OEU Kenya Kitale DR Quantitative Study Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Towards a Housing Strategy to Support Industrial Decentralization: a Case Study of Athi River Town
I TOWARDS A HOUSING STRATEGY TO SUPPORT INDUSTRIAL DECENTRALIZATION: A CASE STUDY OF ATHI RIVER TOWN HENRY MUTHOKA MWAU B.Sc.(Hons) Nairobi, 1986. \ A THESIS SUBMITTED IN PART FULFILMENT FOR THE DEGREE OF MASTER OF ARTS (PLANNING) IN THE UNIVERSITY OF NAIROBI. ;* * * N AND «eg<onal planning OFPA.TTVENT " A - U lT r & ARCHITECTURE, OCSICN -NO OEVFLOPMEn t ' ONIv. RSiTY OK NAlKOil ■“"'Sttrffftas ’ NAIROBI, KENYA (ii) DECLARATION This thesis is my original work and*has not been presented for a degree in any other university• Signed HENRY M. KWAU This thesis has been submitted for examination with my approval as University Supervisor, Signed DR. P.0. ONOIEGE (SUPERVISOR) *av*i*n t o „ ACKNOWLEDGEMENTS This study would not have been successful without the assistance of many people in various institutions. It therefore gives me pleasure to mention a few and express my sincere appreciation for their assistance. First, I would like to thank the Directorate of Personnel Management (DPM)|through the Department of Physical Planning, Ministry of Local Government and Physical Planning whose sponsorship made this work possible. Their collaboration with the department of Urban and Regional Planning, especially through the Chairman, Mr. Z. Maleche, University of Nairobi, made the training course successful. I am greatly indebted to Dr. P. 0. Ondiege, the project supervisor and lecturer in the department, for his guidance throughout the research work. Thanks go to Mr. P. Karanja, the then acting Town Clerk/Treasurer, at time of research work and Mr. Kyatha, both of Athi River Town Council, whose co-operation eased the field work task. -
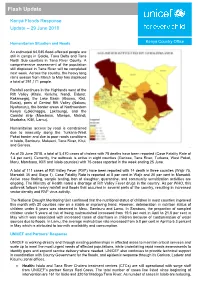
Flash Update
Flash Update Kenya Floods Response Update – 29 June 2018 Humanitarian Situation and Needs Kenya Country Office An estimated 64,045 flood-affected people are still in camps in Galole, Tana Delta and Tana North Sub counties in Tana River County. A comprehensive assessment of the population still displaced in Tana River will be completed next week. Across the country, the heavy long rains season from March to May has displaced a total of 291,171 people. Rainfall continues in the Highlands west of the Rift Valley (Kitale, Kericho, Nandi, Eldoret, Kakamega), the Lake Basin (Kisumu, Kisii, Busia), parts of Central Rift Valley (Nakuru, Nyahururu), the border areas of Northwestern Kenya (Lokichoggio, Lokitaung), and the Coastal strip (Mombasa, Mtwapa, Malindi, Msabaha, Kilifi, Lamu). Humanitarian access by road is constrained due to insecurity along the Turkana-West Pokot border and due to poor roads conditions in Isiolo, Samburu, Makueni, Tana River, Kitui, and Garissa. As of 25 June 2018, a total of 5,470 cases of cholera with 78 deaths have been reported (Case Fatality Rate of 1.4 per cent). Currently, the outbreak is active in eight counties (Garissa, Tana River, Turkana, West Pokot, Meru, Mombasa, Kilifi and Isiolo counties) with 75 cases reported in the week ending 25 June. A total of 111 cases of Rift Valley Fever (RVF) have been reported with 14 death in three counties (Wajir 75, Marsabit 35 and Siaya 1). Case Fatality Rate is reported at 8 per cent in Wajir and 20 per cent in Marsabit. Active case finding, sample testing, ban of slaughter, quarantine, and community sensitization activities are ongoing. -

Annual Report of the Colonies, Kenya, 1936
COLONIAL REPORTS—ANNUAL • \ No. 1806 ^Vnnual Report on the Social and Economic Progress KENYA COLONY AND PROTECTORATE, r936 ; (Fot Reports for X934. and 193'$tt* tftil tf$'$to&*ifyjii:[ respectively (Price 2s. od, each)) Crvw* Copyright Restmd LONDON . 1 ;• ; ' • PRINTED AND PUBLISHED BY ttl$ MAJE$TY^S STATIONERY PFJFIC8 To be eurchaaed directly from H.M. STATIONERY OFFICE it the following addressee Adaatral House, Ktngsway, London, W.Ca f :iu George Street, Edinburgh *) af York Street, Manchester 1 $ t St Andrew's Crescent, Cardiff) V 3o Chichwter Street. Belfast; or through any bookseller ' >937 !. 1 : Price 2s. 6^ net ; ADVERTISEMENT BARCLAYS BANK (DOMINION, COLONIAL AND OVERSEAS) BRANCHES IN KENYA ELDORET - KAKAMEGA - KISUMU KITALE - MOMBASA - NAIROBI - NAKURU AND THROUGHOUT THE UNION OF SOUTH AFRICA KENYA - TANGANYIKA - UGANDA NYASALAND NORTHERN AND SOUTHERN RHODESIA PORTUGUESE EAST AFRICA SOUTH-WEST AFRICA BRITISH WEST AFRICA CYPRUS - MALTA - GIBRALTAR SUDAN - PALESTINE MAURITIUS BRITISH WEST INDIES BRITISH GUIANA LONDON - LIVERPOOL - MANCHESTER HAMBURG - - - NEW YORK HEAD OFFICE: 54, LOMBARD STREET, LONDON, E.C.3 BARCLAYS BANK (CANADA), MONTREAL AND TORONTO 44715 ADVERTISEMENT THE BOARD OF TRADE JOURNAL For over fifty years the Board of Trade Journal has been the source of official infor mation on all aspects of British and world trade. To-day when commercial and trade regulations and tariffs have increased through out the world in number and complexity, there is greater need than ever before for the reliable guide which the Board of Trade Journal provides in the search for markets overseas. The Journal gives a faithful index of the economic position at home as revealed in statistics of imports and exports, of production, and of retail trade, and shipping, and in wholesale and retail prices. -

KENYA POPULATION SITUATION ANALYSIS Kenya Population Situation Analysis
REPUBLIC OF KENYA KENYA POPULATION SITUATION ANALYSIS Kenya Population Situation Analysis Published by the Government of Kenya supported by United Nations Population Fund (UNFPA) Kenya Country Oce National Council for Population and Development (NCPD) P.O. Box 48994 – 00100, Nairobi, Kenya Tel: +254-20-271-1600/01 Fax: +254-20-271-6058 Email: [email protected] Website: www.ncpd-ke.org United Nations Population Fund (UNFPA) Kenya Country Oce P.O. Box 30218 – 00100, Nairobi, Kenya Tel: +254-20-76244023/01/04 Fax: +254-20-7624422 Website: http://kenya.unfpa.org © NCPD July 2013 The views and opinions expressed in this report are those of the contributors. Any part of this document may be freely reviewed, quoted, reproduced or translated in full or in part, provided the source is acknowledged. It may not be sold or used inconjunction with commercial purposes or for prot. KENYA POPULATION SITUATION ANALYSIS JULY 2013 KENYA POPULATION SITUATION ANALYSIS i ii KENYA POPULATION SITUATION ANALYSIS TABLE OF CONTENTS LIST OF ACRONYMS AND ABBREVIATIONS ........................................................................................iv FOREWORD ..........................................................................................................................................ix ACKNOWLEDGEMENT ..........................................................................................................................x EXECUTIVE SUMMARY ........................................................................................................................xi -

Download List of Physical Locations of Constituency Offices
INDEPENDENT ELECTORAL AND BOUNDARIES COMMISSION PHYSICAL LOCATIONS OF CONSTITUENCY OFFICES IN KENYA County Constituency Constituency Name Office Location Most Conspicuous Landmark Estimated Distance From The Land Code Mark To Constituency Office Mombasa 001 Changamwe Changamwe At The Fire Station Changamwe Fire Station Mombasa 002 Jomvu Mkindani At The Ap Post Mkindani Ap Post Mombasa 003 Kisauni Along Dr. Felix Mandi Avenue,Behind The District H/Q Kisauni, District H/Q Bamburi Mtamboni. Mombasa 004 Nyali Links Road West Bank Villa Mamba Village Mombasa 005 Likoni Likoni School For The Blind Likoni Police Station Mombasa 006 Mvita Baluchi Complex Central Ploice Station Kwale 007 Msambweni Msambweni Youth Office Kwale 008 Lunga Lunga Opposite Lunga Lunga Matatu Stage On The Main Road To Tanzania Lunga Lunga Petrol Station Kwale 009 Matuga Opposite Kwale County Government Office Ministry Of Finance Office Kwale County Kwale 010 Kinango Kinango Town,Next To Ministry Of Lands 1st Floor,At Junction Off- Kinango Town,Next To Ministry Of Lands 1st Kinango Ndavaya Road Floor,At Junction Off-Kinango Ndavaya Road Kilifi 011 Kilifi North Next To County Commissioners Office Kilifi Bridge 500m Kilifi 012 Kilifi South Opposite Co-Operative Bank Mtwapa Police Station 1 Km Kilifi 013 Kaloleni Opposite St John Ack Church St. Johns Ack Church 100m Kilifi 014 Rabai Rabai District Hqs Kombeni Girls Sec School 500 M (0.5 Km) Kilifi 015 Ganze Ganze Commissioners Sub County Office Ganze 500m Kilifi 016 Malindi Opposite Malindi Law Court Malindi Law Court 30m Kilifi 017 Magarini Near Mwembe Resort Catholic Institute 300m Tana River 018 Garsen Garsen Behind Methodist Church Methodist Church 100m Tana River 019 Galole Hola Town Tana River 1 Km Tana River 020 Bura Bura Irrigation Scheme Bura Irrigation Scheme Lamu 021 Lamu East Faza Town Registration Of Persons Office 100 Metres Lamu 022 Lamu West Mokowe Cooperative Building Police Post 100 M. -

County Name County Code Location
COUNTY NAME COUNTY CODE LOCATION MOMBASA COUNTY 001 BANDARI COLLEGE KWALE COUNTY 002 KENYA SCHOOL OF GOVERNMENT MATUGA KILIFI COUNTY 003 PWANI UNIVERSITY TANA RIVER COUNTY 004 MAU MAU MEMORIAL HIGH SCHOOL LAMU COUNTY 005 LAMU FORT HALL TAITA TAVETA 006 TAITA ACADEMY GARISSA COUNTY 007 KENYA NATIONAL LIBRARY WAJIR COUNTY 008 RED CROSS HALL MANDERA COUNTY 009 MANDERA ARIDLANDS MARSABIT COUNTY 010 ST. STEPHENS TRAINING CENTRE ISIOLO COUNTY 011 CATHOLIC MISSION HALL, ISIOLO MERU COUNTY 012 MERU SCHOOL THARAKA-NITHI 013 CHIAKARIGA GIRLS HIGH SCHOOL EMBU COUNTY 014 KANGARU GIRLS HIGH SCHOOL KITUI COUNTY 015 MULTIPURPOSE HALL KITUI MACHAKOS COUNTY 016 MACHAKOS TEACHERS TRAINING COLLEGE MAKUENI COUNTY 017 WOTE TECHNICAL TRAINING INSTITUTE NYANDARUA COUNTY 018 ACK CHURCH HALL, OL KALAU TOWN NYERI COUNTY 019 NYERI PRIMARY SCHOOL KIRINYAGA COUNTY 020 ST.MICHAEL GIRLS BOARDING MURANGA COUNTY 021 MURANG'A UNIVERSITY COLLEGE KIAMBU COUNTY 022 KIAMBU INSTITUTE OF SCIENCE & TECHNOLOGY TURKANA COUNTY 023 LODWAR YOUTH POLYTECHNIC WEST POKOT COUNTY 024 MTELO HALL KAPENGURIA SAMBURU COUNTY 025 ALLAMANO HALL PASTORAL CENTRE, MARALAL TRANSZOIA COUNTY 026 KITALE MUSEUM UASIN GISHU 027 ELDORET POLYTECHNIC ELGEYO MARAKWET 028 IEBC CONSTITUENCY OFFICE - ITEN NANDI COUNTY 029 KAPSABET BOYS HIGH SCHOOL BARINGO COUNTY 030 KENYA SCHOOL OF GOVERNMENT, KABARNET LAIKIPIA COUNTY 031 NANYUKI HIGH SCHOOL NAKURU COUNTY 032 NAKURU HIGH SCHOOL NAROK COUNTY 033 MAASAI MARA UNIVERSITY KAJIADO COUNTY 034 MASAI TECHNICAL TRAINING INSTITUTE KERICHO COUNTY 035 KERICHO TEA SEC. SCHOOL -

Geology of the Kitale-Cherangani Hills Area
Report No. 35 CGLONY AND FROTECTDRATE 0F KENY‘. GEOLOGICAL SURVEY OF KENYA GEOLOGY GE THE KITALEnCHERANGANE BELLS AREA DEGREE SHEET 26. SLW. QUARTER (with colnured may) by J. M. MILLER, B.Sc._. F.G.S. Geologist 3950 EUHVHJD EH EH}: f,w’_"\‘F—_R\'.\ZE:I~QT PRET‘ITE'R. \MROBD ,“51‘1 5/, R G EOLOGY OF THE KITALE-CHERANGANI HILLS AREA DEGREE SHEET 26. S.W. QUARTER (with coloured map) .l. M. MILLER. 8.50.. I“.G.S. Geologist FOREWORD The report on the Kitale—Cherangani area extends to the east geological survey that was carried out in I949 in the Kitale, Elgon and West Suk areas, as described in Report No. 19 which was published in I952. The area south-west of Kitale. including the southern slopes of Mount Elgon. has also been described, in Report No. 26. published in 1954. Apart from superficial deposits the rocks of the area consist entirely of ancient gneisses and schists. Owing to the prominence of certain bands of quartzite, Mr. Miller has been able to work out a reasonably detailed picture of the structure of the rocks, concluding that they lie mainly in a series of overl'olds turned over to the west. He also demonstrates the effect of later tectonic events, an important point in the discussion of the relative ages of the Basement System of Kenya. which is believed to be of Archaean age. and the Pre-cambrian Kavirondian and Nyanzian rocks of western Kenya. The inference to be drawn from his work is that the Basement System rocks are. -

Regional Offices Geographical Areas Covered KEPHIS
KEPHIS REGIONAL OFFICES The operations of KEPHIS are organized in regional offices in Mombasa, Nakuru, Kitale, Embu, Kisumu and the headquarters. The geographical areas under the mandate of each Regional Office are as follows: Regional offices Geographical areas covered KEPHIS Headquarters Nairobi, Machakos, Makueni, Kitui, P.O. Box 49592-00100, Nairobi Tharaka Nithi, Kiambu, Thika, Cell: 0709 891 000 Maragwa, Nyambene, Muranga Tel: 020 661 8000 and Kajiado, Email: [email protected] , [email protected] Click here for Headquater's Location direction. Plant Quarantine Station P.O. Box 49421-00100 Nairobi PH: 020-3597204/5 Cell:0722-209505|0734-330017 VOIP-YELLO 7730592/3 Fax: 020-3536176 Email: [email protected] Plant Inspection Unit Jomo Kenyatta International Airport P.O. BOX 19164-00501 Nairobi. PHONE: 254-020-822768 Cell:0722-209504/0734-330016 TELFAX: 254-020-3597206/7 [email protected] Nakuru Regional Office Samburu, Nakuru, Laikipia, Baringo, P.O. Box 1679 Nakuru Kericho, Koibatek, Bomet, Narok, TELEFAX: 020-3536170 Transmara, Nyandarua, Kuria, Migori, Cell:0722-209503|0734-330020 Isibania, Nyamira, Homa Bay, Suba, Email: [email protected] Rachuonyo and Gucha Kitale Regional Office P.O. Box 249 Kitale PH: Trans Nzoia, West Pokot, Uasin Gishu, 254-054-30908| 020-3536173/3597211 Cell:0722- Bungoma, Mt. Elgon, Teso, Ungari, 209502|0734-330019 Fax: 254-054-31971 Butere, Vihiga, Nyando, Bondo, Siaya, [email protected] Turkana, Keiyo,Malaba, Suam, Marakwet and Nandi Mombasa Regional Office: Kwale, Kilifi, Mombasa, Taita Taveta, P.O. Box 80126 Mombasa Lamu, Tana River, Garissa, Wajir and PH: 2316002/3 |020-3536174/3587523 Mandera Cell:0722-209501|0734-330018 Fax: 254-041-316002 Email: [email protected] Kisumu Regional Office: Kisumu, Kakamega, Busia,Kuria, P.O. -

Factors That Influence Growth of Street Children Population in Kitale Town, Trans-Nzoia County-Kenya
FACTORS THAT INFLUENCE GROWTH OF STREET CHILDREN POPULATION IN KITALE TOWN, TRANS-NZOIA COUNTY-KENYA BY KHAOYA FLYINGSTONE EDWARD A RESEARCH PROJECT REPORT SUBMITTED IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE AWARD OF THE DEGREE OF MASTERS OF ARTS IN PROJECT PLANNING AND MANAGEMENT OF THE UNIVERSITY OF NAIROBI 2014 DECLARATION This project is my original work and has not been presented to any other university. Signature…………………………………………………Date……………… Khaoya Flyingstone Edward Reg.No. L50/62132/2013 This project has been submitted for review with my approval as university supervisor Signature…………………………………………………Date……………… Mr. Yona Sakaja. Lecturer Department of Extra Mural Studies University of Nairobi ii DEDICATION This project is dedicated to my dear wife Nancy , my daughters Brenda , Favor, Gift, Esther, and Treasure my mother Elizabeth Naliaka all my brothers and sisters who encouraged me to carry out this tedious but rewarding work. iii ACKNOWLEDGEMENT My thanks go to My Supervisor Mr. Sakaja for his tireless guidance throughout the writing of this project and very quick responses in addressing issues necessary for the successful completion of this work in good time.I also acknowledge the input of my lecturers especially Dr. Odundo and Mr. Ochieng all of the University of Nairobi for their role in introducing me to research methods during the first semester of my Study in the University of Nairobi which prepared me for this worthwhile project. My special tribute goes to Mr Julius Koringura the resident lecturer in Kitale Campus and Mr Patrick Simiyu, for their support during the entire period of my proposal writing especially in the provision of necessary help in the acquisition of necessary literature for the study. -

Pray for KENYA: 2020/5 December
P. O. BOX 57907 00200 NAIROBI TEL.+254728431067 [email protected] +254 205206573 Pray For KENYA: 2020/5 December Dear Brethren, We praise and glorify the Lord, that in spite of the frowning cloud of providence which Covid-19 has brought, He has been at work ensuring that the Gospel continues to speed ahead. At TBC Nairobi, we have known God’s grace from many different angles. In this update allow us to especially focus on the various prospects of establishing new churches in different towns of Kenya. These open doors for church planting/revitalization work are indeed a gracious answer by God to your prayers for us. It is only fitting that as we sing a song of praise and thanksgiving to God for answered prayers, we also invite you to join with us in exalting the Lord for His kindness. A lot of the existing mission work done by TBC is in the rural areas but now, we believe, the Lord has opened a door for urban ministry in five major towns. These towns are all headquarters of their counties. 1. Siaya Town This town is 425 km west of Nairobi and this is the home county of Eric Abwao (one of the Elders at TBCN). There has been a church in Siaya which was planted by us more than 20 years ago. This church has gone through various leadership difficulties. The founding pastor (now deceased) sadly proved unfaithful. The next pastor after some period was no longer resident. Brother Charles Abwok has only been able to come to Siaya on Sundays when he has preached during the service before travelling back to his home. -

THE OFFICIAL GAZETTE of the COLONY and PROTECTORATE of KENYA Pubhshed Under the Autbonty of Hm Egeeulency- the Governor -Of the Colony and Protectorate of Kenya - VOI
THE OFFICIAL GAZETTE OF THE COLONY AND PROTECTORATE OF KENYA Pubhshed under the Autbonty of Hm EgeeUlency- the Governor -of the Colony and Protectorate of Kenya - VOI. LIII-NO. 25 NAIROBI, May 15, 1 951 hoe 50 ants Reastered as a Newspaper at the G P 0 Pubhshed every Tuesday CONTENTS OFFlClAL GAZETl'E. OFFICIAL GAZETTE-Contd Govt Notlce No PAGE General Not~ceNo *542-Appo~ntment of V~ce-Pres~dentof Court of Wate~C ldlnance 1263 1278-1281, 1301 1302 Appeal 5 I0 Transpo t Llct nslng Board 1269 543-Appointments, etc 5 29 Tenders 1270,1271 544-Appllcatlon for Industrial Llcence 5 30 Momba a Notlces 1273- 1275 545-547-Justices of the Peace 5 30 E A W Lr Bonds Regstel 1276 548-The Forest Ordmance-Nouce 231 Compar ies Ord~nance 1282, 1290 549-Forest Boundary Comm~ss~on 5 32 Med~calPract~t~oner Registered 1287 550-The L~quorOrdinance-Appointment '32 Dlstnct Council Elect~ons 1288,1289, 1296 551-Asian C~vilServlce Adv~soryBoard-Appomt- Nat~ve lquor Llcens~ng 1295 ment ' 32 * Go~ernmentNotice No 542 was published as a Gazette 552-Rent Control Board-Appomtment 32 Extraor lina~yon 8th May 1951 55'3-The Traffic Ordinance-Appomtments '32 554-555-The Nat~veLands Trust Ord~nance-Land SUPPLEMEBT No 23 Set Apart 33 Proclamatzons Rules and Regulatzons I951 556-The Defence (Control of Pnces) Regulat~ons, 1945-Appo~ntments )33 Govt ? lohce No PAGE 557-The Municrpal~tlesOrd~nance-Appo~ntment 133 562 -The Customs Management Ordinance-Revoca- 558-The Legslat~ve Council Ordmance, 1935- tlon of Order 157 Appo~ntment r33 563 --The Samburu (G~azmgControl) (Amendment) 559-560-The Land Control Ordinance-Exempt~ons 34 Rules, 1951 157 561-Ob~tuary 34 56d -The Nakuru Munlclpal~tj(Meat) (Amendment) General Notices ,34- 40 By-laws, 1951 158 General No ILe No Loss of War Bond Certificates 1 '52 56' -The Rab~es(Fees) (Amtndment) Rules, 195 1 158 Probate and Adm~nlstration 1253, 1260, 1266-1268, 1283-1236 56f -The Nakuru Mun~clpal~ty (Conservancy) 1- '93.~ (Amendment). -

Environmental and Social Impact Assessment Study Report for the Proposed Eldoret-Kitale
ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT STUDY REPORT FOR THE PROPOSED ELDORET-KITALE 132KV TRAMISSION LINE JANUARY 2010 Submitted By: Otieno Odongo & Partners Consulting Engineers P.O Box 54021-00200 Nairobi Tel : 020-38700222 Fax : 020-3870103 Fax : 020-3870103 Email: [email protected] Submitted To: The Company Secretary The Kenya Power & Lighting Co. Ltd P.O Box 30099-00100 Nairobi, Kenya Tel : 020-3103366 1 EIA for proposed development 132kv Transmission Line Eldoret-Kitale January 2010 Document Authentication This report is prepared for: The Kenya Power & Lighting Company Limited P.O. Box 30099-00100 Nairobi Signed by: Position: Signature: Date: Otieno Odongo & Partners Consulting Engineers a registered firm of experts by the National Environment Management Authority, confirm that the contents of this report are a true representation of the Environmental and Social Impact Assessment of the proposed Eldoret-Kitale 132 kV Transmission Line Signed by the Environmental Expert: Signature: Date: 2 EIA for proposed development 132kv Transmission Line Eldoret-Kitale January 2010 EXECUTIVE SUMMARY Introduction The Government of Kenya plans to increase access to electricity in Kenya tenfold from the current 4% in the rural areas to about 40% by 2020. To achieve this, the transmission lines network are being considered for construction and upgrading which will have the communication system required for line protection and management purposes. The Kenya Power and Lighting Company Limited (KPLC) least cost power development plan identified various 132 KV developments for improving the performance of the national grid network to cater for the increasing load growth and meet the objectives of 2030. KPLC is planning to construct a new single circuit 132 kV transmission line between Eldoret – Kitale Power Transmission, comprising the following: • 132 kV line Eldoret – Kitale, 65 km The proposed line will serve the Kitale town and its surrounding environment.