Possible Endocannabinoid Control of Colorectal Cancer Growth
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

615 Neuroscience-Cayman-Bertin
Thomas G. Brock, Ph.D. Introduction to Neuroscience In our first Biology classes, we learned that lipids form the membranes around cells. For many students, interests quickly moved to the intracellular constituents ‘that really matter’, or to how cells or systems work in health and disease. If there was further thought about lipids, it might have been limited to more personal issues, like an expanding waistline. It was easy to forget about lipids in the complexities of, say, Alzheimer’s Disease, where tau protein is hyperphosphorylated by a host of kinases before forming neurofibrillary tangles and amyloid precursor protein is processed by assorted secretases, ultimately aggregating to form neurodegenerating plaques. What possible role could lipids have in all this? After all, lipids just form the membranes around cells. Fortunately, neuroscientists study complex systems. Whether working at the molecular, cellular, or organismal level, the research focus always returns to the intricately interconnected bigger picture. Perhaps surprisingly, lipids keep emerging as part of the bigger picture. At least, the smaller lipids do. Many of the smaller lipids, including the cannabinoids and eicosanoids, act as paracrine hormones, modulating cell functions in a receptor-mediated fashion. In this sense, they are rather like the peptide hormones in their diversity and actions. In the neurosystem, this means that these signaling lipids determine if synapses fire or not, when cells differentiate or die, and whether tissues remain healthy or become inflamed. Returning to the question posed above about lipids in Alzheimer’s, these mediators have roles at many levels in the course of the disease, as presented in an article on page 42 of this catalog. -

Cannabinoids and Endocannabinoid System Changes in Intestinal Inflammation and Colorectal Cancer
cancers Review Cannabinoids and Endocannabinoid System Changes in Intestinal Inflammation and Colorectal Cancer Viktoriia Cherkasova, Olga Kovalchuk * and Igor Kovalchuk * Department of Biological Sciences, University of Lethbridge, Lethbridge, AB T1K 7X8, Canada; [email protected] * Correspondence: [email protected] (O.K.); [email protected] (I.K.) Simple Summary: In recent years, multiple preclinical studies have shown that changes in endo- cannabinoid system signaling may have various effects on intestinal inflammation and colorectal cancer. However, not all tumors can respond to cannabinoid therapy in the same manner. Given that colorectal cancer is a heterogeneous disease with different genomic landscapes, experiments with cannabinoids should involve different molecular subtypes, emerging mutations, and various stages of the disease. We hope that this review can help researchers form a comprehensive understanding of cannabinoid interactions in colorectal cancer and intestinal bowel diseases. We believe that selecting a particular experimental model based on the disease’s genetic landscape is a crucial step in the drug discovery, which eventually may tremendously benefit patient’s treatment outcomes and bring us one step closer to individualized medicine. Abstract: Despite the multiple preventive measures and treatment options, colorectal cancer holds a significant place in the world’s disease and mortality rates. The development of novel therapy is in Citation: Cherkasova, V.; Kovalchuk, critical need, and based on recent experimental data, cannabinoids could become excellent candidates. O.; Kovalchuk, I. Cannabinoids and This review covered known experimental studies regarding the effects of cannabinoids on intestinal Endocannabinoid System Changes in inflammation and colorectal cancer. In our opinion, because colorectal cancer is a heterogeneous Intestinal Inflammation and disease with different genomic landscapes, the choice of cannabinoids for tumor prevention and Colorectal Cancer. -

N-Acyl-Dopamines: Novel Synthetic CB1 Cannabinoid-Receptor Ligands
Biochem. J. (2000) 351, 817–824 (Printed in Great Britain) 817 N-acyl-dopamines: novel synthetic CB1 cannabinoid-receptor ligands and inhibitors of anandamide inactivation with cannabimimetic activity in vitro and in vivo Tiziana BISOGNO*, Dominique MELCK*, Mikhail Yu. BOBROV†, Natalia M. GRETSKAYA†, Vladimir V. BEZUGLOV†, Luciano DE PETROCELLIS‡ and Vincenzo DI MARZO*1 *Istituto per la Chimica di Molecole di Interesse Biologico, C.N.R., Via Toiano 6, 80072 Arco Felice, Napoli, Italy, †Shemyakin-Ovchinnikov Institute of Bioorganic Chemistry, R. A. S., 16/10 Miklukho-Maklaya Str., 117871 Moscow GSP7, Russia, and ‡Istituto di Cibernetica, C.N.R., Via Toiano 6, 80072 Arco Felice, Napoli, Italy We reported previously that synthetic amides of polyunsaturated selectivity for the anandamide transporter over FAAH. AA-DA fatty acids with bioactive amines can result in substances that (0.1–10 µM) did not displace D1 and D2 dopamine-receptor interact with proteins of the endogenous cannabinoid system high-affinity ligands from rat brain membranes, thus suggesting (ECS). Here we synthesized a series of N-acyl-dopamines that this compound has little affinity for these receptors. AA-DA (NADAs) and studied their effects on the anandamide membrane was more potent and efficacious than anandamide as a CB" transporter, the anandamide amidohydrolase (fatty acid amide agonist, as assessed by measuring the stimulatory effect on intra- hydrolase, FAAH) and the two cannabinoid receptor subtypes, cellular Ca#+ mobilization in undifferentiated N18TG2 neuro- CB" and CB#. NADAs competitively inhibited FAAH from blastoma cells. This effect of AA-DA was counteracted by the l µ N18TG2 cells (IC&! 19–100 M), as well as the binding of the CB" antagonist SR141716A. -

2-Arachidonoylglycerol a Signaling Lipid with Manifold Actions in the Brain
Progress in Lipid Research 71 (2018) 1–17 Contents lists available at ScienceDirect Progress in Lipid Research journal homepage: www.elsevier.com/locate/plipres Review 2-Arachidonoylglycerol: A signaling lipid with manifold actions in the brain T ⁎ Marc P. Baggelaara,1, Mauro Maccarroneb,c,2, Mario van der Stelta, ,2 a Department of Molecular Physiology, Leiden Institute of Chemistry, Leiden University, Einsteinweg 55, 2333 CC Leiden, The Netherlands. b Department of Medicine, Campus Bio-Medico University of Rome, Via Alvaro del Portillo 21, 00128 Rome, Italy c European Centre for Brain Research/IRCCS Santa Lucia Foundation, via del Fosso del Fiorano 65, 00143 Rome, Italy ABSTRACT 2-Arachidonoylglycerol (2-AG) is a signaling lipid in the central nervous system that is a key regulator of neurotransmitter release. 2-AG is an endocannabinoid that activates the cannabinoid CB1 receptor. It is involved in a wide array of (patho)physiological functions, such as emotion, cognition, energy balance, pain sensation and neuroinflammation. In this review, we describe the biosynthetic and metabolic pathways of 2-AG and how chemical and genetic perturbation of these pathways has led to insight in the biological role of this signaling lipid. Finally, we discuss the potential therapeutic benefits of modulating 2-AG levels in the brain. 1. Introduction [24–26], locomotor activity [27,28], learning and memory [29,30], epileptogenesis [31], neuroprotection [32], pain sensation [33], mood 2-Arachidonoylglycerol (2-AG) is one of the most extensively stu- [34,35], stress and anxiety [36], addiction [37], and reward [38]. CB1 died monoacylglycerols. It acts as an important signal and as an in- receptor signaling is tightly regulated by biosynthetic and catabolic termediate in lipid metabolism [1,2]. -

A Dissertation Entitled Uncovering Cannabinoid Signaling in C. Elegans
A Dissertation Entitled Uncovering Cannabinoid Signaling in C. elegans: A New Platform to Study the Effects of Medicinal Cannabis By Mitchell Duane Oakes Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Doctor of Philosophy Degree in Biology ________________________________________ Dr. Richard Komuniecki, Committee Chair _______________________________________ Dr. Bruce Bamber, Committee Member ________________________________________ Dr. Patricia Komuniecki, Committee Member ________________________________________ Dr. Robert Steven, Committee Member ________________________________________ Dr. Ajith Karunarathne, Committee Member ________________________________________ Dr. Jianyang Du, Committee Member ________________________________________ Dr. Amanda Bryant-Friedrich, Dean College of Graduate Studies The University of Toledo August 2018 Copyright 2018, Mitchell Duane Oakes This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of Uncovering Cannabinoid Signaling in C. elegans: A New Platform to Study the Effects of Medical Cannabis By Mitchell Duane Oakes Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Doctor of Philosophy Degree in Biology The University of Toledo August 2018 Cannabis or marijuana, a popular recreational drug, alters sensory perception and exerts a range of medicinal benefits. The present study demonstrates that C. elegans exposed to -

Key Aspects to Consider About Beneficial and Harmful Effects on the Central Nervous System by the Endocannabinoid Modulation Linked to New Cardiovascular Therapies
Review Article Annals of Pharmacology and Pharmaceutics Published: 03 Dec, 2019 Key Aspects to Consider about Beneficial and Harmful Effects on the Central Nervous System by the Endocannabinoid Modulation Linked to New Cardiovascular Therapies Martin Gimenez VM1, Mocayar Maron FJ2, Kassuha DE1, Ferder L3 and Manucha W4,5* 1Research in Chemical Sciences, Catholic University of Cuyo, Argentina 2Department of Morphophysiology, National University of Cuyo, Argentina 3Department of Pediatrics, University of Miami, USA 4Department of Pathology, National Council of Scientific and Technological Research (IMBECU-CONICET), Argentina 5Department of Pathology, National University of Cuyo, Mendoza, Argentina Abstract The endocannabinoid system is closely related to the central nervous system and exerts a promising therapeutic potential on it and other systems such as the cardiovascular, mainly through its neuromodulatory, neuroprotective and neuroinflammatory effects. For this reason, when designing new treatments for different relevant pathologies such as hypertension, it is necessary to take into account the side effects that such therapies can cause at the neurological level. Deeping knowledge of each cannabinoid and the molecular mechanisms that can lead to undesired results is necessary. The OPEN ACCESS present review analyzes the psychoactive consequences of anandamide and other similar substances *Correspondence: such as other endocannabinoids, phytocannabinoids and synthetic cannabinoids, to assess their Walter Manucha, Department of little-explored -
DB Abs Cagliari Cong SIF 2007
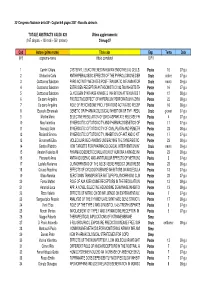
33° Congresso Nazionale della SIF - Cagliari 6-9 giugno 2007 - Raccolta abstracts TOTALE ABSTRACTS VALIDI: 828 Ultimo aggiornamento: (167 simposi + 100 orali + 561 posters) 24-mag-07 Cod Autore (primo nome) Titolo abs Esp. Tema Data (N°) cognome-nome (titolo completo) O/P/I 1 Carnini Chiara CYSTEINYL LEUKOTRIENES IN HUMAN ENDOTHELIAL CELLS: SYNTHPEoSstIeSr AND ACTIVI1T6IES 07-giu 2 Ghelardini Carla ANTIHYPERALGESIC EFFECTS OF THE PYRROLIDINONE DERIVATIVEO rNaIlKe-13317 IN MdoOloDrEeLS OF N0E7-UgRiuOPATHIC PAIN 3 Cuzzocrea Salvatore PARG ACTIVITY MEDIATES POST-TRAUMATIC INFLAMMATORY REACOTrIaOleN AFTER EXnPeuErRoIMENTA0L9 S-gPiuINAL CORD TRAUMA 4 Cuzzocrea Salvatore ESTROGEN RECEPTOR ANTAGONIST ICI 182,780 INHIBITS THE ANTPI-IoNsFteLrAMMATORY1 E6FFECT OF07 G-gLiUu COCORTICOIDS 5 Cuzzocrea Salvatore GLYCOGEN SYNTHASE KINASE-3 INHIBITION ATTENUATES THE DEPVoEsLtOerPMENT OF B1L2EOMYCIN0-8IN-gDiuUCED LUNG INJURY 6 De sarro Angelina PROTECTIVE EFFECT OF HYPERICUM PERFORATUM IN ZYMOSAN-IPNoDsUteCrED MULTIPL2E2 ORGAN D08Y-SgFiuUNCTION SYNDROME 7 De sarro Angelina ROLE OF PEROXISOME PROLIFERATORS ACTIVATED RECEPTORS PAoLPstHeAr (PPAR- ) IN1 6ACUTE PA0N8C-gRiuEATITIS INDUCED BY CERULEIN 8 Esposito Emanuela GENETIC OR PHARMACOLOGICAL INHIBITION OF TNF- REDUCED SPOLrAalNeCHNIC ISCgHioEvaMnIiA AND R07E-PgEiuRFUSION INJURY 9 Martire Maria SELECTIVE REGULATION OF [3H]D-ASPARTATE RELEASE FROM HIPPPoOsCteArMPAL NERV4E ENDINGS07 B-gYi uLARGE-CONDUCTANCE CA2+- AND VOLTAGE-ACTIVATED K+ (BK) CHANNELS 10 Mey Valentina SYNERGISTIC CYTOTOXICITY AND PHARMACOGENETICS -

SYNTHESIS of 3-HETEROCYCLE PHENYL N-ALKYL CARBAMATES and THEIR ACTIVITY AS FAAH INHIBITORS Doctoral Dissertation
TKK Dissertations 203 Espoo 2009 SYNTHESIS OF 3-HETEROCYCLE PHENYL N-ALKYL CARBAMATES AND THEIR ACTIVITY AS FAAH INHIBITORS Doctoral Dissertation Mikko Myllymäki Helsinki University of Technology Faculty of Chemistry and Materials Sciences Department of Chemistry TKK Dissertations 203 Espoo 2009 SYNTHESIS OF 3-HETEROCYCLE PHENYL N-ALKYL CARBAMATES AND THEIR ACTIVITY AS FAAH INHIBITORS Doctoral Dissertation Mikko Myllymäki Dissertation for the degree of Doctor of Philosophy to be presented with due permission of the Faculty of Chemistry and Materials Sciences for public examination and debate in Auditorium KE2 (Komppa Auditorium) at Helsinki University of Technology (Espoo, Finland) on the 19th of December, 2009, at 12 noon. Helsinki University of Technology Faculty of Chemistry and Materials Sciences Department of Chemistry Teknillinen korkeakoulu Kemian ja materiaalitieteiden tiedekunta Kemian laitos Distribution: Helsinki University of Technology Faculty of Chemistry and Materials Sciences Department of Chemistry P.O. Box 6100 (Kemistintie 1) FI - 02015 TKK FINLAND URL: http://chemistry.tkk.fi/ Tel. +358-9-470 22527 Fax +358-9-470 22538 E-mail: [email protected] © 2009 Mikko Myllymäki ISBN 978-952-248-240-2 ISBN 978-952-248-241-9 (PDF) ISSN 1795-2239 ISSN 1795-4584 (PDF) URL: http://lib.tkk.fi/Diss/2009/isbn9789522482419/ TKK-DISS-2686 Multiprint Oy Espoo 2009 3 AB HELSINKI UNIVERSITY OF TECHNOLOGY ABSTRACT OF DOCTORAL DISSERTATION P.O. BOX 1000, FI-02015 TKK http://www.tkk.fi Author Mikko Juhani Myllymäki Name of the dissertation -

N-Acyl Amino Acids (Elmiric Acids): Endogenous Signaling Molecules with Therapeutic Potential
Molecular Pharmacology Fast Forward. Published on November 14, 2017 as DOI: 10.1124/mol.117.110841 This article has not been copyedited and formatted. The final version may differ from this version. MOL #110841 1 MINIREVIEW N-Acyl amino acids (Elmiric Acids): endogenous signaling molecules with therapeutic potential Sumner H. Burstein Department of Biochemistry & Molecular Pharmacology, University of Massachusetts Medical School, Worcester, MA 01605 Downloaded from molpharm.aspetjournals.org at ASPET Journals on September 30, 2021 Molecular Pharmacology Fast Forward. Published on November 14, 2017 as DOI: 10.1124/mol.117.110841 This article has not been copyedited and formatted. The final version may differ from this version. MOL #110841 2 Running title. N-Acyl amino acids; endogenous signaling molecules Corresponding author: Sumner H. Burstein, Department of Biochemistry & Molecular Pharmacology, University of Massachusetts Medical School, Worcester, MA 01605 [email protected] Phone: 508-856-2850 FAX: 508-856-2251 Number of of text pages, 26 Number of tables, 3 Downloaded from Number of figures, 4 Number of references, 60 Number of words in the: molpharm.aspetjournals.org Abstract, 220 Introduction, 742 Discussion, 6338 Abbreviations: COX, cyclooxygenase; FAAH, fatty acid amide hydrolase; GABA, γ- at ASPET Journals on September 30, 2021 aminobutyric acid; GPCR, G-protein coupled receptor; LXA4, lipoxin A4 ; LOX, 12,14 lipoxygenases; PGJ,15-deoxy-Δ -prostaglandin-J2 Molecular Pharmacology Fast Forward. Published on November 14, 2017 as DOI: 10.1124/mol.117.110841 This article has not been copyedited and formatted. The final version may differ from this version. MOL #110841 3 Abstract The subject of N-acyl amino acid conjugates has been rapidly growing in recent years, especially with regard to their analgesic and anti-inflammatory actions. -

Roger G. Pertwee.Pdf
Handbook of Experimental Pharmacology Volume 168 Editor-in-Chief K. Starke, Freiburg i. Br. Editorial Board G.V.R. Born, London M. Eichelbaum, Stuttgart D. Ganten, Berlin F. Hofmann, München B. Kobilka, Stanford, CA W. Rosenthal, B erlin G. Rubanyi, Richmond, CA Cannabinoids Contributors M.E.Abood,S.Bátkai,T.Bisogno,G.A.Cabral,M.J.Christie, A.A. Coutts, S.N. Davies, R. de Miguel, L. De Petrocellis, V. Di Marzo, M. Egertová, M.R. Elphick, J. Fernández-Ruiz, S.J. Gatley, S.T. Glaser, M. Gómez, S. Gonzáles, M. Guzmán, C.J. Hillard, W.-S.V. Ho, A.G. Hohmann, A.C. Howlett, M.A. Huestis, A.A. Izzo, M. Karsak, G. Kunos, C. Li, A.H. Lichtman, K.P. Lindsey, M. Maccarrone, K. Mackie, A. Makriyannis, B.R. Martin, S.P. Nikas, P. Pacher, R.G. Pertwee, J.A. Ramos, P.H. Reggio, G. Riedel, P. Robson, E. Schlicker, A. Staab, B. Szabo, G.A. Thakur, O. Valverde, C.W. Vaughan, J.M. Walker, T. Wenger, A. Zimmer Editor Roger G. Pertwee 123 Professor Dr. Roger Pertwee School of Medical Sciences Institute of Medical Science University of Aberdeen Foresterhill Aberdeen AB25 2ZD Scotland, UK email: [email protected] With 84 Figures and 26 Tables ISSN 0171-2004 ISBN 3-540-22565-X Springer Berlin Heidelberg New York Library of Congress Control Number: 2004109756 This work is subject to copyright. All rights reserved, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broad- casting, reproduction on microfilm or in any other way, and storage in data banks. -

A Budding Source of Targets for Treating Inflammatory and Neuropathic Pain
Clinical and Translational Science Institute Centers 1-1-2018 The Endogenous Cannabinoid System: A Budding Source of Targets for Treating Inflammatory and Neuropathic Pain Giulia Donvito Virginia Commonwealth University Sara R. Nass West Virginia University Jenny L. Wilkerson Virginia Commonwealth University Zachary A. Curry Virginia Commonwealth University Lesley D. Schurman Virginia Commonwealth University See next page for additional authors Follow this and additional works at: https://researchrepository.wvu.edu/ctsi Part of the Medicine and Health Sciences Commons Digital Commons Citation Donvito, Giulia; Nass, Sara R.; Wilkerson, Jenny L.; Curry, Zachary A.; Schurman, Lesley D.; Kinsey, Steven G.; and Lichtman, Aron H., "The Endogenous Cannabinoid System: A Budding Source of Targets for Treating Inflammatory and Neuropathic Pain" (2018). Clinical and Translational Science Institute. 717. https://researchrepository.wvu.edu/ctsi/717 This Article is brought to you for free and open access by the Centers at The Research Repository @ WVU. It has been accepted for inclusion in Clinical and Translational Science Institute by an authorized administrator of The Research Repository @ WVU. For more information, please contact [email protected]. Authors Giulia Donvito, Sara R. Nass, Jenny L. Wilkerson, Zachary A. Curry, Lesley D. Schurman, Steven G. Kinsey, and Aron H. Lichtman This article is available at The Research Repository @ WVU: https://researchrepository.wvu.edu/ctsi/717 Neuropsychopharmacology REVIEWS (2018) 43, 52–79 © 2018 American -

The Endocannabinoid System As a Potential Therapeutic Target for Pain Modulation
Copyright © Trakya University Faculty of Medicine Invited Review | 115 Balkan Med J 2014;31:115-20 © 2014 The Endocannabinoid System as a Potential Therapeutic Target for Pain Modulation Ahmet Ulugöl Department of Medical Pharmacology, Trakya University Faculty of Medicine, Edirne, Turkey Although cannabis has been used for pain management for millennia, on multi-target analgesia compounds, where one of the targets is the very few approved cannabinoids are indicated for the treatment of pain endocannabinoid degrading enzyme. In this review, I provide an over- and other medical symptoms. Cannabinoid therapy re-gained attention view of the current understanding about the processes accounting for only after the discovery of endocannabinoids and fatty acid amide hy- the biosynthesis, transport and metabolism of endocannabinoids, and pharmacological approaches and potential therapeutic applications in drolase (FAAH) and monoacylglycerol lipase (MAGL), the enzymes this area, regarding the use of drugs elevating endocannabinoid levels playing a role in endocannabinoid metabolism. Nowadays, research in pain conditions. (Balkan Med J 2014;31:115-20). has focused on the inhibition of these degradative enzymes and the Key Words: 2-AG, anandamide, endocannabinoids, FAAH, MAGL, elevation of endocannabinoid tonus locally; special emphasis is given pain Cannabinoids are a group of chemical compounds that pro- CANNABINOID RECEPTORS AND THE SITE OF duce their effects via activating cannabinoid receptors; they ACTION OF CANNABINOIDS include the phytocannabinoids (herbal cannabinoids/natural cannabinoids found in the cannabis plant), synthetic cannabi- To date, two subtypes of cannabinoid receptors, termed noids, and endogenous cannabinoids (endocannabinoids) (1, 2). cannabinoid-1 (CB1) and cannabinoid-2 (CB2) receptors, Cannabis, also known as marijuana, has been used as both a have been cloned (10, 11).