Surgical Sutures: an Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Suture Assembled with Polymeric Drug-Delivery Sheet for Sustained, Local Pain Relief
Acta Biomaterialia 9 (2013) 8318–8327 Contents lists available at SciVerse ScienceDirect Acta Biomaterialia journal homepage: www.elsevier.com/locate/actabiomat Surgical suture assembled with polymeric drug-delivery sheet for sustained, local pain relief Ji Eun Lee a,1, Subin Park b,1, Min Park a, Myung Hun Kim a, Chun Gwon Park a, Seung Ho Lee a, ⇑ ⇑ Sung Yoon Choi a, Byung Hwi Kim b, Hyo Jin Park c, Ji-Ho Park d, Chan Yeong Heo e,f, , Young Bin Choy a,b, a Interdisciplinary Program in Bioengineering, College of Engineering, Seoul National University, Seoul 110-799, Republic of Korea b Department of Biomedical Engineering, College of Medicine and Institute of Medical & Biological Engineering, Medical Research Center, Seoul National University, Seoul 110-799, Republic of Korea c Department of Pathology, Seoul National University Bundang Hospital, Seongnam 463-707, Republic of Korea d Department of Bio and Brain Engineering, Korea Advanced Institute of Science and Technology, Daejeon 305-701, Republic of Korea e Department of Plastic Surgery and Reconstructive Surgery, Seoul National University College of Medicine, Seoul 110-799, Republic of Korea f Department of Plastic Surgery and Reconstructive Surgery, Seoul National University Bundang Hospital, Seongnam 463-707, Republic of Korea article info abstract Article history: Surgical suture is a strand of biocompatible material designed for wound closure, and therefore can be a Received 23 January 2013 medical device potentially suitable for local drug delivery to treat pain at the surgical site. However, the Received in revised form 21 May 2013 preparation methods previously introduced for drug-delivery sutures adversely influenced the mechan- Accepted 3 June 2013 ical strength of the suture itself – strength that is essential for successful wound closure. -
Suture Manual
Suture Manual REPAIR AND REGENERATE Suture Manual List of Contents Introduction Page 3 Principles Page 6 Surgical needles Page 12 Sutures Page 15 Manufacture and packaging Page 28 Organisational aids Page 33 No claim is made for the completeness of the information given about the suture material: this must be gathered from the relevant literature for healthcare specialists. More detailed information concerning the materials can be obtained from the information leaflets in each package. We shall be pleased to send these on request. Visit our website: www.resorba.com for constantly updated and comprehensive information on our products and developments. 2 Introduction In nature, damaged or destroyed tissue Absorbable materials, e.g. PGA RESORBA®, Requirements for an layers must be covered over quickly to support the natural healing process until ideal suture: preserve the integrity and functions of form and function are restored. Such • high tensile strength the organism. We humans have copied materials are subsequently metabolised • high knot security this response from nature. by the organism. • good tie down • no capillary function It is the aim of modern wound care, first Non-absorbable suture materials (e.g. • good tissue tolerance and foremost, to preserve intact tissues MOPYLEN®) guarantee lasting support • easy passage through tissue and support the damaged parts. Our su- and best biotolerance, which is especially • sterile presentation ture materials, based on biocompatible essential for long-term implants. raw materials, make possible the targeted application of every kind of wound care, A large number of suture materials are The optimum use of any and guarantees the best possible tissue nowadays used in wound closure. -

Tissue Response to Suture Materials (4 Different Sutures) Used in Fascia Repair in Single-Port Laparoscopic Cholecystectomy
HAYDARPAŞA NUMUNE MEDICAL JOURNAL DOI: 10.14744/hnhj.2017.88597 Haydarpasa Numune Med J 2018;58(2):67–73 ORIGINAL ARTICLE hnhtipdergisi.com Tissue Response to Suture Materials (4 Different Sutures) Used in Fascia Repair in Single-Port Laparoscopic Cholecystectomy Sina Ferahman1, Turgut Dönmez2, Oğuzhan Sunamak3, Selim Saraçoğlu1, Demet Ferahman4 1Department of General Surgery, Istanbul University Cerrahpasa Faculty of Medicine, Istanbul, Turkey 2Department of General Surgery, Lutfiye Nuri Burat State Hospital, Istanbul, Turkey 3Department of General Surgery, Haydarpasa Numune Training and Research Hospital, Istanbul, Turkey 4Department of Internal Medicine, Istanbul University Cerrahpasa Faculty of Medicine, Istanbul, Turkey Abstract Introduction: This study aimed to evaluate the tissue inflammatory response to suture materials used for fascia repair in single-port laparoscopic cholecystectomy. Methods: The medical records of 65 patients who underwent single-port laparoscopic cholecystectomy in general surgery clinics at state hospitals between December 2013 and January 2015 were retrospectively analyzed. Tissue reaction to the suture materials used for repairing a 2-cm fascia incision in single-port laparoscopic cholecystectomy was evaluated. Tissue reaction to the following suture materials used for repairing the fascia defect was analyzed: non-absorbable braided polyester, non- absorbable monofilament polypropylene, absorbable polyfilament polyglactin, and absorbable monofilament poldioxanone. Results: Non-absorbable braided polyester was used in 14 patients, non-absorbable monofilament polypropylene in 25 pa- tients, absorbable polyfilament polyglactin in 10 patients, and absorbable monofilament poldioxanone in 16 patients. Pa- tients were followed up for at least 6 months. Fourteen patients who had a foreign body reaction could not be treated by antibiotherapy and therefore underwent surgery to excise the sutures responsible for inducing the reaction. -

Natural Cellulose Fibers for Surgical Suture Applications
polymers Article Natural Cellulose Fibers for Surgical Suture Applications María Paula Romero Guambo 1, Lilian Spencer 1, Nelson Santiago Vispo 1 , Karla Vizuete 2 , Alexis Debut 2 , Daniel C. Whitehead 3 , Ralph Santos-Oliveira 4 and Frank Alexis 1,5,* 1 School of Biological Sciences and Engineering, Yachay Tech University, Urcuquí, Imbabura 100115, Ecuador; [email protected] (M.P.R.G.); [email protected] (L.S.); [email protected] (N.S.V.) 2 Center of Nanoscience and Nanotechnology, Universidad de las Fuerzas Armadas ESPE, Sangolquí 1715231, Ecuador; [email protected] (K.V.); [email protected] (A.D.) 3 Department of Chemistry, Clemson University, Clemson, SC 29634, USA; [email protected] 4 Brazilian Nuclear Energy Commission, Nuclear Engineering Institute, Laboratory of Nanoradiopharmaceuticals and Synthesis of Novel Radiopharmaceuticals, Rio de Janeiro 21941906, Brazil; [email protected] 5 Biodiverse Source, San Miguel de Urcuquí 100651, Ecuador * Correspondence: [email protected] Received: 10 November 2020; Accepted: 11 December 2020; Published: 18 December 2020 Abstract: Suture biomaterials are critical in wound repair by providing support to the healing of different tissues including vascular surgery, hemostasis, and plastic surgery. Important properties of a suture material include physical properties, handling characteristics, and biological response for successful performance. However, bacteria can bind to sutures and become a source of infection. For this reason, there is a need for new biomaterials for suture with antifouling properties. Here we report two types of cellulose fibers from coconut (Cocos nucifera) and sisal (Agave sisalana), which were purified with a chemical method, characterized, and tested in vitro and in vivo. -

Tissue Anchoring Performance of Barbed Surgical Sutures for Tendon Repair 1Hui Cong, 2Simon Roe, 3Peter Mente, 3Jacqueline H
Tissue Anchoring Performance of Barbed Surgical Sutures for Tendon Repair 1Hui Cong, 2Simon Roe, 3Peter Mente, 3Jacqueline H. Cole, 4Gregory Ruff, and 1, 5Martin W. King 1College of Textiles, 2College of Veterinary Medicine, 3Dept. Biomedical Engineering, North Carolina State University, Raleigh, NC 27695, 4Vilcom Circle, Chapel Hill, NC 27514, 5Donghua University, Shanghai, China 201620. Introduction: Barbed surgical sutures are approved by the US Food & Drug Administration for use in plastic and cosmetic surgical procedures [1-3]. The main advantage of the barbed surgical suture is that the barbs project out, penetrate, and anchor with surrounding tissue along the entire suture’s length, thus eliminating the need for tying a knot. While this barbed suture technology is widely accepted clinically for skin wound closure, its suitability Figure 2. Tendon/suture pullout test model. in other applications, such as tendon repair, has not been accepted [4]. Increasing the tissue anchoring performance Results: Table 1 shows the average results of barb generated from the protruding barbs is a key factor to geometry and tensile pullout force measured on the nylon expanding the application of barbed surgical sutures into 6 and PP barbed sutures. Based on the t-test result, the PP other fields. The initial objective of the current study was barbed sutures had a significantly higher anchoring to develop a novel in vitro tendon/suture model for performance compared to the nylon 6 sutures (p=0.03). measuring the anchoring performance of barbed sutures in porcine tendon tissue. The second objective was to Table 1. Cut angle, cut depth and pullout force measured compare the tendon anchoring performance of nylon 6 for both nylon 6 and PP barbed sutures. -
SURGICAL SUTURE Types, Indications and Features
SURGICAL SUTURE Types, indications and features OVERVIWE The surgical suture is a medical device used in closing wound edges or repairing tissue damage, there are many types of sutures with different specification suitable for wide variety uses. Sutures are classified according to many characteristics such as: ❖ All surgical sutures are either, absorbable sutures which decomposed in the body and doesn’t need to be removed by doctor, or non-absorbable sutures which need to be removed from surgeon after wound healing. (these is the basic classification). ❖ It’s classified according to structure of material either monofilament suture composed of a single fiber, or multifilament (braided) composed of many small fibers braided together ❖ According to origin of suture material, either natural like silk, cotton or catgut which made from sheep intestines, or synthetic; like poly Glycolide, poly lactic acid, nylon, poly ester ❖ And several another classification like coated or not coated, dyed or undyed. The ideal suture material should have several basic characteristics to be high in quality and for minimal risk as following: • the composition of suture material can be used in many surgical procedures. • Without any foreign-body left inside body, irritants that caused tissue reaction. • Surgical suture should be non-antigenic and non-pyrogenic. • Should be non-electrolytic • Sterile by any sterilization method such as sterilization by ethylene oxide or by gamma radiation. as the sterilization method are critical to minimize a infection of wound. • it should have a high tensile strength according to material size and material structure. • it’s easy to handle. • uniform size according to suture diameter. -
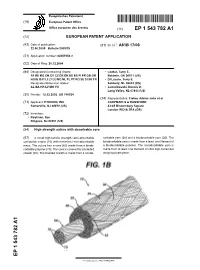
High Strength Suture with Absorbable Core
Europäisches Patentamt *EP001543782A1* (19) European Patent Office Office européen des brevets (11) EP 1 543 782 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.7: A61B 17/06 22.06.2005 Bulletin 2005/25 (21) Application number: 04257953.2 (22) Date of filing: 20.12.2004 (84) Designated Contracting States: • Lawler, Terry E. AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Baldwin, GA 30511 (US) HU IE IS IT LI LT LU MC NL PL PT RO SE SI SK TR • Di Luccio, Terry E. Designated Extension States: Ashbury, NL 08802 (US) AL BA HR LV MK YU • Jamiolkowski, Dennis D. Long Valley, NL 07853 (US) (30) Priority: 18.12.2003 US 740024 (74) Representative: Fisher, Adrian John et al (71) Applicant: ETHICON, INC. CARPMAELS & RANSFORD Somerville, NJ 08876 (US) 43-45 Bloomsbury Square London WC1A 2RA (GB) (72) Inventors: • Koyfman, Ilya Ringoes, NJ 08551 (US) (54) High strength suture with absorbable core (57) A novel high tensile strength semi-absorbable sorbable yarn (30) and a bioabsorbable yarn (35). The composite suture (10) with minimized non-absorbable bioabsorbable yarn is made from a least one filament of mass. The suture has a core (60) made from a bioab- a bioabsorbable polymer. The nonabsorbable yarn is sorbable polymer (70). The core is covered by a braided made from at least one filament of ultra high molecular sheath (20). The braided sheath is made from a nonab- weight polyethylene. EP 1 543 782 A1 Printed by Jouve, 75001 PARIS (FR) EP 1 543 782 A1 Description Technical Field 5 [0001] The field of art to which this invention relates is surgical sutures, in particular, surgical sutures having both bioabsorbable and nonabsorbable components. -

Influence of Different Types of Surgical Suture Material on the Intensity of Tissue Reaction in Oral Cavity
Zbornik Matice srpske za prirodne nauke / Proc. Nat. Sci, Matica Srpska Novi Sad, ¥ 115, 91—99, 2008 UDC 616.31-089 DOI:10.2298/ZMSPN0815091M Siniša M. Mirkoviã Ljubiša D. Dÿambas Sreãko Ð. Selakoviã Faculty of Medicine Novi Sad, Clinic of Dentistry of Vojvodina Hajduk Veljkova 12, Novi Sad, Serbia INFLUENCE OF DIFFERENT TYPES OF SURGICAL SUTURE MATERIAL ON THE INTENSITY OF TISSUE REACTION IN ORAL CAVITY ABSTRACT: Throughout the history the most diverse suture material have been used for closing and suturing surgical wounds. The four basic features of suture material are des- cribed: knot safety, stretch capacity, tissue reactivity and wound safety. Tissue reaction, even the minimum one, which develops during the first to seven days after applying the su- ture in the tissue. The aim of this study was to investigate influence of a monofilament suture material (nylon) on the intensity of local tissue reaction in experimental conditions, and to compare it with the multifilament suture used in the routine practice of oral surgery (silk). This investigation is a prospective experimental study carried out on Wistar rats. The experiment included 30 animals, in which Black Silk (thickness 4-1) and Nylon (thickness 4-0) were applied in the upper and lower jaw, respectively. To monitor tissue reaction on different suture materials the following parameters were used: coagulum formation, presence of polymorphonuclear leukocytes, presence of macrophages and granuloma, formation of epithelial bridge and connective tissue, collagen synthesis, granulomatous tissue formation and presence of fibrous tissue. After comparing parameters for the intensity of tissue reaction to the investigate su- ture materials by suturing the oral mucosa, certain advantage could be given to the monofi- lament suture materials. -

Applying Basic Principles of Surgery May Pave the Way for More Effective Endoscopic Bariatric Techniques
Published online: 2021-06-17 Innovation forum Applying basic principles of surgery may pave the way for more effective endoscopic bariatric techniques Authors Kiyoshi Hashiba1, Carlos Alberto Cappellanes1, Pablo Rodrigo de Siqueira1, Antonio Carlos Conrado2,BrunoRibeiro3, Fernando Pavinato Marson1, Bruno Gregnanin Pedron1 Institutions ABSTRACT 1 Department of Digestive Endoscopy, Hospital Sírio- Background and study aims In the last decade, gastroen- Libanês, São Paulo, Brazil terologists have been attempting to use endoscopy to re- – 2 Endoscopy Unit, Hospital da Restauração Recife, Brazil produce the great success of traditional surgical suture – 3 Endoscopy Division, UF Health Jacksonville techniques. Despite recent advances, we still lack a reliable Jacksonville, Florida, United States method that results in a permanent suture with minimal in- cidence of suture failure. This was an experimental study in submitted 20.8.2020 pigs with an innovative technique that applied basic surgi- accepted after revision 15.2.2021 cal concepts to endoscopy to evaluate the effectiveness of a novel suture technique. Bibliography Methods The procedures were performed on six live pigs – Endosc Int Open 2021; 09: E1049 E1054 under general anesthesia. Endoscopic mucosal resection DOI 10.1055/a-1451-3854 (EMR) first was performed in the stomach, exposing the ISSN 2364-3722 submucosal or muscularis propria layers. A novel device, a © 2021. The Author(s). transparent chamber cap (DASE), was developed to aspirate This is an open access article published by Thieme under the terms of the Creative the gastric wall, allowing the sutures to reach deep layers. Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. -

Drug Eluting Sutures: a Recent Update
Journal of Applied Pharmaceutical Science Vol. 9(07), pp 111-123, July, 2019 Available online at http://www.japsonline.com DOI: 10.7324/JAPS.2019.90716 ISSN 2231-3354 Drug eluting sutures: A recent update Anureet Arora1, Geeta Aggarwal2, Janita Chander1, Paramjot Maman3, Manju Nagpal1* 1Chitkara College of Pharmacy, Chitkara University, Chandigarh Patiala National Highway, Patiala 140401, India. 2Delhi Pharmaceutical Sciences and Research University, Govt. of NCT of Delhi, Pushp Vihar, Sector III, New Delhi 110017, India. 3Paraxel Solutions Ltd, Rajiv Gandhi IT Park, Chandigarh, India. ARTICLE INFO ABSTRACT Received on: 12/03/2019 The main use of surgical sutures is to assist closure and healing of trauma-induced as well as surgical wounds. This Accepted on: 04/05/2019 is done by upholding wound tissues together in order to facilitate the healing process. A huge variety of sutures Available online: 01/07/2019 are available for the medical purposes, e.g., bio active sutures, knot-less sutures, electronic sutures, drug-eluting sutures, anti-microbial sutures, and stem cells containing sutures. Sutures increase the capabilities to improve tissue approximation and wound healing. Sutures with drug eluting property are the advanced type of sutures being used for Key words: surgical purpose via delivery of drug to the specified area. Various new strategies develop the effectiveness of sutures Surgical, smart sutures, to be used as physical entity to get better biologically active component which enables the delivery of various desirable ophthalmics, electrospinning, drugs and cells to the affected site. Ideal modified sutures should not only retain its mechanical integrity during the antibacterial. -

New Suturing System for Flexible Endoscopy in the Gastrointestinal Tract
Japanese Journal of Gastroenterology and Hepatology Research Article ISSN 2435-121 Volume 6 New Suturing System for Flexible Endoscopy in The Gastrointestinal Tract Fuchs KH*, Neki K, Lee AM, Dominguez R, Broderick R, Sandler B and Horgan S Department of Surgery, University of California San Diego, Center for the Future of Surgery, La Jolla, CA, USA *Corresponding author: Received: 09 Feb 2021 Copyright: Karl-Hermann Fuchs, Accepted: 26 Feb 2021 ©2021 Fuchs KH, This is an open access article distributed un- Department of Surgery, University of California Published: 02 Mar 2021 der the terms of the Creative Commons Attribution License, San Diego, Center for the Future of Surgery, 9500 which permits unrestricted use, distribution, and build upon Gilman Drive, MC: 0740, La Jolla, CA 92093, USA, your work non-commercially. E-mail: [email protected] Citation: Fuchs KH. New Suturing System for Flexible Endoscopy in The Gastrointestinal Tract. Japanese J Gstro Hepato. 2021; V6(2): 1-6 1. Abstract 2. Introduction 1.1. Background: We have assessed an approach, enabling an en- Suturing in interventional flexible endoscopy is a challenging prob- doscopist together with surgical assistance to perform endoscopic lem considering the level of complexity. Early endoscopic technol- sutures based on minimally-invasive principles. ogy lacked the deep bite necessary to reach the muscular is of the 1.2. Aim: Assessment of a new suturing-system in the gastrointes- gut wall [1-7]. Very complex endoscopic platforms had been devel- tinal tract. oped, but have not reached the market for a number of reasons such as expensive technology, cumbersome technique with long learn- 1.3. -

Hybrid Suture with Monofilament and Braided Construction
(19) TZZ _T (11) EP 2 829 286 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 28.01.2015 Bulletin 2015/05 A61L 17/10 (2006.01) (21) Application number: 14178353.0 (22) Date of filing: 24.07.2014 (84) Designated Contracting States: (72) Inventors: AL AT BE BG CH CY CZ DE DK EE ES FI FR GB • Dreyfuss, Peter J GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO Naples, FL Florida 34108 (US) PL PT RO RS SE SI SK SM TR • Dooney, JR., Thomas Designated Extension States: Naples, FL Florida 34109 (US) BA ME (74) Representative: Ehrner & Delmar Patentbyrå AB (30) Priority: 24.07.2013 US 201361857818 P Box 10316 100 55 Stockholm (SE) (71) Applicant: Arthrex, Inc. Naples, FL 34108-1945 (US) (54) Hybrid suture with monofilament and braided construction (57) A hybrid monofilament/braided surgical suture polyethylene or polypropylene filament, among many that combines a monofilament with a braided construc- others. The stiffness properties of the hybrid surgical su- tion. The hybrid surgical suture may be formed by braid- ture allow the suture to be pushed through small and very ing yarns of high tenacity fibers tightly over a core in the small diameter tubes and cannulations (such as Lasso form of a monofilament yarn. The monofilament may be instruments, for example) yet fix securely with existing any type of material, for example, a nylon, silk, polyester, fixation devices (such as knotless suture anchors). EP 2 829 286 A1 Printed by Jouve, 75001 PARIS (FR) 1 EP 2 829 286 A1 2 Description not a coreless construct anymore.