Short- and Long-Latency Auditory Evoked Potentials in Individuals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Essays in Economics of Education
Essays in Economics of Education A DISSERTATION SUBMITTED TO THE FACULTY OF THE GRADUATE SCHOOL OF THE UNIVERSITY OF MINNESOTA BY Claudia Bueno Rocha Vidigal IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY Paul Glewwe, Adviser February 2019 © Claudia Bueno Rocha Vidigal 2019 ACKNOWLEDGEMENTS I would like to express my deepest gratitude to my advisor, professor Paul Glewwe, for his continuous support, guidance and encouragement. I had the great fortune to have worked with him and I am deeply indebted to his patient advice over the years. I am also grateful to my committee members, professors Deborah Levison, Joe Ritter, and Marc Bellemare, for their thoughtful comments and suggestions on my dissertation. I am also thankful for having had the opportunity to meet amazing colleagues and professors in my doctoral program. This long process would not have been possible without their support and friendship. I am profoundly grateful to my family, especially my parents, who have been a great source of support throughout my academic journey. Lastly, but most importantly, my husband and classmate, Vinicius Vidigal, deserves heartfelt thanks for his love, encouragement, and support. i DEDICATION To my mother, Katia Lucila Bueno, and my grandmother, Maria Angela Sotovia Bueno, whose love, encouragement and support made all this possible. ii ABSTRACT This dissertation consists of three essays in the economics of education. It investigates the effects of educational programs in primary and secondary schools in Brazil, as well as the effects of racial and low-income quotas in Brazilian universities. The first essay analyzes the impact of Brazil’s Multifunctional Resources Classroom Inclusion Program on the academic outcomes of disabled and non-disabled students in primary and secondary schools. -

Grammar for Academic Writing
GRAMMAR FOR ACADEMIC WRITING Tony Lynch and Kenneth Anderson (revised & updated by Anthony Elloway) © 2013 English Language Teaching Centre University of Edinburgh GRAMMAR FOR ACADEMIC WRITING Contents Unit 1 PACKAGING INFORMATION 1 Punctuation 1 Grammatical construction of the sentence 2 Types of clause 3 Grammar: rules and resources 4 Ways of packaging information in sentences 5 Linking markers 6 Relative clauses 8 Paragraphing 9 Extended Writing Task (Task 1.13 or 1.14) 11 Study Notes on Unit 12 Unit 2 INFORMATION SEQUENCE: Describing 16 Ordering the information 16 Describing a system 20 Describing procedures 21 A general procedure 22 Describing causal relationships 22 Extended Writing Task (Task 2.7 or 2.8 or 2.9 or 2.11) 24 Study Notes on Unit 25 Unit 3 INDIRECTNESS: Making requests 27 Written requests 28 Would 30 The language of requests 33 Expressing a problem 34 Extended Writing Task (Task 3.11 or 3.12) 35 Study Notes on Unit 36 Unit 4 THE FUTURE: Predicting and proposing 40 Verb forms 40 Will and Going to in speech and writing 43 Verbs of intention 44 Non-verb forms 45 Extended Writing Task (Task 4.10 or 4.11) 46 Study Notes on Unit 47 ii GRAMMAR FOR ACADEMIC WRITING Unit 5 THE PAST: Reporting 49 Past versus Present 50 Past versus Present Perfect 51 Past versus Past Perfect 54 Reported speech 56 Extended Writing Task (Task 5.11 or 5.12) 59 Study Notes on Unit 60 Unit 6 BEING CONCISE: Using nouns and adverbs 64 Packaging ideas: clauses and noun phrases 65 Compressing noun phrases 68 ‘Summarising’ nouns 71 Extended Writing Task (Task 6.13) 73 Study Notes on Unit 74 Unit 7 SPECULATING: Conditionals and modals 77 Drawing conclusions 77 Modal verbs 78 Would 79 Alternative conditionals 80 Speculating about the past 81 Would have 83 Making recommendations 84 Extended Writing Task (Task 7.13) 86 Study Notes on Unit 87 iii GRAMMAR FOR ACADEMIC WRITING Introduction Grammar for Academic Writing provides a selective overview of the key areas of English grammar that you need to master, in order to express yourself correctly and appropriately in academic writing. -

Performance of Students Admitted Through Affirmative Action in Brazil.Latin American Research Review
Valente, R R and Berry, B J L. Performance of Students Admitted through Affirmative Action in Brazil.Latin American Research Review. 2017; 52(1), pp. 18-34. DOI: https://doi.org/10.25222/larr.50 SOCIOLOGY Performance of Students Admitted through Affirmative Action in Brazil Rubia R. Valente and Brian J. L. Berry University of Texas at Dallas, US Corresponding author: Rubia R. Valente ([email protected]) Following the implementation of the Lei das Cotas (Affirmative Action Law) in Brazil, there has been debate as to whether students who were admitted through affirmative action perform at the same level as students admitted through traditional methods. This article examines the results of the Exame Nacional de Desempenho dos Estudantes (ENADE) from 2009 to 2012 to determine whether there is a relationship between students’ performance at the university level and the manner of their admittance. We find that students admitted to public universities under affirmative action perform at similar levels to students who were not, whereas quota students in private universities perform slightly better than students admitted through traditional methods. Com a implementação das Lei das Cotas no Brasil, tem se debatido se estudantes admitidos através de ação afirmativa demonstram o mesmo nível acadêmico dos estudantes admitidos através de métodos tradicionais. Este artigo analisa os resultados do Exame Nacional de Desempenho dos Estudantes (ENADE) durante o período de 2009 á 2012 para determinar se existe uma relação entre o desempenho dos alunos no âmbito universitário e as modalidades da sua admissão. Nossa análise revela que os estudantes que foram admitidos em universidades públicas através de ações afirmativas têm o mesmo desempenho acadêmico de estudantes que não se beneficiam de ações afirmativas, enquanto alunos cotistas em universidades privadas têm um desempenho ligeiramente melhor do que alunos admitidos através de métodos tradicionais. -

Practitioner's Guide to the Dizzy Patient
PRACTITIONER’S GUIDE TO THE DIZZY PATIENT Alan L. Desmond, AuD Wake Forest Baptist Health Otolaryngology ABOUT THE PRACTITIONER’S GUIDE TO THE DIZZY PATIENT The information in this guide has been reviewed for accuracy by specialists in Audiology, Otolaryngology, Neurology, Physical Therapy and Emergency Medicine ABOUT THE AUTHOR Alan L. Desmond, AuD, is the director of the Balance Disorders Program at Wake Forest Baptist Medical Center and a faculty member of Wake Forest School of Medicine. He is the author of Vestibular Function: Evaluation and Treatment (Thieme, 2004), and Vestibular Function: Clinical and Practice Management (Thieme, 2011). He is a co-author of Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo. He serves as a representative of the American Academy of Audiology at the American Medical Association and received the Academy Presidents Award in 2015 for contributions to the profession. He also serves on several advisory boards and has presented numerous articles and lectures related to vestibular disorders. HOW TO MAKE AN APPOINTMENT WITH THE WAKE FOREST BAPTIST HEALTH BALANCE DISORDERS TEAM Physician referrals can be made through the STAR line at 336-713-STAR (7827). PRACTITIONER’S GUIDE TO THE DIZZY PATIENT TABLE OF CONTENTS How to Use the Practitioner’s Guide to the Dizzy Patient . 2 Typical Complaints of Various Vestibular and non-Vestibular Disorders . 3 Structure and Function of the Vestibular System . 4 Categorizing the Dizzy Patient . 5 Timing and Triggers of Common Disorders . 6 Initial Examination Checklist for Acute Vertigo: Peripheral versus Central . 7 Diagnosing Acute Vertigo . 8 Fall Risk Questionnaire . 10 Physician’s Guide to Fall Risk Questionnaire . -

UNIVERSITY of CALIFORNIA Santa Barbara Assessing the Law Of
UNIVERSITY OF CALIFORNIA Santa Barbara Assessing the Law of Social Quotas: A qualitative approach to the perspectives of black University Students in São Paulo A Thesis Submitted in Partial Satisfaction of the Requirements for the Degree Master of Arts in Latin American and Iberian Studies by Alexander K. Scarlett Committee in charge: Professor Howard Winant, Chair Professor David Lopez-Carr Professor Emiko Saldivar September 2016 The thesis of Alexander K. Scarlett is approved. ____________________________________________ David Lopez-Carr ____________________________________________ Emiko Saldivar ____________________________________________ Howard Winant, Committee Chair September 2016 ABSTRACT Assessing the Law of Social Quotas: A qualitative approach to the perspectives of black university students in São Paulo Alexander K. Scarlett This paper provides some preliminary understandings of how well the Brazilian law of Social Quotas is working since it’s passing in 2012, focusing on student attitudes toward this law, their progress towards university degrees, and presumably middle-class status. By interviewing ten students (selected largely from the educational non-profit, Educafro) from various universities throughout the city of São Paulo, this essay peers into the lives of black students enrolled in affirmative action programs. In addition to public university students, I also include private university students who have received financial assistance (grants, loans, and scholarships) from programs to increase accessibility for underrepresented communities. I chose black university students as my primary informants as they are the population most equipped to comment on and detail the successes and failures of affirmative action policies. I confirmed my hypothesis that black students would generally provide positive responses to the Law of Social Quotas, as the majority of informants reflected positively of the legislations. -

P Homol Al Icfes Res 252 Abril 5 2018
Exámenes de Estado válidos para ingreso a la educación superior presentados en el exterior, resolución No. 000252 del 5 de abril de 2018. Examen Entidad País Sekretariat der Ständigen Konferenz der Kultusminister der Länder in der DEUTCHES ABITUR Alemania Bundesrepublik Deutschland - Kultusministerkonferenz KMK EXAMEN FACHHOCHSCHULREIFEPRÜFUNG CON PROFUNDIZACIÓN DE Instituto de Enseñanza Secundaria de Tecklenburggurger Land del Distrito de Alemania DEUTSCHES FACHABITUR Steinfut Ibbenbürn FESTSTELLUNGSPRÜFUNG Studienkolleg Múnich Alemania EXAMEN FINAL ENSEÑANZA SECUNDARIA CONTINUA GENERAL - HAVO Ministerio de Educación Nacional Aruba HIGHER SCHOOL CERTIFICATE RECORD OF ACHIEVEMENT Board of Stuoies Teaching & Educational Stanoards NSW Australia OVERALL POSITION (OP) Departamento de Educación de Queensland Australia EXAMEN DE ADMISIÓN NIVEL SUPERIOR Escuela Industrial " Pedro Domingo Murillo" Ministerio de Educación Bolivia EXAMEN ENEM Ministerio de Educación Brasil EXAMEN VESTIBULAR Ministerio de Educación y Cultura Brasil EXAMEN DE BACHILLERATO - VYSVEDCENIE O MATURITNEJ SKUSKE Ministerio de Educación, Ciencia, Investigación y Deporte Bratislava (República Eslovaca) STOP Universidad Libre de Burgas Bulgaria ALBERTA EDUCATION DIPLOMA EXAMS Government of Alberta Canadá GRADUATION PROGRAM British Columbia Ministry Education Canadá MEL Ministère de l`Education Canadá EXAMEN PSU Ministerio de Educación Chile PRUEBA DE APTITUD ACADÉMICA - PAA Ministerio de Educación del Gobierno de Chile y el DEMRE Chile EXAMEN UNIFICADO DE ADMISIÓN Oficina -

DOCUMENTO De TRABAJO DOCUMENTO DE TRABAJO
InstitutoINSTITUTO de Economía DE ECONOMÍA TRABAJO de DOCUMENTO DOCUMENTO DE TRABAJO 403 2011 Gender Differences in Major Choice and College Entrance Probabilities in Brazil Alejandra Traferri. www.economia.puc.cl • ISSN (edición impresa) 0716-7334 • ISSN (edición electrónica) 0717-7593 Versión impresa ISSN: 0716-7334 Versión electrónica ISSN: 0717-7593 PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE INSTITUTO DE ECONOMIA Oficina de Publicaciones Casilla 76, Correo 17, Santiago www.economia.puc.cl GENDER DIFFERENCES IN MAJOR CHOICE AND COLLEGE ENTRANCE PROBABILITIES IN BRAZIL Alejandra Traferri* Documento de Trabajo Nº 403 Santiago, Noviembre 2011 * [email protected] INDEX ABSTRACT 1 1. INTRODUCTION 2 2. MODEL AND ESTIMATION STRATEGY 5 2.1 Basic model 7 2.2 Model with correlations 9 2.3 Alternative models 12 3. THE UNIVERSITY ENTRANCE PROCESS 13 4. DATA AND DESCRIPTIVE STATISTICS 16 5. RESULTS OF THE ESTIMATIONS 21 5.1 Benchmark mode 21 5.2 Model with correlations 26 5.3 Gender differences in entrance probabilities and preferences 30 5.4. Interaction between gender and other explanatory variables 31 6. CONCLUSION 32 REFERENCES 34 APPENDIX 66 GENDER DIFFERENCES IN MAJOR CHOICE AND COLLEGE ENTRANCE PROBABILITIES IN BRAZIL∗ ALEJANDRA TRAFERRIy Abstract. I study gender differences in major choice and col- lege entrance probabilities in University of Campinas, a Brazilian public university dependent on the State of S~aoPaulo. As with most Brazilian public universities, students select a major, and then compete for a place in that major by taking a major-specific entrance exam. This singular characteristic of the Brazilian case allows me to differentiate the effect of gender on major-specific entrance probabilities and preferences. -

A Case Study in the City of Goiania
The cursinho industry and the advancement of the neoliberal agenda for access to education in Brazil: a case study in the city of Goiania by Sabrina Fernandes A thesis submitted to the Faculty of Graduate and Postdoctoral Affairs in partial fulfillment of the requirements for the degree of Master of Arts in Political Economy Carleton University Ottawa, Ontario ©2012, Sabrina Fernandes Library and Archives Bibliotheque et Canada Archives Canada Published Heritage Direction du 1+1 Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington Ottawa ON K1A0N4 Ottawa ON K1A 0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-93632-0 Our file Notre reference ISBN: 978-0-494-93632-0 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing Library and permettant a la Bibliotheque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par telecommunication ou par I'lnternet, preter, telecommunication or on the Internet, distribuer et vendre des theses partout dans le loan, distrbute and sell theses monde, a des fins commerciales ou autres, sur worldwide, for commercial or non support microforme, papier, electronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriete du droit d'auteur ownership and moral rights in this et des droits moraux qui protege cette these. Ni thesis. Neither the thesis nor la these ni des extraits substantiels de celle-ci substantial extracts from it may be ne doivent etre imprimes ou autrement printed or otherwise reproduced reproduits sans son autorisation. -

Vestibular Findings in Military Band Musicians
THIEME 122 Original Research Vestibular Findings in Military Band Musicians Bianca Simone Zeigelboim1 Crislaine Gueber2 Thanara Pruner da Silva3 Paulo Breno Noronha Liberalesso4 Claudia Giglio de Oliveira Gonçalves1 João Henrique Faryniuk2 Jair Mendes Marques1 Ari Leon Jurkiewicz1 1 Department of Speech-Language Pathology, Undergraduate Course Address for correspondence Bianca Simone Zeigelboim, PhD, and Communication Disorders Graduate Course at Universidade Department of Otoneurology, Universidade Tuiuti do Paraná–UTP, R. Tuiuti do Paraná—UTP, Curitiba, PR, Brazil Gutemberg, 99—9th floor, Curitiba, PR 80420-030, Brazil 2 Department of Speech-Language Pathology, UTP, Curitiba, Paraná, (e-mail: [email protected]). Brazil 3 Department of Surgery, Hospital das Clinicas, Universidade Federal do Paraná (UFPR), Curitiba, Paraná, Brazil 4 Pequeno Principe Hospital and the Digital EEG Laboratory at the Hospital da Cruz Vermelha, Curitiba, Paraná, Brazil Int Arch Otorhinolaryngol 2014;18:122–127. Abstract Introduction Exposure to music is the subject of many studies because it is related to an individual’s professional and social activities. Objectives Evaluate the vestibular behavior in military band musicians. Methods A retrospective cross-sectional study was performed. Nineteen musicians with ages ranging from 21 to 46 years were evaluated (average ¼ 33.7 years and standard deviation ¼ 7.2 years). They underwent anamnesis and vestibular and otolaryngologic evaluation through vectoelectronystagmography. Results The most evident otoneurologic symptoms in the anamnesis were tinnitus (84.2%), hearing difficulties (47.3%), dizziness (36.8%), headache (26.3%), intolerance to intense sounds (21.0%), and earache (15.7%). Seven musicians (37.0%) showed vestibular abnormality, which occurred in the caloric test. The abnormality was more prevalent in the peripheral vestibular system, and there was a predominance of irritative Keywords peripheral vestibular disorders. -
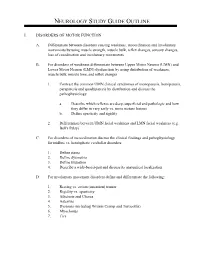
Neurology Study Guide Outline
NEUROLOGY STUDY GUIDE OUTLINE I. DISORDERS OF MOTOR FUNCTION A. Differentiate between disorders causing weakness, incoordination and involuntary movements by using muscle strength, muscle bulk, reflex changes, sensory changes, loss of coordination and involuntary movements B. For disorders of weakness differentiate between Upper Motor Neuron (UMN) and Lower Motor Neuron (LMN) dysfunction by using distribution of weakness, muscle bulk, muscle tone, and reflex changes 1. Contrast the common UMN clinical syndromes of monoparesis, hemiparesis, paraparesis and quadriparesis by distribution and discuss the pathophysiology a. Describe which reflexes are deep, superficial and pathologic and how they differ in very early vs. more mature lesions b. Define spasticity and rigidity 2. Differentiate between UMN facial weakness and LMN facial weakness (e.g. Bell's Palsy) C. For disorders of incoordination discuss the clinical findings and pathophysiology for midline vs. hemispheric cerebellar disorders 1. Define ataxia 2. Define dysmetria 3. Define titubation 4. Describe a wide-based-gait and discuss its anatomical localization D. For involuntary movement disorders define and differentiate the following: 1. Resting vs. action (intention) tremor 2. Rigidity vs. spasticity 3. Athetosis and Chorea 4. Asterixis 5. Dystonia (including Writers Cramp and Torticollis) 6. Myoclonus 7. Tics 8. Discuss the clinical findings, lab findings, and treatment of the following: a. Parkinson's Disease b. Essential Tremor c. Tardive Dyskinesia d. Huntington's Chorea e. Wilson's Disease II. DISORDERS OF SENSATION A. Differentiate central sensory disorders from peripheral sensory disorders by distribution, modalities affected, associated findings and the presence or absence of pain. B. For central sensory disorders describe the following and discuss the localization of each: 1. -

Gender, Genre, and Appropriation in Argentine and Brazilian Hard-Boiled Crime Fiction
Literatura Policial: Gender, Genre, and Appropriation in Argentine and Brazilian Hard-boiled Crime Fiction A DISSERTATION SUBMITTED TO THE FACULTY OF THE GRADUATE SCHOOL OF THE UNIVERSITY OF MINNESOTA BY Katherine Ann Ostrom IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY Fernando Arenas and Amy Kaminsky, advisers June 2011 © Katherine Ann Ostrom 2011 i Acknowledgements I am deeply indebted to my co-directors Amy Kaminsky and Fernando Arenas for their continuous support throughout my time as a graduate student at the University of Minnesota. This project grew out of a paper written for Professor Arenas in my first semester of graduate school, and I had been inspired by Professor Kaminsky’s scholarship even earlier. Through years of courses, meetings, exams, applications, and chapter drafts, they have offered helpful feedback and guidance while encouraging me to follow my passions and speak with my own voice. I am grateful as well to my committee members Ana Forcinito and Joanna O’Connell and to my other professors and mentors, especially Barbara Weissberger and Susan McMillan-Villar at the University of Minnesota and Patrick O’Connor, my undergraduate adviser at the University of Chicago, who have helped me discover the texts, authors, and ideas that would go into this dissertation. Among many fellow graduate students who have helped me, I am especially grateful to my friends Kajsa Larson, Adriana Gordillo, Kristin Beamish-Brown, Naomi Wood, Megan Corbin, Satty Flaherty-Echeverría, Scott Ehrenburg, Joseph Towle, and Rebecca Weaver for discussions and feedback on this project. The administrative staff and my students and other colleagues at the University of Minnesota Department of Spanish and Portuguese Studies and at Macalester College’s Department of Hispanic Studies have also provided much support and encouragement. -

Download Download
AISHE-J Volume 10, Number 1 (Spring 2018) 3501 New Audiences and New Educational Stratifications in Brazilian Higher Education in the 21st Century* Caregnato, C.E.† Raizer, L.† Grisa, G.‡ Miorando, B.S.† †Federal University of Rio Grande do Sul, Brazil ‡Federal Institute of Education, Science and Technology of Rio Grande do Sul, Brazil Abstract This article addresses the contradictions associated with the access of new audiences to higher education in Brazil in the last decade, aiming to describe and characterize the expansion of the system. Advances and limitations can be identified, as there are democratization movements and changes in patterns of persistent inequality. The discussion is based on studies about educational stratification, drawing on a Bourdieusian framework, and uses secondary statistical data on higher education and other Brazilian social indicators, collected by official agencies. The analysis indicates the increase in access to higher education in terms of income and ethnic group, allowing for a broader access to academic cultural capital and labour opportunities. However, it reinforces the argument that inequalities associated with educational stratification still remain in Brazil. The inclusion of these new audiences in Brazilian higher education is marked by categories of differentiation, such as the nature of institutions and funding of higher education, types of degree, teaching modality and shift. With that, despite the advances towards massification and retreat on vertical stratification, the forms of horizontal stratification in Brazilian higher education are increasing. Keywords: Higher education; educational stratification; new audiences; Brazil. *Article URL: http://ojs.aishe.org/index.php/aishe-j/article/view/[350] AISHE-J Volume 10, Number 1 (Spring 2018) Page 3502 1.