Medicare Claims Processing Manual (Chapter 12; Physician/Nonphysician Practitioners)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Icelandic Primary Care Physicians' Perceived
ICELANDIC PRIMARY CARE PHYSICIANS’ PERCEIVED COMPETENCE IN DETECTION AND TREATMENT OF BEHAVIOR DISORDERS Haukur Sigurðsson A Thesis Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of MASTER OF ARTS August 2007 Committee: William H. O’Brien, Advisor Robert A. Carels Michael J. Zickar © 2006 Haukur Sigurðsson All Rights Reserved iii ABSTRACT William H. O’Brien, Advisor While mental disorders are prevalent in primary health care settings, they often go undetected and untreated. There are no records to be found on studies of the effectiveness of Icelandic primary care physicians in diagnosing and treating mental illness. However, it is likely that the Icelandic primary health care system is not significantly different from systems in other countries that show poor detection and treatment of mental illness. The present study is the first study aimed at evaluating Icelandic primary care physicians’ experience with mental health problems and perceived competence in detection and treatment of behavior disorders. Furthermore, it is the first empirical attempt to assess the need for improved primary mental health care in Iceland. This exploratory study was designed to assess primary care physician’s perception of: 1) Prevalence and significance of different behavior disorders in the primary health care clinics, 2) their ability to detect and treat behavior disorders within the primary health care system, 3) the physician’s access to mental health services as well as quality of communication with mental health professionals, and 4) barriers to adequate mental health care within the Icelandic primary health care system. Main results suggest that Icelandic primary care physicians correctly identify that they, among all health care workers, are the ones seeing the highest proportion of people in the community suffering from mental health problems. -

Apple Education Professional Services. Turning Technology Into Educational Solutions
Apple Education Professional Services. Turning technology into educational solutions. Apple Education Professional Services is uniquely qualified to help your institution deliver on the promise of educational technology: more effective schools and higher student achievement. We’ve been committed to providing products that transform learning as well as professional services to education for more than 30 years. Today, our professional services experts are among the industry’s most experienced and respected. Drawing on our experience in education as well as industry certification training, our experts will help you leverage your technology investments to make an educational difference. Services tailored to your specific educational needs. Whether you’re in a K–12 school, at the district, or on a university campus, Apple Apple Integration Services Education Professional Services has a complete array of offerings to meet the diverse Add our experts to your staff. needs of education. Here are a few examples of what we can help you do: Apple Project Management • Plan and implement a full Apple 1 to 1 Learning Program The road to successful deployments. • Deploy wikis, blogs, or Podcast Producer • Create a new campuswide technology solution or integrate our technology with Apple Setup Services your existing systems Ready, set up, and go. • Mentor your technical staff so they get the most out of your specific Mac OS X Server installation and custom configuration Not only can we offer solutions for integrating iMac and MacBook into your curriculum, we’ll show you how iPod touch and iPad can transform learning, too. In other words, whatever your educational technology needs, we can help. -

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -

(Medicaid) Physician-Related Services/Health Care Professional
Washington Apple Health (Medicaid) Physician-Related Services/Health Care Professional Services Billing Guide May 1, 2020 Every effort has been made to ensure this guide’s accuracy. If an actual or apparent conflict between this document and an agency rule arises, the agency rules apply. Physician-Related Services/Health Care Professional Services About this guide* This publication takes effect May 1, 2020, and supersedes earlier guides to this program. The Health Care Authority (agency) is committed to providing equal access to our services. If you need an accommodation or require documents in another format, please call 1-800-562- 3022. People who have hearing or speech disabilities, please call 711 for relay services. Washington Apple Health means the public health insurance programs for eligible Washington residents. Washington Apple Health is the name used in Washington State for Medicaid, the children's health insurance program (CHIP), and state- only funded health care programs. Washington Apple Health is administered by the Washington State Health Care Authority. What has changed? Subject Change Reason for Change Entire document Housekeeping changes To improve usability Are clients enrolled in an Added a note box to identify the Billing clarification agency-contracted managed professional fees the agency pays care organization (MCO) for through fee-for-service eligible? Pre-operative visit before a Added language regarding the To improve clarity client receives a dental primary care physician’s role in service under anesthesia -

Mary Black Memorial Hospital
MEDICAL STAFF RULES & REGULATIONS Board of Directors: July 25, 2017 Table of Contents Page ARTICLE I Introduction 1.1 Definitions ..................................................................................................4 - 5 ARTICLE II Admission and Discharge 2.1 Admissions ................................................................................................ 6 - 7 2.2 Coverage and Call ..................................................................................... 7 - 9 2.3 Transfers ...................................................................................................... 10 2.4 Patients Who Are a Danger to Themselves or Others ................................. 10 2.5 Prompt Assessment ..................................................................................... 10 2.6 Discharge Orders and Instructions .............................................................. 11 2.7 Discharge Against Medical Advice ............................................................... 11 ARTICLE III Medical Records 3.1 Authentication of Entries ............................................................................. 11 3.2 Clarity, Legibility, and Completeness .................................................... 11 - 12 3.3 Abbreviations and Symbols ......................................................................... 12 3.4 Correction of Errors ..................................................................................... 12 3.5 History and Physical Examination ........................................................ -

CV-Summer 2017.Pdf
CURRICULUM VITAE NAME: MARY THERESE KILLACKEY, MD OFFICE ADDRESS: 1430 Tulane Avenue New Orleans, LA 70112 t 504.988.2317 f 504.988.1874 [email protected] PLACE OF BIRTH: Yonkers, NY EDUCATION: 1990-1994 Columbia College, Columbia University New York, NY, B.A. (Biology) 1994-1998 College of Physicians & Surgeons, Columbia University New York, NY M.D. POST-GRADUATE TRAINING: 6/1998-6/1999 Intern, General Surgery Strong Memorial Hospital University of Rochester Rochester, NY 6/1999-6/2003 Resident, General Surgery Strong Memorial Hospital University of Rochester Rochester, NY 7/2003-6/2005 Fellow, Abdominal Organ Transplant Surgery Recanati/Miller Transplant Institute The Mount Sinai Hospital New York, NY 11/2010 Leadership Development Program American Society of Transplant Surgeons Northwestern University Kellogg School of Management Chicago, IL 6/2015 Surgeons as Leaders Course American College of Surgeons Chicago, IL 9/2015-8/2016 Clinical Leadership Development Program Tulane School of Medicine, Office of the Dean New Orleans, LA 12/2015 Mid-Career Women Faculty Professional Development Seminar Association of American Medical Colleges Austin, TX 6/2016 Being a Resilient Leader Association of American Medical Colleges Washington, DC 6/2017 - 4/2018 Fellow, Executive Leadership in Academic Medicine Drexel University College of Medicine Philadelphia, PA ACADEMIC APPOINTMENTS: 7/2003-6/2005 Instructor in Surgery Mount Sinai School of Medicine New York, NY 10/2006-present Assistant Professor of Surgery and Pediatrics Tulane University -
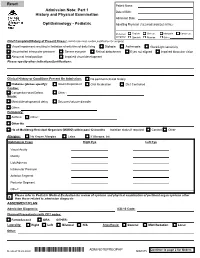
Adm Notepreophp
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

Everything You Need to Know About Professional Liability Insurance You Already Learned from Dr
THE ADVOCATE ✯ SUMMER 2016 55 EVERYTHING YOU NEED TO KNOW ABOUT PROFESSIONAL LIABILITY INSURANCE YOU ALREADY LEARNED FROM DR. SEUSS (AND OTHER CHILDREN’S STORIES) BY J. JAMES COOPER AND EMILY E. GARRISON VERY PROFESSIONAL FACES THE POTENTIAL for unfore- & officers policies often contain endorsements excluding seen claims from her clients. Even when those claims “professional services” from coverage. Thus, a threshold E are groundless, defending against them can be costly determination of what is, or is not, a “professional service” and time consuming. Professional liability insurance is an will have significant consequences for an insured. So it important risk management tool that may provide protection may not be surprising that, absent a precise definition of against many of the claims you face as a provider of profes- that term in the policy, insureds and insurers often disagree sional services, but it is also possible that your insurance about its meaning. policy may contain limiting or exclusionary language that eliminates or reduces the insurance coverage that you thought Texas courts have held that professional services “must you purchased. arise out of acts particular to the individual’s specialized vocation.”2 To constitute a professional service, then, “it Fortunately, understanding the ins and outs of professional must be necessary for the professional to use his special- liability policies, and learning how to avoid some of the ized knowledge or training.”3 This “legal” definition of common coverage pitfalls, is not as complicated as you may “professional services” may even control over contrary think. In fact, many of the lessons you learned in your policy language.4 favorite childhood stories serve to guide you down the yellow brick road of coverage. -

A Leader in the Oil & Gas Industry
KPMG GLOBAL ENERGY INSTITUTE A leader in the Oil & Gas industry kpmg.com/energy KPMG INTERNATIONAL 2 A leader in the Oil & Gas industry Sourcing the demand for energy. Keeping pace with change. Change is a constant factor in the Oil & Gas industry. The next few years may represent a tipping point, based on increased demand for energy, the growing presence of Asian markets and the gradual shift from traditional to alternative energy sources. Africa will be seen to play an ever more important role as a ready source of Oil & Gas for Western and Asian markets. Oil & Gas remains one of the world’s largest industries. In terms of value, Oil & Gas exports total more than 15 percent of global exports. Over 10 percent of the value of the world’s stock markets are invested in the energy sector, and eight of the top ten global FORTUNE companies are energy companies.1 Despite these impressive numbers, global energy demand will continue to exceed supply. Even with increased energy efficiency, world energy consumption is estimated to rise by 56 percent over the next three decades, with half of this increase driven by greater demand from China and India.2 Oil will remain the main source of energy while natural gas will overtake coal as the second-largest energy source.3 Alternative energy will continue to account for the highest growth rates in the global energy mix.4 1 KPMG research 2 International Energy Outlook 2013 3 Outlook for Energy: A View to 2040, ExxonMobil 4 Ibid. © 2014 KPMG International Cooperative (“KPMG International”). -

2013 Education Resolutions
2013 Agenda for the Reference Committee on Education National Conference of Special Constituencies—Sheraton Kansas City Hotel at Crown Center Item No. Resolution Title 1. Resolution No. 2001 Educate Adolescents on Consensual Sex (Don’t Rape) 2. Resolution No. 2002 Promotion of Forensic Sexual Assault & Child Abuse Examination Training 3. Resolution No. 2003 Enhancing the Training of Family Physicians in Addiction Medicine 4. Resolution No. 2004 Curriculum for End-of-Life Care 5. Resolution No. 2005 Education Resources for Non-Pharmacologic Approaches to Chronic Disease 6. Resolution No. 2006 Educational Resources for Environmental Influences on Health and Disease Processes 7. Resolution No. 2007 Resident Training in Reproductive Options 8. Resolution No. 2008 Breastfeeding Educations for Patients and Providers 9. Resolution No. 2009 Protected Time for Organized Medicine in Residency Education 10. Resolution No. 2010 Collaboration with Non-Physician Medical Providers 11. Resolution No. 2011 AAFP Advocates to American Board of Family Medicine on Behalf of Those Holding Certificates of Added Qualifications 12. Resolution No. 2012 Partnership and Promotion of Family Medicine to International Medical Graduate Residency Applicants 13. Resolution No. 2013 Education to Combat Gender Inequality for Family Medicine Physicians 4/26/2013 Page 1 of 1 Resolution No. 2001 2013 National Conference of Special Constituencies—Sheraton Kansas City Hotel at Crown Center 1 Educate Adolescents on Consensual Sex (Don’t Rape) 2 3 Submitted by: Cathleen London, MD, Women 4 Divya Reddy, MD, Women 5 Melodie Mope, MD, Women 6 Regina Kim, MD, Women 7 Barbara Walker, MD, Women 8 9 WHEREAS, Ninety-nine percent of people who rape are men, and 10 11 WHEREAS, 8% of men admit committing acts that meet the legal definition of rape or attempted 12 rape. -

General Surgery
- 1 - KALEIDA HEALTH Name: ___________________________________ Date: ____________________________ DELINEATION OF PRIVILEGES - GENERAL SURGERY PLEASE NOTE: Please check the box for each privilege requested. Do not use an arrow or line to make selections. We will return applications that ignore this directive. GENERAL STATEMENTS - Privileges in Adult Surgery are separated into the following divisions: General Surgery and Plastic Surgery. Applicants desiring procedure privileges in more than one division must complete separate forms for each. Procedures designated with an asterisk (*) indicate that Moderate or Deep Sedation may be required. If you do not have Moderate or Deep Sedation privileges, you must invite a Kaleida Health anesthesiologist to participate in the procedure. Procedures are also separated into levels of complexity (Level I-A, Level I-B, Level I, Level II, and Level III), which require increasing levels of education and experience. In general, procedures learned during residency are grouped in Level I-A or Level I and are granted upon evidence of successful completion of residency training. Level II procedures may or may not require evidence of additional training beyond residency. Documentation of additional training and/or experience is required for all Level III procedures. LEVEL I-A PRIVILEGES Procedures which involve primarily wound care, can be done under local anesthetic and occasionally involve application of temporary skin coverage or application of agents to expedite wound healing. Can be performed by any competent -

General Surgery Career Resource
The American Journal of Surgery (2013) 206, 719-723 Association of Women Surgeons: Career Development Resources General surgery career resource Ana M. Parsee, M.D.a, Sharona B. Ross, M.D.b, Nancy L. Gantt, M.D.c, Kandace Kichler, M.D.d, Celeste Hollands, M.D.e,* aJohns Hopkins Hospital, Baltimore, MD, USA; bFlorida Hospital, Tampa, FL, USA; cNortheast Ohio Medical University, St. Elizabeth Health Center, Rootstown, OH, USA; dUniversity of Miami, Palm Beach Regional Campus, Palm Beach, FL, USA; eSt John’s Children’s Hospital, Springfield, IL, USA KEYWORDS: Abstract General surgery residency training can lead to a rewarding career in general surgery and General surgery; serve as the foundation for careers in several surgical subspecialties. It offers broad-based training with General surgery exposure to the cognitive and technical aspects of several surgical specialties and prepares graduating residency; residents for a wide range of career paths. This career development resource discusses the training as- Surgical fellowship; pects of general surgery. Surgical subspecialties; Ó 2013 Elsevier Inc. All rights reserved. Transition to practice; Surgery interest groups General surgery training provides the foundation for who enter medical school with an interest in surgery and many different surgical career paths. The training begins those who become interested early can become involved with a general surgery residency, which is usually followed in their schools’ surgery interest group (SIGs) as early as by either entry into practice or additional training. General the first day of medical school at most institutions. Each surgery residency programs provide broad-based training local SIG has different offerings to help students explore with exposure to the cognitive and technical aspects of and develop their interest in surgery as a career.