Differential Effects of PD-L1 Versus PD-1 Blockade on Myeloid Inflammation in Human Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soluble CD83 Inhibits T Cell Activation by Binding to the TLR4/MD-2 Complex on CD14+ Monocytes
Soluble CD83 Inhibits T Cell Activation by Binding to the TLR4/MD-2 Complex on CD14+ Monocytes This information is current as Joe M. Horvatinovich, Elizabeth W. Grogan, Marcus Norris, of September 29, 2021. Alexander Steinkasserer, Henrique Lemos, Andrew L. Mellor, Irina Y. Tcherepanova, Charles A. Nicolette and Mark A. DeBenedette J Immunol 2017; 198:2286-2301; Prepublished online 13 February 2017; Downloaded from doi: 10.4049/jimmunol.1600802 http://www.jimmunol.org/content/198/6/2286 Supplementary http://www.jimmunol.org/content/suppl/2017/02/11/jimmunol.160080 http://www.jimmunol.org/ Material 2.DCSupplemental References This article cites 80 articles, 29 of which you can access for free at: http://www.jimmunol.org/content/198/6/2286.full#ref-list-1 Why The JI? Submit online. by guest on September 29, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Author Choice Freely available online through The Journal of Immunology Author Choice option Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2017 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. -

Cx3cr1 Mediates the Development of Monocyte-Derived Dendritic Cells During Hepatic Inflammation
CX3CR1 MEDIATES THE DEVELOPMENT OF MONOCYTE-DERIVED DENDRITIC CELLS DURING HEPATIC INFLAMMATION. Supplementary material Supplementary Figure 1: Liver CD45+ myeloid cells were pre-gated for Ly6G negative cells for excluding granulocytes and HDCs subsequently analyzed among the cells that were CD11c+ and had high expression of MHCII. Supplementary Table 1 low/- high + Changes in gene expression between CX3CR1 and CX3CR1 CD11b myeloid hepatic dendritic cells (HDCs) from CCl4-treated mice high Genes up-regulated in CX3CR1 HDCs Gene Fold changes P value Full name App 4,01702 5,89E-05 amyloid beta (A4) precursor protein C1qa 9,75881 1,69E-22 complement component 1, q subcomponent, alpha polypeptide C1qb 9,19882 3,62E-20 complement component 1, q subcomponent, beta polypeptide Ccl12 2,51899 0,011769 chemokine (C-C motif) ligand 12 Ccl2 6,53486 6,37E-11 chemokine (C-C motif) ligand 2 Ccl3 4,99649 5,84E-07 chemokine (C-C motif) ligand 3 Ccl4 4,42552 9,62E-06 chemokine (C-C motif) ligand 4 Ccl6 3,9311 8,46E-05 chemokine (C-C motif) ligand 6 Ccl7 2,60184 0,009272 chemokine (C-C motif) ligand 7 Ccl9 4,17294 3,01E-05 chemokine (C-C motif) ligand 9 Ccr2 3,35195 0,000802 chemokine (C-C motif) receptor 2 Ccr5 3,23358 0,001222 chemokine (C-C motif) receptor 5 Cd14 6,13325 8,61E-10 CD14 antigen Cd36 2,94367 0,003243 CD36 antigen Cd44 4,89958 9,60E-07 CD44 antigen Cd81 6,49623 8,24E-11 CD81 antigen Cd9 3,06253 0,002195 CD9 antigen Cdkn1a 4,65279 3,27E-06 cyclin-dependent kinase inhibitor 1A (P21) Cebpb 6,6083 3,89E-11 CCAAT/enhancer binding protein (C/EBP), -

(Siglec) Adhesion Receptor That Binds CD83
CD83 Is a Sialic Acid-Binding Ig-Like Lectin (Siglec) Adhesion Receptor that Binds Monocytes and a Subset of Activated CD8+ T Cells This information is current as of September 25, 2021. Nathalie Scholler, Martha Hayden-Ledbetter, Karl-Erik Hellström, Ingegerd Hellström and Jeffrey A. Ledbetter J Immunol 2001; 166:3865-3872; ; doi: 10.4049/jimmunol.166.6.3865 http://www.jimmunol.org/content/166/6/3865 Downloaded from References This article cites 44 articles, 21 of which you can access for free at: http://www.jimmunol.org/content/166/6/3865.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 25, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts Errata An erratum has been published regarding this article. Please see next page or: /content/182/3/1772.2.full.pdf The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2001 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. CD83 Is a Sialic Acid-Binding Ig-Like Lectin (Siglec) Adhesion Receptor that Binds Monocytes and a Subset of Activated CD8؉ T Cells1 Nathalie Scholler,2* Martha Hayden-Ledbetter,† Karl-Erik Hellstro¨m,* Ingegerd Hellstro¨m,* and Jeffrey A. -

Expansions of Adaptive-Like NK Cells with a Tissue-Resident Phenotype in Human Lung and Blood
Expansions of adaptive-like NK cells with a tissue-resident phenotype in human lung and blood Demi Brownliea,1, Marlena Scharenberga,1, Jeff E. Moldb, Joanna Hårdb, Eliisa Kekäläinenc,d,e, Marcus Buggerta, Son Nguyenf,g, Jennifer N. Wilsona, Mamdoh Al-Amerih, Hans-Gustaf Ljunggrena, Nicole Marquardta,2,3, and Jakob Michaëlssona,2 aCenter for Infectious Medicine, Department of Medicine Huddinge, Karolinska Institutet, 14152 Stockholm, Sweden; bDepartment of Cell and Molecular Biology, Karolinska Institutet, 171 77 Stockholm, Sweden; cTranslational Immunology Research Program, University of Helsinki, 00014 Helsinki, Finland; dDepartment of Bacteriology and Immunology, University of Helsinki, 00014 Helsinki, Finland; eHelsinki University Central Hospital Laboratory, Division of Clinical Microbiology, Helsinki University Hospital, 00290 Helsinki, Finland; fDepartment of Microbiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104; gInstitute for Immunology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104; and hThoracic Surgery, Department of Molecular Medicine and Surgery, Karolinska University Hospital, Karolinska Institutet, 171 76 Stockholm, Sweden Edited by Marco Colonna, Washington University in St. Louis School of Medicine, St. Louis, MO, and approved January 27, 2021 (received for review August 18, 2020) Human adaptive-like “memory” CD56dimCD16+ natural killer (NK) We and others recently identified a subset of tissue-resident − cells in peripheral blood from cytomegalovirus-seropositive indi- CD49a+CD56brightCD16 NK cells in the human lung (14, 15). viduals have been extensively investigated in recent years and are The human lung is a frequent site of infection with viruses such currently explored as a treatment strategy for hematological can- as influenza virus and HCMV, as well as a reservoir for latent cers. -

The CD83 Reporter Mouse Elucidates the Activity of the CD83 Promoter in B, T, and Dendritic Cell Populations in Vivo
The CD83 reporter mouse elucidates the activity of the CD83 promoter in B, T, and dendritic cell populations in vivo Matthias Lechmann*, Naomi Shuman, Andrew Wakeham, and Tak W. Mak* Campbell Family Institute for Breast Cancer Research and Ontario Cancer Institute, University of Toronto, Toronto, ON, Canada M5G 2C1 Contributed by Tak W. Mak, July 1, 2008 (sent for review December 11, 2007) CD83 is the major surface marker identifying mature dendritic cells (22). However, truncated splice forms of CD83 have yet to be (DCs). In this study, we report the generation of reporter mice detected in human serum. At least some sCD83 may be generated expressing EGFP under the control of the CD83 promoter. We have by proteolytic cleavage of mCD83 (20). used these mice to characterize CD83 expression by various im- Although the CD83 ligand remains a mystery, analyses of gene- mune system cell types both in vivo and ex vivo and under targeted CD83-deficient mice have revealed that thymic CD83 steady-state conditions and in response to stimulation with a expression is crucial for the maturation of CD4ϩCD8ϩ thymocytes Toll-like receptor (TLR) ligand. With those mice we could prove in into CD4ϩ T cells (13, 14). In addition, CD83 may regulate the vivo that the CD83 promoter is highly active in all DCs and B cells intercellular interactions between DCs and peripheral T and B cells in lymphoid organs. Interestingly, this promoter activity in B cells (12, 23–25). In vitro culture of either human or murine lymphocytes mainly depended on the stage of development, is up-regulated in in the presence of sCD83 inhibits their proliferation (26, 27). -

Tocilizumab Contributes to the Inflammatory Status of Mature Dendritic Cells Through Interleukin-6 Receptor Subunits Modulation
ORIGINAL RESEARCH published: 16 August 2017 doi: 10.3389/fimmu.2017.00926 Tocilizumab Contributes to the inflammatory status of Mature Dendritic Cells through Interleukin-6 Receptor Subunits Modulation Daniel Meley1, Audrey Héraud 1, Valerie Gouilleux-Gruart2,3, Fabrice Ivanes1,4 and Florence Velge-Roussel 1,5* 1 EA 4245 Cellules Dendritiques, Immuno-modulation et Greffes, Université François-Rabelais de Tours, UFR de Médecine, Tours, France, 2 CNRS UMR 7292; Université François-Rabelais de Tours, UFR de Médecine, Tours, France, 3 Department of Immunology, CHRU de Tours, Tours, France, 4 Service de Cardiologie, CHRU de Tours, Tours, France, 5 UFR des Sciences Pharmaceutiques, Tours, France Tocilizumab, a humanized anti-IL-6 receptor α (IL-6Rα) is widely used in the treatment of a panel of pathologies such as adult and juvenile rheumatoid arthritis (RA) and the Edited by: systemic form of juvenile idiopathic arthritis in children. Its indications are expected to José Mordoh, Fundación Instituto Leloir, be largely extended to other inflammatory diseases in close future. Dendritic cells (DCs) Argentina appear to be deeply involved in the immunopathology of these diseases, yet the effects Reviewed by: of tocilizumab on these cells were poorly studied. In this study, we explored the effect Daniel Olive, Institut national de la santé et de la of tocilizumab on the regulation of IL-6R subunits [gp130, soluble form of IL-6Rα (sIL- recherche médicale, France 6Rα), and mIL-6Rα] in human monocyte-derived DCs. Human DCs were derived from Gilles Chiocchia, CD14+ monocytes purified with beads with IL-4 and granulocyte macrophage colony- Institut national de la santé et de la recherche médicale, France stimulating factor. -

CD83 Modulates B Cell Activation and Germinal Center Responses
CD83 Modulates B Cell Activation and Germinal Center Responses Lena Krzyzak, Christine Seitz, Anne Urbat, Stefan Hutzler, Christian Ostalecki, Joachim Gläsner, Andreas Hiergeist, This information is current as André Gessner, Thomas H. Winkler, Alexander of September 26, 2021. Steinkasserer and Lars Nitschke J Immunol published online 16 March 2016 http://www.jimmunol.org/content/early/2016/03/16/jimmun ol.1502163 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2016/03/16/jimmunol.150216 Material 3.DCSupplemental http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 26, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published March 16, 2016, doi:10.4049/jimmunol.1502163 The Journal of Immunology CD83 Modulates B Cell Activation and Germinal Center Responses Lena Krzyzak,* Christine Seitz,* Anne Urbat,† Stefan Hutzler,† Christian Ostalecki,‡ Joachim Gla¨sner,x Andreas Hiergeist,x Andre´ Gessner,x Thomas H. Winkler,{ Alexander Steinkasserer,*,1 and Lars Nitschke†,1 CD83 is a maturation marker for dendritic cells. -
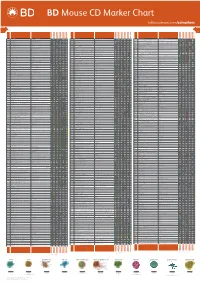
Mouse CD Marker Chart Bdbiosciences.Com/Cdmarkers
BD Mouse CD Marker Chart bdbiosciences.com/cdmarkers 23-12400-01 CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD1d CD1.1, CD1.2, Ly-38 Lipid, Glycolipid Ag + + + + + + + + CD104 Integrin b4 Laminin, Plectin + DNAX accessory molecule 1 (DNAM-1), Platelet and T cell CD226 activation antigen 1 (PTA-1), T lineage-specific activation antigen 1 CD112, CD155, LFA-1 + + + + + – + – – CD2 LFA-2, Ly-37, Ly37 CD48, CD58, CD59, CD15 + + + + + CD105 Endoglin TGF-b + + antigen (TLiSA1) Mucin 1 (MUC1, MUC-1), DF3 antigen, H23 antigen, PUM, PEM, CD227 CD54, CD169, Selectins; Grb2, β-Catenin, GSK-3β CD3g CD3g, CD3 g chain, T3g TCR complex + CD106 VCAM-1 VLA-4 + + EMA, Tumor-associated mucin, Episialin + + + + + + Melanotransferrin (MT, MTF1), p97 Melanoma antigen CD3d CD3d, CD3 d chain, T3d TCR complex + CD107a LAMP-1 Collagen, Laminin, Fibronectin + + + CD228 Iron, Plasminogen, pro-UPA (p97, MAP97), Mfi2, gp95 + + CD3e CD3e, CD3 e chain, CD3, T3e TCR complex + + CD107b LAMP-2, LGP-96, LAMP-B + + Lymphocyte antigen 9 (Ly9), -

Human CD83-Targeted Chimeric Antigen Receptor T Cells Prevent and Treat Graft-Versus-Host Disease
RESEARCH ARTICLE The Journal of Clinical Investigation Human CD83-targeted chimeric antigen receptor T cells prevent and treat graft-versus-host disease Bishwas Shrestha,1 Kelly Walton,2 Jordan Reff,1 Elizabeth M. Sagatys,3,4 Nhan Tu,4 Justin Boucher,4 Gongbo Li,4 Tayyebb Ghafoor,4 Martin Felices,2 Jeffrey S. Miller,2 Joseph Pidala,4,5 Bruce R. Blazar,6 Claudio Anasetti,4,5 Brian C. Betts,2 and Marco L. Davila1,4,5 1Department of Immunology, Moffitt Cancer Center, Tampa, Florida, USA. 2Division of Hematology, Oncology, and Transplantation, Department of Medicine, Masonic Cancer Center, University of Minnesota, Minneapolis, Minnesota, USA. 3Department of Hematopathology and Laboratory Medicine, Moffitt Cancer Center, Tampa, Florida, USA. 4Department of Oncologic Sciences, University of South Florida, Tampa, Florida, USA. 5Department of Blood and Marrow Transplantation and Cellular Immunotherapy, Moffitt Cancer Center, Tampa, Florida, USA. 6Division of Blood and Marrow Transplantation, Department of Pediatrics, Masonic Cancer Center, University of Minnesota, Minneapolis, Minnesota, USA. Graft-versus-host disease (GVHD) remains an important cause of morbidity and mortality after allogeneic hematopoietic cell transplantation (allo-HCT). For decades, GVHD prophylaxis has included calcineurin inhibitors, despite their incomplete efficacy and impairment of graft-versus-leukemia (GVL). Distinct from pharmacologic immune suppression, we have developed what we believe is a novel, human CD83-targeted chimeric antigen receptor (CAR) T cell for GVHD prevention. CD83 is expressed on allo-activated conventional CD4+ T cells (Tconvs) and proinflammatory dendritic cells (DCs), which are both implicated in GVHD pathogenesis. Human CD83 CAR T cells eradicate pathogenic CD83+ target cells, substantially increase the ratio of regulatory T cells (Tregs) to allo-activated Tconvs, and provide durable prevention of xenogeneic GVHD. -

Human Small Cell Lung Carcinoma and Carcinoid Tumor Regulate Dendritic Cell Maturation and Function Nora S
Human Small Cell Lung Carcinoma and Carcinoid Tumor Regulate Dendritic Cell Maturation and Function Nora S. Katsenelson, Galina V. Shurin, Svetlana N. Bykovskaia, Jeffrey Shogan, Michael R. Shurin Department of Pathology (NSK, GVS, MRS), University of Pittsburgh Medical Center, University of Pittsburgh Cancer Institute, Pittsburgh, Pennsylvania; and Bone Marrow Transplantation Program (SNB, JS), Allegheny General Hospital, Pittsburgh, Pennsylvania KEY WORDS: Apoptosis, Bronchial carcinoid tumor, The induction of apoptosis in dendritic cells (DC) is Dendritic cell, Immunohistochemistry, Small-cell a key mechanism by which tumors escape immune lung carcinoma. recognition and elimination. In fact, a number of Mod Pathol 2001;14(1):40–45 studies have showed the correlation between the number of DC within the tumor and the clinical Immune responses to tumor antigens are the result prognosis, suggesting that increased infiltration of of reciprocal communication between antigen- tumor tissue by DC was associated with better pa- presenting cells, T cells, and B cells. The most po- tient survival and low incidence of metastatic dis- tent professional antigen-presenting cells are den- ease. We compared the number of DC and their dritic cells (DC), which are considered to be solely distribution pattern in human small-cell lung car- responsible for initiating primary immune re- cinoma and bronchial carcinoid tumor (CT) tissues. sponses, including antitumor immunity (1, 2). DC Immunohistochemical analysis revealed the pres- recognize and take up antigen, process it, and ence of cells expressing DC markers CD1a and CD83 present antigenic peptides to T cells in a major in small-cell lung carcinoma tissues and the com- histocompatibility complex (MHC)–restricted man- plete absence of these cells in CT samples. -

Insulin-Like Growth Factor I Promotes Maturation and Inhibits Apoptosis of Immature Cord Blood Monocyte–Derived Dendritic Cells Through MEK and PI 3-Kinase Pathways
0031-3998/03/5406-0919 PEDIATRIC RESEARCH Vol. 54, No. 6, 2003 Copyright © 2003 International Pediatric Research Foundation, Inc. Printed in U.S.A. Insulin-Like Growth Factor I Promotes Maturation and Inhibits Apoptosis of Immature Cord Blood Monocyte–Derived Dendritic Cells through MEK and PI 3-Kinase Pathways ENMEI LIU, HELEN K.W. LAW, AND YU-LUNG LAU Department of Paediatrics and Adolescent Medicine, Faculty of Medicine, The University of Hong Kong, Queen Mary Hospital, Pokfulam, Hong Kong, China ABSTRACT IGF-I has profound effects on the immune system. We pre- DC maturation and apoptosis. On the contrary, neutralizing viously reported that IGF-I promoted cord blood (CB)-naïve TNF-␣ significantly increased the IGF-I–induced up-regulation T-cell maturation and now show that IGF-I promoted maturation of CD83 and CD40. We conclude that IGF-I has maturation and of CB monocyte–derived dendritic cells (DC) with up-regulation survival effects on CB DC. These effects are mediated through of CD83, CD86, CD40, and major histocompatibility complex both MEK and PI 3-kinase pathways but not through the IGF-I (MHC) class II molecules, and down-regulation of mannose induction of TNF-␣ production by the DC. (Pediatr Res 54: receptor. Furthermore, IGF-I inhibited apoptosis of CB DC and 919–925, 2003) increased the production of tumor necrosis factor ␣ (TNF-␣). These effects were blocked by specific mitogen-activated protein Abbreviations kinase kinase (MEK) inhibitor (PD98059) and phosphoinositol AV, annexin V 3-kinase inhibitor (LY294002). PD98059 partially inhibited the CB, cord blood IGF-I–induced up-regulation of MHC class II. -

The Analysis of CD83 Expression on Human Immune Cells Identifies a Unique CD83 + -Activated T Cell Population
The Analysis of CD83 Expression on Human Immune Cells Identifies a Unique CD83 + -Activated T Cell Population This information is current as Xinsheng Ju, Pablo A. Silveira, Wei-Hsun Hsu, Zehra of October 1, 2021. Elgundi, Renz Alingcastre, Nirupama D. Verma, Phillip D. Fromm, Jennifer L. Hsu, Christian Bryant, Ziduo Li, Fiona Kupresanin, Tsun-Ho Lo, Candice Clarke, Kenneth Lee, Helen McGuire, Barbara Fazekas de St. Groth, Stephen R. Larsen, John Gibson, Kenneth F. Bradstock, Georgina J. Clark and Derek N. J. Hart Downloaded from J Immunol 2016; 197:4613-4625; Prepublished online 11 November 2016; doi: 10.4049/jimmunol.1600339 http://www.jimmunol.org/content/197/12/4613 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2016/11/11/jimmunol.160033 Material 9.DCSupplemental References This article cites 50 articles, 24 of which you can access for free at: http://www.jimmunol.org/content/197/12/4613.full#ref-list-1 by guest on October 1, 2021 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc.