Delaware and Vermont Network Adequacy Regulations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
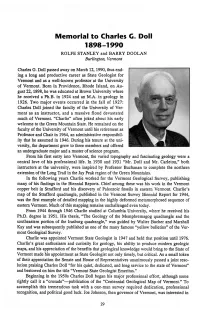
Memorial to Charles C. Doll 1898-1990 ROLFE STANLEY and BARRY DOOLAN Burlington, Vermont
Memorial to Charles C. Doll 1898-1990 ROLFE STANLEY and BARRY DOOLAN Burlington, Vermont Charles G. Doll passed away on March 12,1990, thus end ing a long and productive career as State Geologist for Vermont and as a well-known professor at the University of Vermont. Born in Providence, Rhode Island, on Au gust 22,1898, he was educated at Brown University where he received a Ph.B. in 1924 and an M.A. in geology in 1926. Two major events occurred in the fall of 1927: Charles Doll joined the faculty of the University of Ver mont as an instructor, and a massive flood devastated much of Vermont. “Charlie” often joked about his early welcome to the Green Mountain State. He remained on the faculty of the University of Vermont until his retirement as Professor and Chair in 1964, an administrative responsibil ity that he assumed in 1946. During his tenure at the uni versity, the department grew to three members and offered an undergraduate major and a master of science program. From his first entry into Vermont, the varied topography and fascinating geology were a central love of his professional life. In 1930 and 1931 “Mr. Doll and Mr. Carleton,” both instructors at the university, were inspired by Professor Buchanan to complete the northern extension of the Long Trail in the Jay Peak region of the Green Mountains. In the following years Charlie worked for the Vermont Geological Survey, publishing many of his findings in the Biennial Reports. Chief among these was his work in the Vermont copper belt in Strafford and his discovery of Paleozoic fossils in eastern Vermont. -

Pennsylvania Passes an Act for the Gradual Abolition of Slavery, Freeing Future Children of Slaves
1777: Constitution of the Vermont Republic bans slavery. 1780: Pennsylvania passes An Act for the Gradual Abolition of Slavery, freeing future children of slaves. Those born prior to the Act remain enslaved for life. The Act becomes a model for other Northern states. Last slaves freed 1847. 1783: Massachusetts Supreme Judicial Court rules slavery illegal based on 1780 state constitution. All slaves are immediately freed. 1783: New Hampshire begins a gradual abolition of slavery. 1784: Connecticut begins a gradual abolition of slavery, freeing future children of slaves, and later all slaves 1784: Rhode Island begins a gradual abolition of slavery. 1787: The United States in Congress Assembled passed the Northwest Ordinance of 1787 outlawing any new slavery in the Northwest Territories. 1799: New York State passes gradual emancipation act freeing future children of slaves, and all slaves in 1827. 1802: Ohio writes a state constitution that abolishes slavery. 1804: New Jersey begins a gradual abolition of slavery, freeing future children of slaves. Those born prior to the Act remain enslaved for life. 1805: Great Britain: bill for Abolition passed in Commons, rejected in the House of Lords. 1806: U.S. President Thomas Jefferson in a message to Congress calls for criminalizing the international slave trade, asking Congress to "withdraw the citizens of the United States from all further participation in those violations of human rights … which the morality, the reputation, and the best of our country have long been eager to proscribe." 1807, 2 March: Jefferson signs the Act Prohibiting Importation of Slaves into law in the U.S. which took effect 1 January 1808. -

Behavioral Health Barometer: Vermont, Volume 6
Behavioral Health Barometer Vermont, Volume 6 Indicators as measured through the 2019 National Survey on Drug Use and Health and the National Survey of Substance Abuse Treatment Services VT VT VT Acknowledgments This report was prepared for the Substance Abuse and Mental Health Services Administration (SAMHSA) under contract No. 283–17–3101 with SAMHSA, U.S. Department of Health and Human Services (HHS). Public Domain Notice All material appearing in this report is in the public domain and may be reproduced or copied without permission from SAMHSA. Citation of the source is appreciated. However, this publication may not be reproduced or distributed for a fee without the specific, written authorization of the Office of Communications, SAMHSA, HHS. Electronic Access This publication may be downloaded at https://store.samhsa.gov. Recommended Citation Substance Abuse and Mental Health Services Administration. Behavioral Health Barometer: Vermont, Volume 6: Indicators as measured through the 2019 National Survey on Drug Use and Health and the National Survey of Substance Abuse Treatment Services. HHS Publication No. SMA–20–Baro–19–VT. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2020. Originating Office Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 5600 Fishers Lane, Rockville, MD 20857. Nondiscrimination Notice SAMHSA complies with applicable federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, -

Northern Railroad of New Hampshire -Concord to West Lebanon, NH = 69 Miles +/- • Ashuelot R
The Politics, Economics, and Technology of Early Railroad Development in Vermont and the Montpelier & Wells River Railroad The Plainfield Historical Society January 31, 2016 Frank J. Barrett, Jr. The Program Part I The Politics, Economics, and Technology of Early Railroad Development in Vermont 1825 to 1855 (BREAK) Part II The Montpelier & Wells River Railroad 1867 - 1956 Part I The Politics, Economics, and Technology of Early Railroad Development in Vermont 1825 to 1855 The Question: What Brought the Confluence of Railroads into the Upper Connecticut River Valley and Vermont in the late 1840’s? The Answer: The Erie Canal thru the Mohawk Valley of New York Opened in October 1825. Connected New York City with the Great Lakes and Canada. The Erie Canal Was a Political Success Cost to the State of New York: $7,143,789.66 Period of Construction: July 4, 1817 to October 26, 1825 (8 years, 3 months) For the first time in this country a government was engaged in the funding of a large scale transportation internal improvement project. The Erie Canal Was an Engineering Success 363 Miles Long 83 Locks 18 Aqueducts Approximately 300 Bridges Greatly advanced the knowledge of civil engineering and construction practices. The Erie Canal Was an Economic Success Cross State Travel Time: 4 to 6 Weeks Dropped to 6 Days Freight Transportation Costs: $95 to $125 ton Dropped to $4 to $6 ton Established great economic growth along the length of the canal and at New York City. The Geographical Problem: Mislocated Colonial Ports From the American Traveler of Boston in 1825 “Is Old Massachusetts in her palsied Dotage? Is her sun of prosperity … setting, to rise no more? This sun with increasing splendor is irradiating the hills of the Hudson and fertile vales of New York. -

STATE of NEW HAMPSHIRE Executive Council THEODORE L
STATE OF NEW HAMPSHIRE Executive Council THEODORE L. GATSAS State House Room 207 Executive Councilor 107 North Main Street District Four Concord, NH 03301 WWW.NH.GOV/COUNCIL (603) 271-3632 TO: All District Four Cities and Towns FROM: Executive Councilor Theodore L. Gatsas DATE: January 22, 2021 The Governor and Executive Council met on Friday, January 22, 2021, in Concord, NH and considered an agenda of approximately 143 items. The next scheduled Governor and Executive Council Meeting will be held on Wednesday, February 3, 2021 at 10:00 a.m. in Concord, NH. These meetings are available telephonically. CONSENT CALENDAR AGENDA #1 MOP 150, I, B (1): Expenditure Approvals DEPARTMENT OF TRANSPORTATION #A. Authorized the Bureau of Turnpikes to continue membership and participation with the E- ZPass Interagency Group, New York, NY, by paying annual membership dues in the amount of $75,000 for Calendar Year 2021. Effective upon G&C approval. 100% Turnpike Funds. VOTE: 5-0 DEPARTMENT OF EDUCATION #B. Authorized to enter Katelyn Komisarek into an educational tuition agreement with College for America, Southern NH University, Manchester, NH, to participate in Public Administration during the period of March 1, 2021 through June 20, 2021, and to pay said costs in the amount of $999. 100% Other Agency Income. VOTE: 5-0 #2 MOP 150, I, B (2): Approval of Acceptances DEPARTMENT OF ADMINISTRATIVE SERVICES #A. Authorized to accept direct reimbursement for professional development, technical assistance, and cooperative outreach from the National Association of State Procurement Officials for an amount not to exceed $70,400. Effective upon G&C approval through December 31, 2021. -

Vermont Forests 2017
United States Department of Agriculture Vermont Forests 2017 Forest Service Northern Resource Bulletin Publication Date Research Station NRS-120 March 2020 Abstract The second full remeasurement of the annual inventory of the forests of Vermont was completed in 2017 and covers nearly 4.5 million acres of forest land, with an average volume of over 2,300 cubic feet per acre. The data in this report are based on 1,125 plots located across Vermont. Forest land is dominated by the maple/beech/birch forest-type group, which occupies 71 percent of total forest land area. Of the forest land, 70 percent consists of large diameter trees, 23 percent contains medium diameter trees, and 7 percent contains small diameter trees. The volume of growing stock on timberland has continued to increase since the 1980s and currently totals nearly 9 billion cubic feet. The average annual net growth of growing stock on timberland from 2012 to 2017 was nearly 160 million cubic feet per year. Additional information is presented on forest attributes, land use change, carbon, timber products, species composition, regeneration, and forest health. Sets of supplemental tables are available online at https://doi.org/10.2737/NRS-RB-120 and contain summaries of quality assurance data and a core set of estimates for a variety of forest resources. Acknowledgments The authors would like to thank inventory crew members from Vermont for their help during the 2008–2017 inventory years: Aaron Clark, Robert Gregory, John Higham, Katherine Locke, Jason Morrison, Joyce Quinn, Bryan Tirrell, and Ashley Zickefoose. Thanks also to Paul Frederick and Barbara Schultz for serving as reviewers and providing insightful, constructive comments. -

COVID-19 Modeling December 8, 2020
COVID-19 Modeling December 8, 2020 Presentation available at: dfr.vermont.gov Covid on the rise in the Region Massachusetts coronavirus cases hit Rhode Island averaging the most daily cases per single-day record high for second straight day capita in the United States Boston Herald – Der 3, 202 WPRI 12 – December 7, 2020 New COVID infections soar in New Rhode Island reports 35 COVID deaths, Hampshire 3,681 new cases over last 3 days - a record 1,618 people tested positive on Thursday New Hampshire Public Radio – December 7, 2020 The Providence Journal – December 7, 2020 Maine shatters previous record with 427 new 1 in 10 of NY’s 700K coronavirus cases were cases of COVID-19 reported since Thanksgiving Day WMTW 8 – December 7, 2020 Syracuse.com – December 6, 2020 Connecticut Sees Highest COVID-19 Positivity Rate Statewide hospitalizations hit an all-time high Since Spring: Lamont of 144 Thursday WVIT – December 3, 2020 Portland Press Herald – December 4, 2020 2 Covid-19 Infections Past Three Weeks Nation 27% Region 10 Days 78% 7 Days Vermont 54% 3 Sources: Vermont Department of Health and Johns Hopkins University - November 16th to December 7th Covid-19 Positivity Rates Past Three Weeks Nation 5% 10 Days Region 7 Days 56% Vermont -6% 4 Sources: Vermont Department of Health and Johns Hopkins University - November 16th to December 7th 5 Sources: Vermont Department of Health Regional Case Growth 53.11% Increase in New Confirmed Cases Positive Cases Nov. 24th to Nov. 30th Positive Cases Dec. 1st to Dec. 7th 93,132 142,547142,598 6 Sources: State -

New Hampshire Commuting Patterns
New Hampshire Commuting Patterns Commuters who live Workers commuting and work in Residents commuting from another state: 65,486 New Hampshire: to another state: 106,338 571,241 Working in New Hampshire . Nearly all (94.6 percent) New Hampshire residents who commute out‐of‐state travel to . An average of 636,727 workers commute to a work in one of the three bordering states. job in New Hampshire. Among those New Hampshire residents who . About nine out of ten workers (89.7 percent) leave the state for work, 78.6 percent travel to who work in New Hampshire also live here Massachusetts, 8.5 percent travel to work in (571,241). Another 10.3 percent of workers Vermont, and 7.5 percent travel to work in commute in from another state (65,486). Maine. Nearly all (95.0 percent) of New Hampshire . Just over 300 residents reported working in a workers who live in another state commute in country other than the United States. from one of the three bordering states. Among those who commute to New Hampshire from another state for work, 26.7 percent come New Hampshire InState Commuters from Maine, 45.7 percent come from . There are 571,241 New Hampshire residents Massachusetts, and 22.5 percent come from age 16 and over who also work in the state. Vermont. About two‐thirds of these New Hampshire residents work in three counties: 31.2 percent Residents of New Hampshire work in Hillsborough County, 20.9 percent work in Rockingham County, and 13.1 percent . An average of 677,579 New Hampshire work in Merrimack County. -

A Love Letter to Vermont
Christ Church Opens Why Are They Birding Abounds in Warming Shelter / p.5 Returning Home? / p.14 Adamant / p.24 Holiday Shopping & F r e e , ThanksgivingIndependent Nov 18–Decand 16, Local 2020 Thanksgiving Torch Passes A Love Letter to National to Vermont Life, Sodexo By Mike Dunphy he coronavirus is notching yet an- other change to Central Vermont TThanksgivings this year. After 47 years, the Washington County Youth Service Bureau/Boys & Girls Clubs have passed the torch of its annual Thanksgiv- ing dinner to National Life and Sodexo. No longer able to throw the in-person feast at Bethany Church in Montpelier because of the pandemic, the new part- ners are offering a pick-up this year and will continue to offer delivery. In part, the change is a result of the dinner’s immense success over the years — serving 814 in 2019 (from less than 100 in its first year), alone — as it has stretched the abilities of the organization to handle the major solicitation and coor- dination effort required to make the meal happen. But it’s the pandemic that broke the camel’s back, as it stripped non-profit organizations around the country, the Youth Services Bureau included, of mon- etary donations, volunteers, fundraising opportunities, and more. “The pandemic made it all but impossible for staff to take on the event this year from a time, logis- The author on a snowy hike. see Thanksgiving, page 12 Courtesy photo. By Mirna Valerio he other day I spent an afternoon on the Stowe Pin- This is what I think of when I think of Vermont — nacle trail, marveling at all that trail and others here shared responsibility; collective wonderment; a sense of ECRWSS PRSRT STD Montpelier, VT Montpelier, Permit NO. -

Executive Order 01-20
STATE OF VERMONT EXECUTIVE DEPARTMENT ADDENDUM 8 TO AMENDED AND RESTATED EXECUTIVE ORDER 01-20 [Extension of State of Emergency Declared March 13, 2020; Stay Safe/Stay Working/Stay in School] WHEREAS, since December 2019, Vermont has been working in close collaboration with the National Centers for Disease Control and Prevention (“CDC”) and with the United States Health and Human Services Agency to first monitor and plan for outbreaks of a respiratory illness due to a novel coronavirus (“COVID-19”) and then to implement measures to keep Vermonters healthy and safe; and WHEREAS, the Governor directed the Vermont Department of Health (“VDH”) to activate the Health Operations Center in February 2020 when VDH began to monitor and later, test Vermonters who may have been exposed to COVID-19; and WHEREAS, in March 2020, the Governor directed the Department of Public Safety, Division of Vermont Emergency Management (“DPS”) to assemble an interagency taskforce, and later to activate the Vermont State Emergency Operations Center (“SEOC”), in accordance with the State Emergency Management Plan, to organize prevention, response and mitigation efforts and share information with local and State officials; and WHEREAS, on March 7, 2020 and March 11, 2020, VDH detected the first two cases of COVID-19 in Vermont and as of November 13, 2020, the State has experienced 2,651 cases and 59 deaths which are COVID-19 related; and WHEREAS, on March 11, 2020 the World Health Organization made the assessment that COVID-19 can be characterized as a pandemic; and -

Master Plan Montpelier, Vermont
“October Crossing,” Robin LaHue MASTER PLAN MONTPELIER, VERMONT Montpelier Planning Commission enVision Montpelier Stakeholders Department of Planning and Community Development Final Adopted Version: September 23, 2015 Expires: December 1, 2017 (per condition of approval) 2 Alexandria Heather, Montpelier resident Table of Contents Introduction ..................................................................................................... 13 Master Plan Process ..................................................................................................................... 13 National Citizens Survey ............................................................................................................. 17 Survey Findings ............................................................................................................................ 17 Consistency with Act 200 ............................................................................................................. 18 Background ............................................................................................................................. 22 Development History ................................................................................................................... 22 State and Regional Context ......................................................................................................... 25 Montpelier’s Magic ..................................................................................................................... -

Covid-19 Daily Update
COVID-19 Update July 1, 2021 New or updated information is in red and bold Also available online at healthvermont.gov/covid19 Click the “Vermont COVID-19 Update” button This will be the COVID-19 Update’s final issue After nearly 16 months, today will be the final issue of this COVID-19 Update. It has been a valuable tool to share information with the media, state and national partners throughout this response. We will continue to keep everyone informed through our regular communication channels, including news releases, social media @healthvermont and our website, healthvermont.gov. You can continue to access daily cases and other data, updated regularly, on the COVID-19 Vaccine Dashboard and the COVID-19 activity on the Vermont Dashboard. Thank you for staying informed throughout the COVID-19 response! Free, convenient, walk-in clinics available through the Fourth of July weekend New walk-in clinics available across Vermont throughout the holiday weekend, including at the Johnson Skate Park, Barton Fairground, Stowe Independence Day celebration, and more. “Even with our state’s high vaccination rate, we still need as many Vermonters as possible to protect themselves from COVID-19 by getting vaccinated,” Gov. Phil Scott said, in a press release. “If you’re not yet vaccinated, I encourage you to join the vast majority of your fellow Vermonters and find a clinic near you. Every Vermonter vaccinated puts us in a better position to continue to build on the progress we’ve made into the fall and winter. It’s free, quick and easy, and there is no better time than now.” You can find a list of walk-in clinics for this weekend and more at healthvermont.gov/MyVaccine.