Knockdown of KDM1B Inhibits Cell Proliferation and Induces Apoptosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![Crystal Structure of LSD1 in Complex with 4-[5-(Piperidin-4-Ylmethoxy)-2-(P-Tolyl) Pyridin-3-Yl]Benzonitrile](https://docslib.b-cdn.net/cover/7859/crystal-structure-of-lsd1-in-complex-with-4-5-piperidin-4-ylmethoxy-2-p-tolyl-pyridin-3-yl-benzonitrile-127859.webp)
Crystal Structure of LSD1 in Complex with 4-[5-(Piperidin-4-Ylmethoxy)-2-(P-Tolyl) Pyridin-3-Yl]Benzonitrile
molecules Article Crystal Structure of LSD1 in Complex with 4-[5-(Piperidin-4-ylmethoxy)-2-(p-tolyl) pyridin-3-yl]benzonitrile Hideaki Niwa 1 ID , Shin Sato 1, Tomoko Hashimoto 2, Kenji Matsuno 2 and Takashi Umehara 1,* ID 1 Laboratory for Epigenetics Drug Discovery, RIKEN Center for Biosystems Dynamics Research (BDR), 1-7-22 Suehiro-cho, Tsurumi, Yokohama 230-0045, Japan; [email protected] (H.N.); [email protected] (S.S.) 2 Department of Chemistry and Life Science, School of Advanced Engineering, Kogakuin University, 2665-1 Nakano, Hachioji, Tokyo 192-0015, Japan; [email protected] (T.H.); [email protected] (K.M.) * Correspondence: [email protected]; Tel.: +81-45-503-9457 Received: 28 May 2018; Accepted: 22 June 2018; Published: 26 June 2018 Abstract: Because lysine-specific demethylase 1 (LSD1) regulates the maintenance of cancer stem cell properties, small-molecule inhibitors of LSD1 are expected to be useful for the treatment of several cancers. Reversible inhibitors of LSD1 with submicromolar inhibitory potency have recently been reported, but their exact binding modes are poorly understood. In this study, we synthesized a recently reported reversible inhibitor, 4-[5-(piperidin-4-ylmethoxy)-2-(p-tolyl)pyridin-3- yl]benzonitrile, which bears a 4-piperidinylmethoxy group, a 4-methylphenyl group, and a 4-cyanophenyl group on a pyridine ring, and determined the crystal structure of LSD1 in complex with this inhibitor at 2.96 Å. We observed strong electron density for the compound, showing that its cyano group forms a hydrogen bond with Lys661, which is a critical residue in the lysine demethylation reaction located deep in the catalytic center of LSD1. -

82594016.Pdf
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Structure Article Molecular Mimicry and Ligand Recognition in Binding and Catalysis by the Histone Demethylase LSD1-CoREST Complex Riccardo Baron,1,* Claudia Binda,2 Marcello Tortorici,2 J. Andrew McCammon,1 and Andrea Mattevi2,* 1Department of Chemistry and Biochemistry, Center for Theoretical Biological Physics, and Department of Pharmacology, Howard Hughes Medical Institute, University of California at San Diego, La Jolla, CA 92093-0365, USA 2Department of Genetics and Microbiology, University of Pavia, Via Ferrata 1, 27100, Pavia, Italy *Correspondence: [email protected] (R.B.), [email protected] (A.M.) DOI 10.1016/j.str.2011.01.001 SUMMARY (LSD1 or KDM1A, according to the newly adopted nomencla- ture) (Shi et al., 2004; Forneris et al., 2005). This enzyme acts Histone demethylases LSD1 and LSD2 (KDM1A/B) on mono- and dimethylated Lys4 of histone H3 through a catalyze the oxidative demethylation of Lys4 of FAD-dependent oxidative process (Figure 1A). LSD1 is often histone H3. We used molecular dynamics simula- associated to the histone deacetylases (HDAC) 1 and 2 and to tions to probe the diffusion of the oxygen substrate. the corepressor protein CoREST, which tightly binds to LSD1 Oxygen can reach the catalytic center independently enhancing both its stability and enzymatic activity. A number of from the presence of a bound histone peptide, studies have indicated that LSD1-CoREST interacts with various protein complexes involved in gene regulation and chromatin implying that LSD1 can complete subsequent deme- modification (Forneris et al., 2008; Mosammaparast and Shi, thylation cycles without detaching from the nucleo- 2010). -
Partial Deletion of Chromosome 6P Causing Developmental Delay and Mild Dysmorphisms in a Child
Vrachnis et al. Mol Cytogenet (2021) 14:39 https://doi.org/10.1186/s13039-021-00557-y CASE REPORT Open Access Partial deletion of chromosome 6p causing developmental delay and mild dysmorphisms in a child: molecular and developmental investigation and literature search Nikolaos Vrachnis1,2,3* , Ioannis Papoulidis4, Dionysios Vrachnis5, Elisavet Siomou4, Nikolaos Antonakopoulos1,2, Stavroula Oikonomou6, Dimitrios Zygouris2, Nikolaos Loukas7, Zoi Iliodromiti8, Efterpi Pavlidou9, Loretta Thomaidis6 and Emmanouil Manolakos4 Abstract Background: The interstitial 6p22.3 deletions concern rare chromosomal events afecting numerous aspects of both physical and mental development. The syndrome is characterized by partial deletion of chromosome 6, which may arise in a number of ways. Case presentation: We report a 2.8-year old boy presenting with developmental delay and mild dysmorphisms. High-resolution oligonucleotide microarray analysis revealed with high precision a 2.5 Mb interstitial 6p deletion in the 6p22.3 region which encompasses 13 genes. Conclusions: Identifcation and in-depth analysis of cases presenting with mild features of the syndrome will sharpen our understanding of the genetic spectrum of the 6p22.3 deletion. Keywords: 6p22.3 deletion, Syndrome, Developmental delay, Intellectual disability, Dysmorphism, Behavioral abnormalities, High-resolution microarray analysis Background dysmorphic features, and structural organ defects, as well Te interstitial deletion of chromosomal region 6p22.3 as intellectual disability. is a rare condition with variable phenotypic expression. We report herein a case of interstitial deletion of chro- To date, more than 30 children and adolescents with this mosome 6p investigated by array-CGH in a 2.8-year old deletion have been reported [1–11]. -

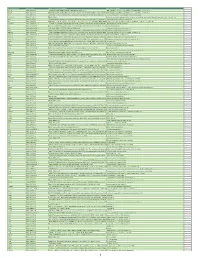
Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -
Official Symbol Accession Alias / Previous Symbol Official Full Name
Official Symbol Accession Alias / Previous Symbol Official Full Name Abcc3 NM_029600.3 1700019L09Rik,MRP3,RIKEN cDNA 1700019L09 gene ATP-binding cassette, sub-family C (CFTR/MRP), member 3 Abcc8 NM_011510.3 D930031B21Rik,MGD-MRK-33673,MGI:105993,MGI:3036285,RIKEN cDNA D930031B21ATP-binding gene,sulfonylurea cassette, sub-familyreceptor,Sur,SUR1 C (CFTR/MRP), member 8 Abl1 NM_009594.4 AI325092,c-Abl,E430008G22Rik,expressed sequence AI325092,MGD-MRK-1015,MGI:2138905,MGI:2443781,RIKENc-abl oncogene 1, non-receptor cDNAtyrosine E430008G22 kinase gene Adamts16 NM_172053.2 MGC:37086 a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 16 Ago4 NM_153177.3 5730550L01Rik,AI481660,argonaute 4,Eif2c4,eukaryotic translation initiation factorargonaute 2C, 4,expressed RISC catalytic sequence subunit AI481660,MGI:2140312,RIKEN 4 cDNA 5730550L01 gene Agt NM_007428.3 AI265500,angiotensin precursor,Aogen,expressed sequence AI265500,MGD-MRK-1192,MGI:2142488,Serpina8angiotensinogen (serpin peptidase inhibitor, clade A, member 8) AI464131 NM_001085515.2 AA408153,AI604836,expressed sequence AA408153,expressed sequence expressedexpressed sequence sequence AI604836,gene AI464131 model 762, (NCBI),Gm762,MGI:2140126,MGI:2140342,MGI:2685608,NET37 Ak1 NM_001198790.1 Ak-1,B430205N08Rik,MGD-MRK-1240,MGD-MRK-1244,MGI:2445070,RIKEN cDNA B430205N08adenylate kinase gene 1 Akt1 NM_001165894.1 Akt,MGD-MRK-1257,PKB,PKB/Akt,PKBalpha thymoma viral proto-oncogene 1 Akt2 NM_001110208.1 2410016A19Rik,AW554154,expressed sequence AW554154,MGD-MRK-28173,MGI:1923730,MGI:2142261,PKB,PKBbeta,RIKENthymoma -

Supplementary Materials
Supplementary materials Supplementary Table S1: MGNC compound library Ingredien Molecule Caco- Mol ID MW AlogP OB (%) BBB DL FASA- HL t Name Name 2 shengdi MOL012254 campesterol 400.8 7.63 37.58 1.34 0.98 0.7 0.21 20.2 shengdi MOL000519 coniferin 314.4 3.16 31.11 0.42 -0.2 0.3 0.27 74.6 beta- shengdi MOL000359 414.8 8.08 36.91 1.32 0.99 0.8 0.23 20.2 sitosterol pachymic shengdi MOL000289 528.9 6.54 33.63 0.1 -0.6 0.8 0 9.27 acid Poricoic acid shengdi MOL000291 484.7 5.64 30.52 -0.08 -0.9 0.8 0 8.67 B Chrysanthem shengdi MOL004492 585 8.24 38.72 0.51 -1 0.6 0.3 17.5 axanthin 20- shengdi MOL011455 Hexadecano 418.6 1.91 32.7 -0.24 -0.4 0.7 0.29 104 ylingenol huanglian MOL001454 berberine 336.4 3.45 36.86 1.24 0.57 0.8 0.19 6.57 huanglian MOL013352 Obacunone 454.6 2.68 43.29 0.01 -0.4 0.8 0.31 -13 huanglian MOL002894 berberrubine 322.4 3.2 35.74 1.07 0.17 0.7 0.24 6.46 huanglian MOL002897 epiberberine 336.4 3.45 43.09 1.17 0.4 0.8 0.19 6.1 huanglian MOL002903 (R)-Canadine 339.4 3.4 55.37 1.04 0.57 0.8 0.2 6.41 huanglian MOL002904 Berlambine 351.4 2.49 36.68 0.97 0.17 0.8 0.28 7.33 Corchorosid huanglian MOL002907 404.6 1.34 105 -0.91 -1.3 0.8 0.29 6.68 e A_qt Magnogrand huanglian MOL000622 266.4 1.18 63.71 0.02 -0.2 0.2 0.3 3.17 iolide huanglian MOL000762 Palmidin A 510.5 4.52 35.36 -0.38 -1.5 0.7 0.39 33.2 huanglian MOL000785 palmatine 352.4 3.65 64.6 1.33 0.37 0.7 0.13 2.25 huanglian MOL000098 quercetin 302.3 1.5 46.43 0.05 -0.8 0.3 0.38 14.4 huanglian MOL001458 coptisine 320.3 3.25 30.67 1.21 0.32 0.9 0.26 9.33 huanglian MOL002668 Worenine -

KDM1B Protein Full Length Mouse Recombinant Protein Expressed in Sf9 Cells
Catalog # Aliquot Size K421-30BG-20 20 µg K421-30BG-50 50 µg KDM1B Protein Full length mouse recombinant protein expressed in Sf9 cells Catalog # K421-30BG Lot # P1749-3 Product Description Purity Recombinant full-length mouse KDM1B was expressed by baculovirus in Sf9 insect cells using an N-terminal GST tag. The gene accession number is NM_172262. The purity of KDM1B was Gene Aliases determined to be >85% by densitometry. 4632428N09Rik; AI482520; Aof1 Approx. MW ~118kDa. Formulation Recombinant protein stored in 50mM Tris-HCl, pH 7.5, 150mM NaCl, 10mM glutathione, 0.1mM EDTA, 0.25mM DTT, 0.1mM PMSF, 25% glycerol. Storage and Stability Store product at –70oC. For optimal storage, aliquot target into smaller quantities after centrifugation and store at recommended temperature. For most favorable performance, avoid repeated handling and multiple freeze/thaw cycles. Scientific Background KDM1B encodes Lysine-specific histone demethylase 1B that demethylates 'Lys-4' of histone H3, a specific tag for epigenetic transcriptional activation, thereby acting as a corepressor. It specifically associates with the coding region of its target genes. Removal of endogenous KDM1B Protein KDM1B promotes an increase in H3K4me2 levels and Full length mouse recombinant protein expressed in Sf9 cells concurrent decrease in H3K9me2 levels, with a consequent down-regulation of targeted gene Catalog Number K421-30BG transcription. Lot # P1749-3 Purity >85% References Concentration 0.1 µg/µl Stability 1yr at –70oC from date of shipment o 1. Fang R, et al. Human LSD2/KDM1b/AOF1regulates gene Storage & Shipping Store product at –70 C. For optimal storage, aliquot target into smaller transcription by modulating intragenic H3K4me2 methyla- quantities after centrifugation and tion. -

Long Non-Coding RNA Landscape in Prostate Cancer Molecular Subtypes: a Feature Selection Approach
International Journal of Molecular Sciences Article Long Non-Coding RNA Landscape in Prostate Cancer Molecular Subtypes: A Feature Selection Approach Simona De Summa 1,* , Antonio Palazzo 2 , Mariapia Caputo 1, Rosa Maria Iacobazzi 3 , Brunella Pilato 1, Letizia Porcelli 3, Stefania Tommasi 1 , Angelo Virgilio Paradiso 4,† and Amalia Azzariti 3,† 1 Molecular Diagnostics and Pharmacogenetics Unit, IRCCS IstitutoTumori Giovanni Paolo II, 70124 Bari, Italy; [email protected] (M.C.); [email protected] (B.P.); [email protected] (S.T.) 2 Laboratory of Nanotechnology, IRCCS IstitutoTumori Giovanni Paolo II, 70124 Bari, Italy; [email protected] 3 Laboratory of Experimental Pharmacology, IRCCS Istituto Tumori Giovanni Paolo II, 70124 Bari, Italy; [email protected] (R.M.I.); [email protected] (L.P.); [email protected] (A.A.) 4 Scientific Directorate, IRCCS Istituto Tumori Giovanni Paolo II, 70124 Bari, Italy; [email protected] * Correspondence: [email protected] † Co-senior authors. Abstract: Prostate cancer is one of the most common malignancies in men. It is characterized by a high molecular genomic heterogeneity and, thus, molecular subtypes, that, to date, have not been used in clinical practice. In the present paper, we aimed to better stratify prostate cancer patients through the selection of robust long non-coding RNAs. To fulfill the purpose of the study, a bioinformatic approach focused on feature selection applied to a TCGA dataset was used. In such a way, LINC00668 and long non-coding(lnc)-SAYSD1-1, able to discriminate ERG/not-ERG subtypes, Citation: De Summa, S.; Palazzo, A.; were demonstrated to be positive prognostic biomarkers in ERG-positive patients. -

The BAP1 Deubiquitinase Complex Is a General Transcriptional Co-Activator
bioRxiv preprint doi: https://doi.org/10.1101/244152; this version posted January 8, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. The BAP1 deubiquitinase complex is a general transcriptional co-activator Antoine Campagne1,2, Dina Zielinski1,2 ,3, Audrey Michaud1,2, Stéphanie Le Corre1,2, Florent Dingli1, Hong Chen1,2, Ivaylo Vassilev1,2 ,3, Ming-Kang Lee1,2, Nicolas Servant1,3, Damarys Loew1, Eric Pasmant4, Sophie Postel-Vinay5, Michel Wassef1,2* and Raphaël Margueron1,2* 1 Institut Curie, Paris Sciences et Lettres Research University, 75005 Paris, France. 2 INSERM U934/ CNRS UMR3215. 3 INSERM U900, Mines ParisTech. 4 EA7331, Faculty of Pharmacy, University of Paris Paris Descartes, Department of Molecular Genetics Pathology, Cochin Hospital, HUPC AP-HP, Paris, France. 5 Gustave Roussy, Département d'Innovation Thérapeutique et Essais Précoces, INSERM U981, Université Paris-Saclay, Villejuif, F-94805, France. *Corresponding Authors: Institut Curie - 26 rue d'Ulm, 75005 Paris Emails: [email protected] or [email protected] Tel: +33 (0)156246551 Fax: +33 (0)156246939 bioRxiv preprint doi: https://doi.org/10.1101/244152; this version posted January 8, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. ABSTRACT In Drosophila, a complex consisting of Calypso and ASX catalyzes H2A deubiquitination and has been reported to act as part of the Polycomb machinery in transcriptional silencing. The mammalian homologs of these proteins (BAP1 and ASXL1/2/3, respectively), are frequently mutated in various cancer types, yet their precise functions remain unclear. -

Emerging Multifaceted Roles of BAP1 Complexes in Biological Processes Aileen Patricia Szczepanski1 and Lu Wang1
Szczepanski and Wang Cell Death Discovery (2021) 7:20 https://doi.org/10.1038/s41420-021-00406-2 Cell Death Discovery REVIEW ARTICLE Open Access Emerging multifaceted roles of BAP1 complexes in biological processes Aileen Patricia Szczepanski1 and Lu Wang1 Abstract Histone H2AK119 mono-ubiquitination (H2AK119Ub) is a relatively abundant histone modification, mainly catalyzed by the Polycomb Repressive Complex 1 (PRC1) to regulate Polycomb-mediated transcriptional repression of downstream target genes. Consequently, H2AK119Ub can also be dynamically reversed by the BAP1 complex, an evolutionarily conserved multiprotein complex that functions as a general transcriptional activator. In previous studies, it has been reported that the BAP1 complex consists of important biological roles in development, metabolism, and cancer. However, identifying the BAP1 complex’s regulatory mechanisms remains to be elucidated due to its various complex forms and its ability to target non-histone substrates. In this review, we will summarize recent findings that have contributed to the diverse functional role of the BAP1 complex and further discuss the potential in targeting BAP1 for therapeutic use. Facts levels for catalytic activity and accurate cellular localization, which are critical for the determinant of ● cell fate and transformation. The BAP1 complex has 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; The BAP1 complex is an evolutionary conserved, emerged as an ideal therapeutic target for treatments multiprotein complex that functions -

Exome Sequencing of 457 Autism Families Recruited Online Provides Evidence for Autism Risk Genes
www.nature.com/npjgenmed ARTICLE OPEN Exome sequencing of 457 autism families recruited online provides evidence for autism risk genes Pamela Feliciano1, Xueya Zhou 2, Irina Astrovskaya 1, Tychele N. Turner 3, Tianyun Wang3, Leo Brueggeman4, Rebecca Barnard5, Alexander Hsieh 2, LeeAnne Green Snyder1, Donna M. Muzny6, Aniko Sabo6, The SPARK Consortium, Richard A. Gibbs6, Evan E. Eichler 3,7, Brian J. O’Roak 5, Jacob J. Michaelson 4, Natalia Volfovsky1, Yufeng Shen 2 and Wendy K. Chung1,8 Autism spectrum disorder (ASD) is a genetically heterogeneous condition, caused by a combination of rare de novo and inherited variants as well as common variants in at least several hundred genes. However, significantly larger sample sizes are needed to identify the complete set of genetic risk factors. We conducted a pilot study for SPARK (SPARKForAutism.org) of 457 families with ASD, all consented online. Whole exome sequencing (WES) and genotyping data were generated for each family using DNA from saliva. We identified variants in genes and loci that are clinically recognized causes or significant contributors to ASD in 10.4% of families without previous genetic findings. In addition, we identified variants that are possibly associated with ASD in an additional 3.4% of families. A meta-analysis using the TADA framework at a false discovery rate (FDR) of 0.1 provides statistical support for 26 ASD risk genes. While most of these genes are already known ASD risk genes, BRSK2 has the strongest statistical support and reaches genome-wide significance as a risk gene for ASD (p-value = 2.3e−06). -

Germline Mutations in Histone 3 Family 3A and 3B Cause a Previously Unidentified Neurodegenerative Disorder in 46 Patients
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2020 Histone H3.3 beyond cancer: Germline mutations in Histone 3 Family 3A and 3B cause a previously unidentified neurodegenerative disorder in 46 patients Laura Bryant Marcia C Willing Linda Manwaring et al Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs SCIENCE ADVANCES | RESEARCH ARTICLE GENETICS Copyright © 2020 The Authors, some rights reserved; Histone H3.3 beyond cancer: Germline mutations in exclusive licensee American Association Histone 3 Family 3A and 3B cause a previously for the Advancement of Science. No claim to unidentified neurodegenerative disorder in 46 patients original U.S. Government Laura Bryant1*, Dong Li1*, Samuel G. Cox2, Dylan Marchione3, Evan F. Joiner4, Khadija Wilson3, Works. Distributed 3 5 1 1 6 6 under a Creative Kevin Janssen , Pearl Lee , Michael E. March , Divya Nair , Elliott Sherr , Brieana Fregeau , Commons Attribution 7 7 8 9 Klaas J. Wierenga , Alexandrea Wadley , Grazia M. S. Mancini , Nina Powell-Hamilton , NonCommercial 10 11 12 12 13 Jiddeke van de Kamp , Theresa Grebe , John Dean , Alison Ross , Heather P. Crawford , License 4.0 (CC BY-NC). Zoe Powis14, Megan T. Cho15, Marcia C. Willing16, Linda Manwaring16, Rachel Schot8, Caroline Nava17,18, Alexandra Afenjar19, Davor Lessel20,21, Matias Wagner22,23,24, Thomas Klopstock25,26,27, Juliane Winkelmann22,24,27,28, Claudia B. Catarino25, Kyle Retterer15, Jane L. Schuette29, Jeffrey W. Innis29, Amy Pizzino30,31, Sabine Lüttgen32, Jonas Denecke32, 22,24 15 3 30,31 Tim M. Strom , Kristin G. Monaghan ; DDD Study, Zuo-Fei Yuan , Holly Dubbs , Downloaded from Renee Bend33, Jennifer A.