic Fatigue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pdf/1744-9081-7-46.Pdf Tröm, B
World Journal of Neuroscience, 2012, 2, 113-118 WJNS http://dx.doi.org/10.4236/wjns.2012.22016 Published Online May 2012 (http://www.SciRP.org/journal/wjns/) Changes in reaction time, coefficient of variance of reaction time, and autonomic nerve function in the mental fatigue state caused by long-term computerized Kraepelin test workload in healthy volunteers Daisuke Kuratsune1, Seiki Tajima2, Junichi Koizumi3, Kouzi Yamaguti4, Tetsuya Sasabe4, Kei Mizuno5,6, Masaaki Tanaka6, Naoko Okawa7, Hideki Mito7, Hirokazu Tsubone8, Yasuyoshi Watanabe5,6, Masayasu Inoue1, Hirohiko Kuratsune4,6,7,8 1Department of Biochemistry and Molecular Pathology, Graduate School of Medicine, Osaka City University, Osaka, Japan 2Hyogo Children’s Sleep and Development Medical Research Center, Kobe, Japan 3Division of Materials Science and Chemical Engineering, Yokohama National University, Yokohama, Japan 4Clinical Center for Fatigue Science, Graduate School of Medicine, Osaka City University, Osaka, Japan 5RIKEN, Center for Molecular Imaging Science, MI R&D Center, Kobe, Japan 6Department of Physiology, Graduate School of Medicine, Osaka City University, Osaka, Japan 7Faculty of Health Science for Welfare, Kansai University of Welfare Sciences, Kasiwara, Japan 8Department of Comparative Pathophysiology, Veterinary Medical Sciences, Graduate School of Agricultural & Life Science, The University of Tokyo, Tokyo, Japan Email: [email protected] Received 25 November 2011; revised 17 January 2012; accepted 16 February 2012 ABSTRACT ing a long-term CKT workload is a good mental fa- tigue model to provide much information about the Fatigue is a common sense caused by crushing labor, fatigue state simultaneously, and the increase of RT, stressful social events and various illnesses. It is usually CV, and proportion of sympathetic activity (LF/HF) judged by their subjective symptoms, but it should be are associated with mental fatigue state. -
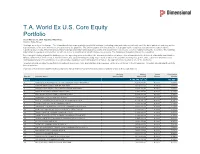
T.A. World Ex U.S. Core Equity Portfolio As of March 31, 2021 (Updated Monthly) Source: State Street Holdings Are Subject to Change
T.A. World Ex U.S. Core Equity Portfolio As of March 31, 2021 (Updated Monthly) Source: State Street Holdings are subject to change. The information below represents the portfolio's holdings (excluding cash and cash equivalents) as of the date indicated, and may not be representative of the current or future investments of the portfolio. The information below should not be relied upon by the reader as research or investment advice regarding any security. This listing of portfolio holdings is for informational purposes only and should not be deemed a recommendation to buy the securities. The holdings information below does not constitute an offer to sell or a solicitation of an offer to buy any security. The holdings information has not been audited. By viewing this listing of portfolio holdings, you are agreeing to not redistribute the information and to not misuse this information to the detriment of portfolio shareholders. Misuse of this information includes, but is not limited to, (i) purchasing or selling any securities listed in the portfolio holdings solely in reliance upon this information; (ii) trading against any of the portfolios or (iii) knowingly engaging in any trading practices that are damaging to Dimensional or one of the portfolios. Investors should consider the portfolio's investment objectives, risks, and charges and expenses, which are contained in the Prospectus. Investors should read it carefully before investing. Your use of this website signifies that you agree to follow and be bound by the terms and conditions -

Measurement of Comparative Social Attitudes: from a Perspective of Japan and Osaka
R. L. R. 93 Measurement of Comparative Social Attitudes: From a Perspective of Japan and Osaka MURAKAMI Hiroshi* 1. Uniqueness of Social Attitude in Japan 1-2. Osaka: Right-wing Populism and ʻCasino Expoʼ 2025 2. What Criteria are Useful for International Comparison? 3. Empirical Research Results in Japan Appendix: ʻResource Supplement Modelʼ for Democracy 1. Uniqueness of Social Attitude in Japan In the field of comparative social and political attitudes both similar and unique aspects are found among countries, and to display this many models have been invented. In general Japanese and German people have been both regarded as diligent and ori- ented to order and rules, but there are also differences. - In the 1930s, dictatorship arose in several countries, gaining wide support of the nation with propaganda and violence. But resistance to and escape from dictatorship spread in Germany and Italy, not in Japan. (And later in Spain, Chile, South Korea, Taiwan etc., and not in North Korea.) - In the Second World War, Japanese soldiers and commanders obeyed to even the orders of suicide attack (Tokkou) and orders to fight until the last man without surrender (Gyokusai), and sometimes requested Japanese civilians to follow in Saipan and Okinawa. Such orders were too authoritative and objectively irrational, although subjectively heroic or useful to postpone the final surrender of the empire. (This delay induced two socialist countries in East Asia)1). - In the postwar period, Germany established a pluralistic, well-balanced party system from conservatives to social democrats, even under the pressure of anti-communism doc- * Professor (Public Administration/ Political Science), Faculty of Law, Ritsumeikan University. -

10. Legal Philosophy
DEVELOPMENTS IN 2009 ― ACADEMIC SOCIETIES 105 Hiroshi Takahashi(Professor, Kobe University). (2)“Development of Date Archives and its Significance for Socio-legal Studies” Iwao Sato(Professor, University of Tokyo). Articles: (1)“The Disparities of the Responses to the Victims of Domestic Violence among the Local Governments in Japan” Akiko Tejima(Graduate Student, Kyoto Women’s University, Lecturer, Kobe College). (2)“Significances and Limitations in Legal Remedies toward Past Injustice” Kumiko Tsuchida(Researcher, Tohoku University Global COE Program). (3)“Exploring Japanese Cop Culture through Questionnaire Survey” Naoko Yoshida(Research Visitor, Meiji University). 10. Legal Philosophy The Japan Association for Legal Philosophy held its 2009 General Meeting at Kansai University on November 14 and 15, 2009. Main Theme: Risk Society and Law Presentations on Each Theme: Section A: (1)“Can Hume be a Contract Theorist?: Through Examining David Gothie’s Analysis of Hume” Takahumi Nakamura(Lecturer, Kagoshima National College of Technology) (2)“Review on the Theory of Immigrants’ Justice: Examining Joseph Carens’ Open Borders Theory” Seiko Urayama(Special Researcher, Japan Society for the Promotion 106 WASEDA BULLETIN OF COMPARATIVE LAW Vol. 29 of Science) (3)“Manners of Criticizing Culture: Through Considering Joseph Carens’ Theory” Takayuki Kawase(Researcher, Kyoto University) (4)“The Limit of the Harm Principle: Reconsidering “the Compulsion of Morals by Law” Mayu Miyazaki(Research Associate, Tamagawa University) Section B: (1)“The Method -
8Th Student Formula SAE Competition of Japan Official Progrum
Official Program 8th Student Formula SAE Competition of JAPAN Monozukuri Design Competition Sat. 2010 9.7 Tue. -11 Ogasayama Sports Park (ECOPA) Organizer JSAE (JSA E ) Society of Automotive Engineers of Japan, Inc. ECOPA Contents Congrtultory Messge / President’s Messge .... 1 Outline of the Competition ........................................ 2 Schedule of Events .................................................... 4 Entry Tems ................................................................. 5 Sponsors ................................................................ 6 wrds ................................................................... 7 Orgnizer / Support / Committee Members ...... 8 Competition Stffs ................................................. 9 Tem Informtion(Vehicle Specifictions) .... 10 〜 17 Tem Informtion(Members nd Sponsors) ... 18 〜38 Event Sfety ............................................................. 39 Congratulatory Message /President’s Message Congratulatory Message 8th Student Formula SAE Competition of Japan Please allow me to take this opportunity to offer my warmest congratulations on the holding of the 8th Student Formula SAE Competition of Japan. Science and technology play a major role in solving the various problems that human society is facing and helps us to realize safe and productive lives while promoting economic growth. Japan is a country that does not possess a large amount of natural resources, so it is our people and knowledge that will support our future development. Strengthening our -

90005396.Pdf
Kobe University Repository : Kernel タイトル Polyphagous koinobiosis: the biology and biocontrol potential of a Title braconid endoparasitoid of exophytic caterpillars 著者 Maeto, Kaoru Author(s) 掲載誌・巻号・ページ Applied Entomology and Zoology,53(4):433-446 Citation 刊行日 2018-11 Issue date 資源タイプ Journal Article / 学術雑誌論文 Resource Type 版区分 author Resource Version © The Japanese Society of Applied Entomology and Zoology 2018. 権利 This is a post-peer-review, pre-copyedit version of an article published Rights in Applied Entomology and Zoology. The final authenticated version is available online at: https://doi.org/10.1007/s13355-018-0581-9 DOI 10.1007/s13355-018-0581-9 JaLCDOI URL http://www.lib.kobe-u.ac.jp/handle_kernel/90005396 PDF issue: 2021-09-30 Applied Entomology and Zoology (2018) 53:433–446 DOI: 10.1007/s13355-018-0581-9 Polyphagous koinobiosis: The biology and biocontrol potential of a braconid endoparasitoid of exophytic caterpillars Kaoru Maeto1 ✉ Kaoru Maeto [email protected] 1 Graduate School of Agricultural Science, Kobe University, 1-1 Rokkodai, Nada, Kobe 657-8501, Japan Abstract Polyphagous koinobiosis might be a novel perspective to help elucidate the evolution of the physiological and ecological traits of parasitoid wasps and determine their use as biocontrol agents. The euphorine braconid Meteorus pulchricornis is a polyphagous koinobiont endoparasitoid of exophytic caterpillars from 15 families within 10 lepidopteran superfamilies. Here, the biology of this common but enigmatic parasitoid wasp is reviewed. The unique cocoon suspension system of M. pulchricornis protects it against predators during and after cocoon spinning. This structural cocoon protection method, as well as robust immune suppression mechanism, likely enables its very wide host range. -

9 Th Student Formula SAE Competition of JAPAN
Official Program 9 th Student FormulaFo SAE Competitionp of JAPAN Student Formula 9th SAE Competition of JAPAN MonozukuriMonozukuri DesigDesign CCompetitionompet . FRI MON Ogasayama Sports Park (ECOPA) Organizer JSAE (JSAE) Society of Automotive Engineers of Japan, Inc. Contents Congratulatory Message/President’s Message ..... 1 Organizer/Support/Committee Members ................... 8 Outline of Events ............................................................................ 2 Competition Staffs ........................................................................ 9 Schedule of Events ...................................................................... 4 Team Information(Vehicle Specifications) ....... 10~17 Entry Teams ...................................................................................... 5 Team Information(Members and Sponsors) ... 18~38 Sponsors .............................................................................................. 6 Event Safety .................................................................................... 39 Awards .................................................................................................. 7 Congratulatory Message / President’s Message Congratulations on the 9th Student Formula SAE Competition of Japan Please allow me to take this opportunity to offer my warmest congratulations on the holding of the 9th Student Formula SAE Competition of Japan. The Great East Japan Earthquake that occurred on March 11 caused unprecedented damage to this country. I would -
Official Program Student Formula PAN SAE Competition of JA Monozukuri Design Competition Ed at S 2009 9.9 W -12
Official Program Student Formula PAN SAE Competition of JA Monozukuri Design Competition ed at S 2009 9.9 W -12 Organizer OGASAYAMA JSAE ECOPA SPORTS PARK Society of Automotive Engineers of Japan, Inc. (JSA E ) Contents Congratulatory Message / President’s message ..... 1 Concept of the Competition ...................................... 2 Outline of the Competition ........................................ 3 Schedule of Events ................................................... 4 Entry Team ................................................................ 5 Sponsors ................................................................... 6 wards ...................................................................... 7 Organisers / Sponsors / Co-Sponsors / Committee Member .......................... 8 Competition staff ....................................................... 9 Team Information(Vehicle Specifications) ... 10 〜 13 Team Information(Members & Sponsors) ..... 14 〜 32 Event Safety ........................................................... 33 Congratulatory Message/President’s Message Congratulatory Message 7th Student Formula SAE Competition of Japan Please allow me to take this opportunity to offer my warmest congratulations on the holding of the 7th Student Formula SAE Competition of Japan. In the rapidly changing world of the 21st century, activities for nurturing and retaining the next generation of engineers are of critical importance for Japan to fully develop its competitive strength on the international stage and sustain its -

Program 1..154
The 90th Annual Meeting of CSJ Program 4S1- 10 Special Program Lecture Synthesis and optical properties of Room S1 inorganic-organic nanocomposite materials based on mesoporous materials (Frontier Research Center, Canon Inc.)MIYATA, Hirokatsu(12:05~ 12:10) Bldg.21 203 4S1- 11 Special Program Lecture Control of aggregation structure of photofunctional organic molecules using one-dimensional inorganic polymer (Grad. Sch. Sci., Eng., Kagoshima Univ.)KANEKO, Yoshiro(12:10~ Quantitative analytical researches on multi- 12:15) 4S1- 12 Special Program Lecture Preparation of Inorganic Layered functional foods Compounds for Selective Adsorption of an Organic Molecule(Fac. Eng., ) ( ~ ) Sunday, March 28, PM Shinshu Univ. OKADA, Tomohiko 12:15 12:20 4S1- 13 Special Program Lecture Highly Functional Low-Dimen- Chair: TAMIYA, Eiichi(13:30~15:00) sional Compouds(Grad. Sch. Sci., Kyoto Univ.)KAGEYAMA, Hiroshi 3S1- 01 Opening remarks(Kyoto Pref. Univ. of Med.)YOSHIKAWA, (12:20~12:25) Toshikazu(13:30~13:40) 4S1- 14 Panel Discussion (12:25~12:30) 3S1- 02 Special Lecture Current situation of the researches onmulti- functional foods(National Food Research Institute, NARO)HINO, Akihiro(13:40~14:20) New energy innovation and material produc- 3S1- 03 Special Lecture Food Factors in Medicine(Kyoto Pref. Univ. tion based on the artificial photosynthesis of Med.)YOSHIKAWA, Toshikazu(14:20~15:00) Monday, March 29, PM Chair: HINO, Akihiro(15:00~17:00) Chair: NANGO, Mamoru(13:30~15:00) 3S1- 04 Special Lecture Development of Functional Foods(Institute 4S1- 15 Introduction(Fac. Eng, Oita Univ.)AMAO, Yutaka(13:30~ for Health Care Science, Suntory Wellness Limited.)KISO, Yoshinobu 13:40) (15:00~15:40) 4S1- 16 Special Program Lecture Carbon Dioxide Fixation Based on 3S1- 05 Special Lecture Future contributions of artificial digestion, the Artificial Photosynthesis System(Fac. -

Association of Monoamine-Synthesizing Genes with the Depression Tendency and Personality in Chronic Fatigue Syndrome Patients
Life Sciences 92 (2013) 183–186 Contents lists available at SciVerse ScienceDirect Life Sciences journal homepage: www.elsevier.com/locate/lifescie Association of monoamine-synthesizing genes with the depression tendency and personality in chronic fatigue syndrome patients Sanae Fukuda a,b, Mieko Horiguchi c,d, Kouzi Yamaguti e,f, Yasuhito Nakatomi b,e, Hirohiko Kuratsune e,f,g, Hiroshi Ichinose d, Yasuyoshi Watanabe b,f,⁎ a Department of Medical Science on Fatigue, Osaka City University, Graduate School of Medicine, Osaka, Japan b Center for Molecular Imaging Science, RIKEN, Kobe, Hyogo, Japan c Department of Domestic Science, Junior College Division, Otsuma Women's University, Tokyo, Japan d Graduate School of Bioscience and Biotechnology, Tokyo Institute of Technology, Yokohama, Japan e Department of Metabolism, Endocrinology and Molecular Medicine, Fatigue Clinical Center, Osaka City University Graduate School of Medicine, Osaka, Japan f Department of Physiology, Osaka City University Graduate School of Medicine, Osaka, Japan g Department of Health Welfare, Kansai Welfare University, Kashiwara, Japan article info abstract Article history: Aims: Tyrosine hydroxylase (TH) and GTP cyclohydrolase I (GCH) are the rate-limiting enzymes for the Received 19 June 2012 biosynthesis of catecholamines and tetrahydrobiopterin (BH4), respectively. Since catecholamines and BH4 Accepted 20 November 2012 are thought to be involved in the pathophysiology of CFS, we explored the genetic factors that influence CFS development and examined the possible association between the SNPs of the TH and GCH genes and Keywords: the various characteristics of CFS patients. Personality Main methods: After drawing venous blood from CFS patients and controls, genomic DNA was then extracted Chronic fatigue syndrome from whole blood in accordance with standard procedures. -

Japan's Signals Intelligence
The Nautilus Institute for Security and Sustainability Japan’s Signals Intelligence (SIGINT) Ground Stations: A Visual Guide Desmond Ball and Richard Tanter Nautilus Institute for Security and Sustainability Special Report 6 August 2015 Summary This is a study of Japan’s ground-based signals intelligence (SIGINT) stations, the 17 (soon to be 19) major facilities that intercept, monitor, collect, process and analyse foreign electronic signals. Official statements convey nothing of the scale or detail of the Japanese SIGINT effort, which is probably the third or fourth largest SIGINT establishment in the world. These Japanese ground signals interception and location facilities are integrated with its air and missile defence radar facilities. Together with Japan’s own long-range underwater surveillance systems, and combined with the Japan-based US parallel air, ground and underwater surveillance systems, they take Japan a very long way towards its stated aim to ensure information supremacy in the region. As potentially lucrative targets in the event of war, destruction of these important but vulnerable facilities could alter escalation dynamics in such a way that the widespread assumption that a Japan-China armed conflict could be controlled before substantial escalation may not hold true. This report is a visual guide, hopefully making it easier for those come after us to identify what they are seeing. Similar and comparable systems are critical to the strategic planning of all countries with substantial military capacities – or ambitions. Accordingly an understanding of the Japanese ground stations, their physical characteristics, and the logic of their deployment may be of use in understanding non-Japanese systems. -

The Ceramic Society of Japan Annual Meeting 2015 Program
Please note, Almost all presentation will be given in Japanese. ○=Speaker The symbol that attached to the end of the presentation number The Ceramic Society of Japan A=Award lecture F=Frontiers of industrial research Annual Meeting 2015 M=Mixing session S=Elemental strategy Program Genera(l Presentation ₁₀ min. Discussion ₄ min. Alternation ₁ min. ) Award/Invited( Presentation ₂₅ min. Discussion ₄ min. Alternation ₁ min. ) ★★ March 18 (Wed) (Room A) ★★ Glass and photonic materials / 構造解析・ガラス形成 (13:00)(Chairman 増野敦信) ₁A₁₇ Structure of Bi₂O₃-GeO₂ glasses (Japan Synchrotron Radiation Research Institute)○Shinji Kohara・Koji Ohara・Akihiko Fujiwara・(Okayama University) Yasuhiko Benino ₁A₁₈ Functional Complex Point Defect Structure in a Huge Size Mismatch System (University of Tokyo)○Ryo Ishikawa・Naoya Shibata・Yuichi Ikuhara・(Kyoto University) Fumiyasu Oba・Isao Tanaka・ (NIMS) Takashi Taniguchi・(Monash University) Scott D. Findlay (13:30)(Chairman 小原慎司) ₁A₁₉ Containerless solidification of undercooled SrO–Al₂O₃ binary melts (The University of Tokyo)○Atsunobu Masuno・Katsuyoshi Kato・Hiroyuki Inoue ₁A₂₀ Fabrication of dense sintered body from low-melting Na₂O-Al₂O₃-P₂O₅ glass powder through oxygen-supplied hot isostatic pressing and its evaluation (Sophia University)○Shiori Hirano・(Delft University of Technology) Hubertus T. Hintzen・(Sophia University) Kiyoshi Itatani ₁A₂₁ Thermal stability and chemical durability of BaO-FeOx-P₂O₅ glasses (Ehime University)○Naoto Kitamura・Akira Saitoh・Hiromichi Takebe・(Japan Atomic Energy Agency) Ippei Amamoto・ Hidekazu