Anaplasmosis.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anaplasma Species of Veterinary Importance in Japan
Veterinary World, EISSN: 2231-0916 REVIEW ARTICLE Available at www.veterinaryworld.org/Vol.9/November-2016/4.pdf Open Access Anaplasma species of veterinary importance in Japan Adrian Patalinghug Ybañez1 and Hisashi Inokuma2 1. Biology and Environmental Studies Program, Sciences Cluster, University of the Philippines Cebu, Lahug, Cebu City 6000, Philippines; 2. Department of Veterinary Clinical Science, Obihiro University of Agriculture and Veterinary Medicine, Obihiro, Inada Cho, Hokkaido 080-8555, Japan. Corresponding author: Adrian Patalinghug Ybañez, e-mail: [email protected], HI: [email protected] Received: 14-06-2016, Accepted: 28-09-2016, Published online: 04-11-2016 doi: 10.14202/vetworld.2016.1190-1196 How to cite this article: Ybañez AP, Inokuma H (2016) Anaplasma species of veterinary importance in Japan, Veterinary World, 9(11): 1190-1196. Abstract Anaplasma species of the family Anaplasmataceae, order Rickettsiales are tick-borne organisms that can cause disease in animals and humans. In Japan, all recognized species of Anaplasma (except for Anaplasma ovis) and a potentially novel Anaplasma sp. closely related to Anaplasma phagocytophilum have been reported. Most of these detected tick- borne pathogens are believed to be lowly pathogenic in animals in Japan although the zoonotic A. phagocytophilum has recently been reported to cause clinical signs in a dog and in humans. This review documents the studies and reports about Anaplasma spp. in Japan. Keywords: Anaplasma spp., Japan, tick-borne pathogen. Introduction A. phagocytophilum sequences [10-15]. Phylogenetic Anaplasma species are Gram-negative, obligate inferences have suggested that 2 clades exist within intracellular bacteria of the order Rickettsiales, fam- the genus Anaplasma: (1) Erythrocytic (A. -

Melioidosis in Birds and Burkholderia Pseudomallei Dispersal, Australia
LETTERS 5. Mätz-Rensing K, Jentsch KD, Rensing S, Melioidosis in Birds However, these are mostly birds Langenhuynsen S, Verschoor E, Niphuis in captivity and often exotic to the H, et al. Fatal herpes simplex infection in and Burkholderia a group of common marmosets (Callithrix location, suggesting potential reduced jacchus). Vet Pathol. 2003;40:405–11. pseudomallei immunity. Little is known about doi:10.1354/vp.40-4-405 Dispersal, Australia melioidosis in wild birds. In Sabah, 6. Bruno SF, Liebhold M, Mätz-Rensing K, Malaysia, only 1 of 440 wild birds Romão MA, Didier A, Brandes A, et al. Herpesvirus infection in free-living black- To the Editor: Melioidosis is an admitted to a research center over 9 tufted-ear marmoset (Callithrix penicil- emerging infectious disease of humans years was found to have melioidosis lata E. Geoffroyi 1812) at the state park of and animals caused by the gram- (6). Serra da Tiririca, Niterói, Rio de Janeiro, negative bacterium Burkholderia Although birds are endotherms, Brazil. Berl Munch Tierarztl Wochenschr. 1997;110:427–30. pseudomallei, which inhabits soil and with high metabolic rates and body 7. Kalter SS, Heberling RL. Comparative surface water in the disease-endemic temperature (40°C–43°C) protecting virology of primates. Bacteriol Rev. regions of Southeast Asia and northern them from many diseases, some birds 1971;35:310–64. Australia (1). The aim of this study appear more susceptible to melioidosis. 8. Mansfi eld K. Emerging and re-emerging infectious diseases of nonhuman primates. was to assess the potential for birds Indeed, high body temperature would Proceedings of the American College to spread B. -

Anaplasmosis: an Emerging Tick-Borne Disease of Importance in Canada
IDCases 14 (2018) xxx–xxx Contents lists available at ScienceDirect IDCases journal homepage: www.elsevier.com/locate/idcr Case report Anaplasmosis: An emerging tick-borne disease of importance in Canada a, b,c d,e e,f Kelsey Uminski *, Kamran Kadkhoda , Brett L. Houston , Alison Lopez , g,h i c c Lauren J. MacKenzie , Robbin Lindsay , Andrew Walkty , John Embil , d,e Ryan Zarychanski a Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, University of Manitoba, Winnipeg, MB, Canada b Cadham Provincial Laboratory, Government of Manitoba, Winnipeg, MB, Canada c Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Medical Microbiology and Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada d Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Medical Oncology and Hematology, University of Manitoba, Winnipeg, MB, Canada e CancerCare Manitoba, Department of Medical Oncology and Hematology, Winnipeg, MB, Canada f Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Pediatrics and Child Health, Section of Infectious Diseases, Winnipeg, MB, Canada g Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada h Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Community Health Sciences, University of Manitoba, Winnipeg, MB, Canada i Public Health Agency of Canada, National Microbiology Laboratory, Zoonotic Diseases and Special Pathogens, Winnipeg, MB, Canada A R T I C L E I N F O A B S T R A C T Article history: Human Granulocytic Anaplasmosis (HGA) is an infection caused by the intracellular bacterium Received 11 September 2018 Anaplasma phagocytophilum. -

Ehrlichiosis and Anaplasmosis Are Tick-Borne Diseases Caused by Obligate Anaplasmosis: Intracellular Bacteria in the Genera Ehrlichia and Anaplasma
Ehrlichiosis and Importance Ehrlichiosis and anaplasmosis are tick-borne diseases caused by obligate Anaplasmosis: intracellular bacteria in the genera Ehrlichia and Anaplasma. These organisms are widespread in nature; the reservoir hosts include numerous wild animals, as well as Zoonotic Species some domesticated species. For many years, Ehrlichia and Anaplasma species have been known to cause illness in pets and livestock. The consequences of exposure vary Canine Monocytic Ehrlichiosis, from asymptomatic infections to severe, potentially fatal illness. Some organisms Canine Hemorrhagic Fever, have also been recognized as human pathogens since the 1980s and 1990s. Tropical Canine Pancytopenia, Etiology Tracker Dog Disease, Ehrlichiosis and anaplasmosis are caused by members of the genera Ehrlichia Canine Tick Typhus, and Anaplasma, respectively. Both genera contain small, pleomorphic, Gram negative, Nairobi Bleeding Disorder, obligate intracellular organisms, and belong to the family Anaplasmataceae, order Canine Granulocytic Ehrlichiosis, Rickettsiales. They are classified as α-proteobacteria. A number of Ehrlichia and Canine Granulocytic Anaplasmosis, Anaplasma species affect animals. A limited number of these organisms have also Equine Granulocytic Ehrlichiosis, been identified in people. Equine Granulocytic Anaplasmosis, Recent changes in taxonomy can make the nomenclature of the Anaplasmataceae Tick-borne Fever, and their diseases somewhat confusing. At one time, ehrlichiosis was a group of Pasture Fever, diseases caused by organisms that mostly replicated in membrane-bound cytoplasmic Human Monocytic Ehrlichiosis, vacuoles of leukocytes, and belonged to the genus Ehrlichia, tribe Ehrlichieae and Human Granulocytic Anaplasmosis, family Rickettsiaceae. The names of the diseases were often based on the host Human Granulocytic Ehrlichiosis, species, together with type of leukocyte most often infected. -

Anaplasmosis
Anaplasmosis Definition: Anaplasmosis is an infection caused by the bacterium Anaplasma phagocytophilum. It is most commonly transmitted by the bite of an infected deer tick (Ixodes scapularis). Signs and symptoms: Symptoms of anaplasmosis can range from mild to very severe and may include: fever, headache, muscle pain, malaise, chills, nausea, abdominal pain, cough, and confusion. Severe symptoms may include: difficulty breathing, hemorrhage, renal failure, or neurological problems. It can be fatal if not treated correctly. People who are immunocompromised or elderly are at higher risk for severe disease. Transmission: Anaplasmosis is primarily transmitted to a person through the bite of an infected deer tick; this tick is endemic throughout Maine. Rarely, it can also be transmitted by receiving blood transfusions from an infected donor. Diagnosis: Anaplasmosis is diagnosed by clinical symptoms and laboratory tests. A blood test is necessary for confirmation. Co-infections with other tick-borne diseases may occur and should be considered. Role of the School Nurse: Prevention • Provide education on prevention efforts including: wearing protective clothing, using an EPA- approved repellent, using caution in tick infested areas, and performing daily tick checks. • Encourage the use of EPA approved repellents when outside (following local policy guidelines), and always performing a tick check when returning indoors. o School nurses can apply repellent with parental permission • If a tick is found, the school nurse should remove the tick using tweezers or a tick spoon. o Tick identification cards are available at: http://www.maine.gov/dhhs/mecdc/infectious- disease/epi/vector-borne/posters/index.shtml. o Testing of the tick is not recommended. -

Human Granulocytic Anaplasmosis (HGA)
MASSACHUSETTS DEPARTMENT OF PUBLIC HEALTH FACT SHEET Human Granulocytic Anaplasmosis (HGA) April 2014 | Page 1 of 3 What is human granulocytic anaplasmosis (HGA)? HGA is caused by bacteria (germs) that attack certain types of white blood cells called granulocytes. HGA is also known as human granulocytic ehrlichiosis. Where do cases of HGA occur? In the United States, HGA is most commonly found in the Northeast, mid-Atlantic and upper Midwest. In Massachusetts, the highest rates of disease occur on the islands of Nantucket and Martha’s Vineyard and in Barnstable and Berkshire counties, but it can occur anywhere in the state. How is HGA spread? HGA is one of the diseases that can be spread by the bite of an infected deer tick. The longer a tick remains attached and feeding, the higher the likelihood that it may spread the bacteria. Deer ticks in Massachusetts can also carry the germs that cause Lyme disease and babesiosis. Deer ticks are capable of spreading more than one type of germ in a single bite. When can I get HGA? HGA can occur during any time of year. The bacteria that cause HGA are spread by infected deer ticks. Young ticks (nymphs) are most active during the warm weather months between May and July. Adult ticks are most active during the fall and spring but will also be out searching for a host any time that winter temperatures are above freezing. How soon do symptoms of HGA appear after a tick bite? Symptoms of HGA usually begin to appear 7 to 14 days after being bitten by an infected tick. -

Reportable Disease Surveillance in Virginia, 2013
Reportable Disease Surveillance in Virginia, 2013 Marissa J. Levine, MD, MPH State Health Commissioner Report Production Team: Division of Surveillance and Investigation, Division of Disease Prevention, Division of Environmental Epidemiology, and Division of Immunization Virginia Department of Health Post Office Box 2448 Richmond, Virginia 23218 www.vdh.virginia.gov ACKNOWLEDGEMENT In addition to the employees of the work units listed below, the Office of Epidemiology would like to acknowledge the contributions of all those engaged in disease surveillance and control activities across the state throughout the year. We appreciate the commitment to public health of all epidemiology staff in local and district health departments and the Regional and Central Offices, as well as the conscientious work of nurses, environmental health specialists, infection preventionists, physicians, laboratory staff, and administrators. These persons report or manage disease surveillance data on an ongoing basis and diligently strive to control morbidity in Virginia. This report would not be possible without the efforts of all those who collect and follow up on morbidity reports. Divisions in the Virginia Department of Health Office of Epidemiology Disease Prevention Telephone: 804-864-7964 Environmental Epidemiology Telephone: 804-864-8182 Immunization Telephone: 804-864-8055 Surveillance and Investigation Telephone: 804-864-8141 TABLE OF CONTENTS INTRODUCTION Introduction ......................................................................................................................................1 -

Leptospirosis Associated Equine Recurrent Uveitis Answers to Your Important Questions What Is Leptospirosis Associated Equine Recurrent Uveitis (LAERU)?
Lisa Dauten, DVM Tri-State Veterinary Services LLC " Leptospirosis Associated Equine Recurrent Uveitis Answers to your Important Questions! What is Leptospirosis Associated Equine Recurrent Uveitis (LAERU)? Let’s start by breaking down some terminology.! Uveitis- inflammation of the uvea. Resulting in cloudiness of the eye, pain, and potential blindness. Also know as “Moon Blindness”. Caused by trauma, infection, or corneal disease.! Uvea- part of the eye containing the iris, ciliary body, and choroid. It keeps the lens of the eye in place, maintains fluid in the eye, and keeps things in the blood from entering the inside of the eye (blood-ocular barrier). ! Recurrent Uveitis- inflammation of the uvea that sporadically reoccurs through out a horses life time. Each time there is a reoccurring episode, the damage to the eye is made worse, eventually leading to permanent damage and potential blindness. ! Leptospirosis- bacteria found in the environment shed in the urine of wildlife and livestock. Horses usually are exposed when grazing pastures or drinking from natural water sources.! LAERU- Recurrent Uveitis in horses caused by Leptospirosis.! What are the clinical signs of Uveitis? Uveitis can come on very suddenly. A lot of times horses present with severe pain in the eye, tearing, squinting, and rubbing face. The eye itself is cloudy, white or blue in color. Sometimes the signs are not as dramatic. The color change of the eye may progress slowly. In these cases, horse owners may mistake the changes for cataracts.! What do I do if I think my horse has Uveitis? Call your veterinarian to request an appointment. -

Tick-Borne Diseases in Maine a Physician’S Reference Manual Deer Tick Dog Tick Lonestar Tick (CDC Photo)
tick-borne diseases in Maine A Physician’s Reference Manual Deer Tick Dog Tick Lonestar Tick (CDC PHOTO) Nymph Nymph Nymph Adult Male Adult Male Adult Male Adult Female Adult Female Adult Female images not to scale know your ticks Ticks are generally found in brushy or wooded areas, near the DEER TICK DOG TICK LONESTAR TICK Ixodes scapularis Dermacentor variabilis Amblyomma americanum ground; they cannot jump or fly. Ticks are attracted to a variety (also called blacklegged tick) (also called wood tick) of host factors including body heat and carbon dioxide. They will Diseases Diseases Diseases transfer to a potential host when one brushes directly against Lyme disease, Rocky Mountain spotted Ehrlichiosis anaplasmosis, babesiosis fever and tularemia them and then seek a site for attachment. What bites What bites What bites Nymph and adult females Nymph and adult females Adult females When When When April through September in Anytime temperatures are April through August New England, year-round in above freezing, greatest Southern U.S. Coloring risk is spring through fall Adult females have a dark Coloring Coloring brown body with whitish Adult females have a brown Adult females have a markings on its hood body with a white spot on reddish-brown tear shaped the hood Size: body with dark brown hood Unfed Adults: Size: Size: Watermelon seed Nymphs: Poppy seed Nymphs: Poppy seed Unfed Adults: Sesame seed Unfed Adults: Sesame seed suMMer fever algorithM ALGORITHM FOR DIFFERENTIATING TICK-BORNE DISEASES IN MAINE Patient resides, works, or recreates in an area likely to have ticks and is exhibiting fever, This algorithm is intended for use as a general guide when pursuing a diagnosis. -

Detection of Tick-Borne Pathogens of the Genera Rickettsia, Anaplasma and Francisella in Ixodes Ricinus Ticks in Pomerania (Poland)
pathogens Article Detection of Tick-Borne Pathogens of the Genera Rickettsia, Anaplasma and Francisella in Ixodes ricinus Ticks in Pomerania (Poland) Lucyna Kirczuk 1 , Mariusz Piotrowski 2 and Anna Rymaszewska 2,* 1 Department of Hydrobiology, Faculty of Biology, Institute of Biology, University of Szczecin, Felczaka 3c Street, 71-412 Szczecin, Poland; [email protected] 2 Department of Genetics and Genomics, Faculty of Biology, Institute of Biology, University of Szczecin, Felczaka 3c Street, 71-412 Szczecin, Poland; [email protected] * Correspondence: [email protected] Abstract: Tick-borne pathogens are an important medical and veterinary issue worldwide. Environ- mental monitoring in relation to not only climate change but also globalization is currently essential. The present study aimed to detect tick-borne pathogens of the genera Anaplasma, Rickettsia and Francisella in Ixodes ricinus ticks collected from the natural environment, i.e., recreational areas and pastures used for livestock grazing. A total of 1619 specimens of I. ricinus were collected, including ticks of all life stages (adults, nymphs and larvae). The study was performed using the PCR technique. Diagnostic gene fragments msp2 for Anaplasma, gltA for Rickettsia and tul4 for Francisella were ampli- fied. No Francisella spp. DNA was detected in I. ricinus. DNA of A. phagocytophilum was detected in 0.54% of ticks and Rickettsia spp. in 3.69%. Nucleotide sequence analysis revealed that only one species of Rickettsia, R. helvetica, was present in the studied tick population. The present results are a Citation: Kirczuk, L.; Piotrowski, M.; part of a large-scale analysis aimed at monitoring the level of tick infestation in Northwest Poland. -

Tick-Borne Disease Working Group 2020 Report to Congress
2nd Report Supported by the U.S. Department of Health and Human Services • Office of the Assistant Secretary for Health Tick-Borne Disease Working Group 2020 Report to Congress Information and opinions in this report do not necessarily reflect the opinions of each member of the Working Group, the U.S. Department of Health and Human Services, or any other component of the Federal government. Table of Contents Executive Summary . .1 Chapter 4: Clinical Manifestations, Appendices . 114 Diagnosis, and Diagnostics . 28 Chapter 1: Background . 4 Appendix A. Tick-Borne Disease Congressional Action ................. 8 Chapter 5: Causes, Pathogenesis, Working Group .....................114 and Pathophysiology . 44 The Tick-Borne Disease Working Group . 8 Appendix B. Tick-Borne Disease Working Chapter 6: Treatment . 51 Group Subcommittees ...............117 Second Report: Focus and Structure . 8 Chapter 7: Clinician and Public Appendix C. Acronyms and Abbreviations 126 Chapter 2: Methods of the Education, Patient Access Working Group . .10 to Care . 59 Appendix D. 21st Century Cures Act ...128 Topic Development Briefs ............ 10 Chapter 8: Epidemiology and Appendix E. Working Group Charter. .131 Surveillance . 84 Subcommittees ..................... 10 Chapter 9: Federal Inventory . 93 Appendix F. Federal Inventory Survey . 136 Federal Inventory ....................11 Chapter 10: Public Input . 98 Appendix G. References .............149 Minority Responses ................. 13 Chapter 11: Looking Forward . .103 Chapter 3: Tick Biology, Conclusion . 112 Ecology, and Control . .14 Contributions U.S. Department of Health and Human Services James J. Berger, MS, MT(ASCP), SBB B. Kaye Hayes, MPA Working Group Members David Hughes Walker, MD (Co-Chair) Adalbeto Pérez de León, DVM, MS, PhD Leigh Ann Soltysiak, MS (Co-Chair) Kevin R. -
Cattle Combination with Decoquinate
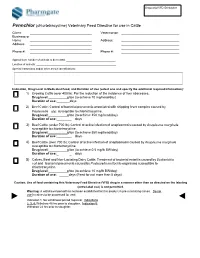
Sequential VFD ID Number Pennchlor (chlortetracycline) Veterinary Feed Directive for use in Cattle Client: __________________________________ Veterinarian: ________________________________ Business or Home __________________________________ Address: ________________________________ Address: __________________________________ ________________________________ __________________________________ ________________________________ Phone #: __________________________________ Phone #: ________________________________ Approximate number of animals to be treated: __________________________________ Location of animals: _______________________________________________________ Special Instructions and/or other animal identifications: Indication, Drug Level in Medicated Feed, and Duration of Use (select one and specify the additional required information): 1) Growing Cattle (over 400 lb): For the reduction of the incidence of liver abscesses. Drug level: g/ton (to achieve 70 mg/head/day) Duration of use:_ days 2) Beef Cattle: Control of bacterial pneumonia associated with shipping fever complex caused by Pasteurella spp. susceptible to chlortetracycline. Drug level: g/ton (to achieve 350 mg/head/day) Duration of use:_ _ days 3) Beef Cattle (under 700 lb): Control of active infection of anaplasmosis caused by Anaplasma marginale susceptible to chlortetracycline. Drug level: g/ton (to achieve 350 mg/head/day) Duration of use:_ _ days 4) Beef Cattle (over 700 lb): Control of active infection of anaplasmosis caused by Anaplasma marginale susceptible to chlortetracycline.