2016 Annual Impact Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Interview with Larry Pope by Andrea L’Hommedieu
Bowdoin College Bowdoin Digital Commons George J. Mitchell Oral History Project Special Collections and Archives 5-14-2008 Interview with Larry Pope by Andrea L’Hommedieu Laurence 'Larry' E. Pope Follow this and additional works at: https://digitalcommons.bowdoin.edu/mitchelloralhistory Part of the Law and Politics Commons, Oral History Commons, Political History Commons, and the United States History Commons Recommended Citation Pope, Laurence 'Larry' E., "Interview with Larry Pope by Andrea L’Hommedieu" (2008). George J. Mitchell Oral History Project. 46. https://digitalcommons.bowdoin.edu/mitchelloralhistory/46 This Interview is brought to you for free and open access by the Special Collections and Archives at Bowdoin Digital Commons. It has been accepted for inclusion in George J. Mitchell Oral History Project by an authorized administrator of Bowdoin Digital Commons. For more information, please contact [email protected]. George J. Mitchell Oral History Project Special Collections & Archives, Bowdoin College Library, 3000 College Sta., Brunswick, Maine 04011 © Bowdoin College Laurence E. Pope GMOH# 013 (Interviewer: Andrea L’Hommedieu) May 15, 2008 Andrea L’Hommedieu: This is an interview for George J. Mitchell Oral History Project. The date is May 15, 2008. I’m here at the Hawthorne-Longfellow Library at Bowdoin College with Laurence “Larry” Pope. This is Andrea L’Hommedieu. Could you start, Mr. Pope, just by giving me your full name? Laurence Pope: Yes, my name is Laurence Pope, and Laurence Everett Pope is the middle initial. AL: And where and when were you born? LP: I was born in New Haven, Connecticut, on September 24, 1945. AL: Is that the area in which you grew up? LP: No, my father was studying Japanese at Yale University at the time, and so that’s why we were there. -
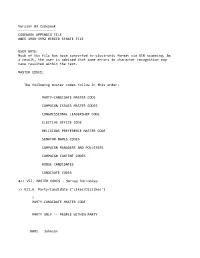
Appendix File Anes 1988‐1992 Merged Senate File
Version 03 Codebook ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ CODEBOOK APPENDIX FILE ANES 1988‐1992 MERGED SENATE FILE USER NOTE: Much of his file has been converted to electronic format via OCR scanning. As a result, the user is advised that some errors in character recognition may have resulted within the text. MASTER CODES: The following master codes follow in this order: PARTY‐CANDIDATE MASTER CODE CAMPAIGN ISSUES MASTER CODES CONGRESSIONAL LEADERSHIP CODE ELECTIVE OFFICE CODE RELIGIOUS PREFERENCE MASTER CODE SENATOR NAMES CODES CAMPAIGN MANAGERS AND POLLSTERS CAMPAIGN CONTENT CODES HOUSE CANDIDATES CANDIDATE CODES >> VII. MASTER CODES ‐ Survey Variables >> VII.A. Party/Candidate ('Likes/Dislikes') ? PARTY‐CANDIDATE MASTER CODE PARTY ONLY ‐‐ PEOPLE WITHIN PARTY 0001 Johnson 0002 Kennedy, John; JFK 0003 Kennedy, Robert; RFK 0004 Kennedy, Edward; "Ted" 0005 Kennedy, NA which 0006 Truman 0007 Roosevelt; "FDR" 0008 McGovern 0009 Carter 0010 Mondale 0011 McCarthy, Eugene 0012 Humphrey 0013 Muskie 0014 Dukakis, Michael 0015 Wallace 0016 Jackson, Jesse 0017 Clinton, Bill 0031 Eisenhower; Ike 0032 Nixon 0034 Rockefeller 0035 Reagan 0036 Ford 0037 Bush 0038 Connally 0039 Kissinger 0040 McCarthy, Joseph 0041 Buchanan, Pat 0051 Other national party figures (Senators, Congressman, etc.) 0052 Local party figures (city, state, etc.) 0053 Good/Young/Experienced leaders; like whole ticket 0054 Bad/Old/Inexperienced leaders; dislike whole ticket 0055 Reference to vice‐presidential candidate ? Make 0097 Other people within party reasons Card PARTY ONLY ‐‐ PARTY CHARACTERISTICS 0101 Traditional Democratic voter: always been a Democrat; just a Democrat; never been a Republican; just couldn't vote Republican 0102 Traditional Republican voter: always been a Republican; just a Republican; never been a Democrat; just couldn't vote Democratic 0111 Positive, personal, affective terms applied to party‐‐good/nice people; patriotic; etc. -
Marblehead Boaters Slip Into Winter
TUESDAY, OCTOBER 11, 2016 Peabody gins up case for 20 more liquor licenses By Adam Swift areas in surrounding communities like Thursday night. If the committee ap- If the latest home rule petition gets ap- ITEM CITY EDITOR Salem, Beverly and Danvers, and unless proves the request, it will be forwarded to proved, Gravel said he hopes it is with there are liquor licenses, we won’t get the the Committee of the Whole for approval. more leeway than the 2014 license in- PEABODY — A home rule petition caliber of restaurants that will be able to At that point, Bettencourt would be able crease. led with the state legislature to allow survive.” to le a home rule petition with the state “On Main Street and Walnut Street, as many as 20 new liquor licenses in the In August, Mayor Edward A. Betten- legislature. there are a lot of buildings with poten- city could help open up downtown devel- court Jr. submitted a request to the In 2014, similar legislation added 10 li- tial for restaurants if they had a liquor opment, said a city councilor. council for approval of a home rule pe- quor licenses, bringing the city’s total to license,” he said. “I’m supportive of any move that will tition to increase the number of all-al- 11 beer and wine licenses and 70 all-alco- Gravel said there are already examples give us the ability to lock up restaurants cohol liquor licenses in Peabody by no hol licenses. But the 2014 legislation did on Main Street of how liquor licenses and other businesses that are looking at more than 20. -

Justices' Profiles Institute of Bill of Rights Law at the William & Mary Law School
College of William & Mary Law School William & Mary Law School Scholarship Repository Supreme Court Preview Conferences, Events, and Lectures 1995 Section 1: Justices' Profiles Institute of Bill of Rights Law at the William & Mary Law School Repository Citation Institute of Bill of Rights Law at the William & Mary Law School, "Section 1: Justices' Profiles" (1995). Supreme Court Preview. 35. https://scholarship.law.wm.edu/preview/35 Copyright c 1995 by the authors. This article is brought to you by the William & Mary Law School Scholarship Repository. https://scholarship.law.wm.edu/preview WARREN E. BURGER IS DEAD AT 87 Was Chief Justice for 17 Years Copyright 1995 The New York Times Company The New York Times June 26, 1995, Monday Linda Greenhouse Washington, June 25 - Warren E. Burger, who retired to apply like an epithet -- overruled no major in 1986 after 17 years as the 15th Chief Justice of the decisions from the Warren era. United States, died here today at age 87. The cause It was a further incongruity that despite Chief was congestive heart failure, a spokeswoman for the Justice Burger's high visibility and the evident relish Supreme Court said. with which he used his office to expound his views on An energetic court administrator, Chief Justice everything from legal education to prison Burger was in some respects a transitional figure management, scholars and Supreme Court despite his tenure, the longest for a Chief Justice in commentators continued to question the degree to this century. He presided over a Court that, while it which he actually led the institution over which he so grew steadily more conservative with subsequent energetically presided. -

Annual Report
COUNCIL ON FOREIGN RELATIONS ANNUAL REPORT July 1,1996-June 30,1997 Main Office Washington Office The Harold Pratt House 1779 Massachusetts Avenue, N.W. 58 East 68th Street, New York, NY 10021 Washington, DC 20036 Tel. (212) 434-9400; Fax (212) 861-1789 Tel. (202) 518-3400; Fax (202) 986-2984 Website www. foreignrela tions. org e-mail publicaffairs@email. cfr. org OFFICERS AND DIRECTORS, 1997-98 Officers Directors Charlayne Hunter-Gault Peter G. Peterson Term Expiring 1998 Frank Savage* Chairman of the Board Peggy Dulany Laura D'Andrea Tyson Maurice R. Greenberg Robert F Erburu Leslie H. Gelb Vice Chairman Karen Elliott House ex officio Leslie H. Gelb Joshua Lederberg President Vincent A. Mai Honorary Officers Michael P Peters Garrick Utley and Directors Emeriti Senior Vice President Term Expiring 1999 Douglas Dillon and Chief Operating Officer Carla A. Hills Caryl R Haskins Alton Frye Robert D. Hormats Grayson Kirk Senior Vice President William J. McDonough Charles McC. Mathias, Jr. Paula J. Dobriansky Theodore C. Sorensen James A. Perkins Vice President, Washington Program George Soros David Rockefeller Gary C. Hufbauer Paul A. Volcker Honorary Chairman Vice President, Director of Studies Robert A. Scalapino Term Expiring 2000 David Kellogg Cyrus R. Vance Jessica R Einhorn Vice President, Communications Glenn E. Watts and Corporate Affairs Louis V Gerstner, Jr. Abraham F. Lowenthal Hanna Holborn Gray Vice President and Maurice R. Greenberg Deputy National Director George J. Mitchell Janice L. Murray Warren B. Rudman Vice President and Treasurer Term Expiring 2001 Karen M. Sughrue Lee Cullum Vice President, Programs Mario L. Baeza and Media Projects Thomas R. -

2013 Annual Report M Ission
2013 ANNUAL REPORT M ISSION The New England Council is an alliance of businesses, academic and health institutions, and public and private organizations throughout New England formed to promote economic growth and a high quality of life in the New England region. The New England Council is a leading voice on the issues that shape the region’s economy and quality of life. The Council focuses on key industries that drive the region’s economic growth including education, energy, transportation, technology and innovation, healthcare and financial services. THE NEW ENGLAND COUNCIL TABLE OF CONTENTS 2013 4 President’s Letter 5 Chairman’s Letter ADVOCACY & INITIATIVES 6 Overview 7 Advanced Manufacturing 8 Defense 9 Energy & Environment 11 Financial Services 12 Healthcare 14 Higher Education 16 New England Economic Partnership 17 Technology 19 Transportation Committee EVENTS 20 Annual Spring Event 22 Annual Dinner 24 Congressional Roundtable Series 26 Capital Conversations Series 28 Featured Events 30 Politics & Eggs Series ABOUT THE COUNCIL 31 DC Dialogue 32 Board of Directors 35 Members 3 THE NEW ENGLAND COUNCIL 2013 PRESIDENT’S LETTER DeaR NEW ENGland Council MEMBER: As I look back at 2013, I am once again impressed by what a successful and productive year it has been for The New England Council. That success has come on several fronts, from membership growth, to new programming and events, to effective advocacy for issues and policies that impact our region. I’m pleased to report that 2013 was an incredibly busy year for the Council with over 50 events and programs for our members over the course of the year. -

Fall Elections Are Less Than 3 Months Away One of the Many Impacts Of
Fall Elections are Less Than 3 Months Away One of the many impacts of the COVID-19 pandemic is that some events that are non-pandemic-related get lost in the all-COVID, all-the-time news coverage. In the midst of the recent NH House and Senate meetings in-person at different locations than their usual State House chambers, the filing period for all State elective offices quietly opened and closed. Other than one US Senator whose term does not end this year - Sen. Maggie Hassan (D) - every NH state, county and local elective office is up for grabs and there are some surprises in the NH House, Senate and Executive Council line-ups for the September primary and the November general elections. In the House, 38 Democrats and 37 Republicans did not file for re-election, which will leave some big holes, especially in committee leadership positions. The chair of the Commerce & Consumer Affairs Committee, Ed Butler, is stepping down and the Science and Technology Committee is losing both its chair and vice-chair, Bob Backus and Howard Moffett. The Health, Human Services and Elderly Affairs Committee will lose its vice-chair, Polly Campion. And the Children and Family Law and Criminal Justice and Public Safety Committees will both lose their vice-chairs, Skip Berrien and Beth Rodd. In addition, two Division chairs of the House Finance Committee will not be back next session because they are seeking higher office: Patricia Lovejoy (D) is running for the Executive Council seat left open by the retirement of Russell Prescott; and Susan Ford (D) is running for State Senate District One, the seat now held by David Starr (R). -

2015 Annual Report Swanzey, New Hampshire
2015 Annual Report Swanzey, New Hampshire The Four Seasons of Swanzey County, State & Federal Government Resources Contact and Meeting Information Governor Maggie Hassan Cheshire County - Commissioners Office of the Governor County Administrative Offices www.town.swanzey.nh.us State House 33 West Street Town Hall Contact Information Regular Monthly Meetings 107 North Main Street Keene, NH 03431 All meetings are held at Town Hall, unless Concord, NH 03301 352-8215 District 1 (Swanzey): 620 Old Homestead Highway otherwise posted. 207-2121 Peter Graves, Clerk PO Box 10009 Swanzey, New Hampshire 03446-0009 Consult the town calendar at New Hampshire General Court District 2: www.town.swanzey.nh.us for the most Chuck Weed, Vice Chair (603)352-7411 up-to-date meeting information. Senator Molly Kelly PO Box 267 District 3: NH Relay TDD 1(800)735-2964 Board of Selectmen Harrisville, NH 03450 cell: Stillman Rogers, Chair (603)352-6250 (Fax) Tuesday Evenings, 6 p.m. 603-491-2502 [email protected] x101 Town Clerk Deborah J. Davis: 352-4435 (home) NH Congressional Delegation x105 Code Enforcement Offi cer W. William Hutwelker III: 313-3948 (cell) Representative Jim McConnell U.S. Senators x107 Town Administrator Kenneth P. Colby Jr.: 357-3499 (home) PO Box G Senator Kelly Ayotte x108 Town Planner [email protected] Keene, NH 03431 41 Hooksett Road, Unit 2 x109 Tax Collector 357-7150 x110 General Assistance Coordinator Planning Board Manchester, NH 03104 2nd & 4th Thursday, 6 p.m. [email protected] x111 Finance Offi ce 622-7979 http://ayotte.senate.gov/ x114 Assessing Coordinator Zoning Board of Adjustment Representative Benjamin Tilton 3rd Monday (Except Jan & Feb), 7 p.m. -

The Senate in Transition Or How I Learned to Stop Worrying and Love the Nuclear Option1
\\jciprod01\productn\N\NYL\19-4\NYL402.txt unknown Seq: 1 3-JAN-17 6:55 THE SENATE IN TRANSITION OR HOW I LEARNED TO STOP WORRYING AND LOVE THE NUCLEAR OPTION1 William G. Dauster* The right of United States Senators to debate without limit—and thus to filibuster—has characterized much of the Senate’s history. The Reid Pre- cedent, Majority Leader Harry Reid’s November 21, 2013, change to a sim- ple majority to confirm nominations—sometimes called the “nuclear option”—dramatically altered that right. This article considers the Senate’s right to debate, Senators’ increasing abuse of the filibuster, how Senator Reid executed his change, and possible expansions of the Reid Precedent. INTRODUCTION .............................................. 632 R I. THE NATURE OF THE SENATE ........................ 633 R II. THE FOUNDERS’ SENATE ............................. 637 R III. THE CLOTURE RULE ................................. 639 R IV. FILIBUSTER ABUSE .................................. 641 R V. THE REID PRECEDENT ............................... 645 R VI. CHANGING PROCEDURE THROUGH PRECEDENT ......... 649 R VII. THE CONSTITUTIONAL OPTION ........................ 656 R VIII. POSSIBLE REACTIONS TO THE REID PRECEDENT ........ 658 R A. Republican Reaction ............................ 659 R B. Legislation ...................................... 661 R C. Supreme Court Nominations ..................... 670 R D. Discharging Committees of Nominations ......... 672 R E. Overruling Home-State Senators ................. 674 R F. Overruling the Minority Leader .................. 677 R G. Time To Debate ................................ 680 R CONCLUSION................................................ 680 R * Former Deputy Chief of Staff for Policy for U.S. Senate Democratic Leader Harry Reid. The author has worked on U.S. Senate and White House staffs since 1986, including as Staff Director or Deputy Staff Director for the Committees on the Budget, Labor and Human Resources, and Finance. -

Kelly Ayotte Occupation: U.S
Name: Kelly Ayotte Occupation: U.S. Senator, New Hampshire As a former New Hampshire Attorney General and now U.S. Senator, you’ve had the opportunity to see our crumbling justice system from multiple perspectives. How do Republicans keep the “tough on crime” mantra while addressing critical funding issues and high recidivism rates? For starters, with over $17 trillion in debt, we need to get our fiscal house in order. Spending on wasteful or duplicative programs diverts money from more urgent priorities. I’ve worked at the federal level to address a problem that we are seeing all across the country – the fact that our nation’s jails are becoming de facto mental health facilities. Having worked as a prosecutor and as state attorney general, I know that there are gaps in both our existing mental health and judicial systems – which is why I’m co-sponsoring the Justice and Mental Health Collaboration Act. This bipartisan legislation would help ensure law enforcement has the tools they need to identify and respond to mental health issues. It would also continue support for mental health courts and crisis intervention teams – getting defendants the treatment they need and stemming recidivism. Some credit you as replacing Sen. Lieberman within the “Three Amigos” as the newcomer to this prominent gathering of Senate foreign policy titans. What have you learned from your short time working with Senators McCain and Graham? No one can replace Joe Lieberman! He was one of my designated mentors when I arrived in the Senate, and I benefitted tremendously from his guidance. -

Table of Contents
Table of Contents 2014 Warrant & Budget Elected Town Officials/Appointed Town Boards and Committees 1 Report of the Board of Selectmen 2 2015 Town Meeting Warrant 4 2015 Recommended Town Budget, Appropriations & Estimated Revenues Summary 7 2015 Default Budget 9 Town Government Economic Development Administration 10 Economic Development Advisory Committee 25 Police Department 11 Swanzey Revenue Development District 26 Emergency Management Department 12 Culture, Conservation & Recreation Fire Department 13 Ashuelot River Local Advisory Committee 27 Public Works Department 16 Swanzey Conservation Commission 29 Recycling Center 17 Open Space Committee 30 Planning Board 18 Recreation Committee 31 Planning & Community Development 19 West Swanzey Sidewalk Committee 31 Zoning Board of Adjustment 20 Swanzey Historical Museum 32 Sewer Commission 21 Old Home Day Committee 33 Trustees of Trust Funds 22 Mount Caesar Union Library 34 Carpenter Home 23 Stratton Free Library 35 North Swanzey Water & Fire Precinct 24 Whitcomb Hall Committee 36 2013 Financial Reports Treasurer’s Report 37 Summary of Tax Collector Activity 40 Financial Report of the Town Clerk 42 General Fund Detailed Statement of Receipts 43 Detailed Statement of Payments, All Funds 44 Carpenter Home Special Revenue Fund Report of Operational Costs and Related Rev- 50 enue Trustees of Trust Funds Financial Reports for Town & Monadnock Regional School District 51 Summary of Assessed Valuation 56 Tax Rate Information (2014 & Previous Years) 57 Police Special Details Revolving Fund 58 Recycling -

Women's Representation in New Hampshire
Women’s Representation in New Hampshire Parity Ranking: 1st of 50 Levels of Government Score of 47: Fifteen points for Gov. Maggie Statewide Executives Hassan’s first term, 12 for first terms of Senators Jeanne Shaheen (D) and Kelly Ayotte Female governors: Vesta Roy (1982-83, (R), 7 for the percent of recent House elections appointed), Jeanne Shaheen (1997-2003), won by women, 10 for the percentage of state Maggie Hassan (2013-present) legislators who are women, 1 for speaker of the house, and 2 for Mayor Donnalee Lozeau of The position of governor is New Hampshire’s Nashua. only statewide elected executive office. Quick Facts Congress New Hampshire is the first and only state to U.S. Senate: 2 of 2 seats are held by women, send an all-female delegation to Congress. New Kelly Ayotte (2011-present), Jeanne Shaheen (2009-present) Hampshire also was the first state in the nation to have a majority female state legislative U.S. House: 2 of 2 seats are held by women chamber (in the state Senate in 2009-2010). In its history, New Hampshire has elected four Trending women to Congress, all of whom are currently in office. New Hampshire experienced a drop in the State Legislature percentage of legislative seats held by women after the 2010 election, when Republicans took Percentage women: 33.5% control of both the state House and Senate. The th number of women dropped from 13 to 6 in the Rankings: 5 of 50 Senate and 143 to 99 in the House. In 2012, Senate: 9 of 24 (37.5%) are women women made a substantial rebound; there are now 140 women serving in the state legislature.