Luton & Dunstable University Hospital Annual Report and Accounts 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chalgrave News
CHALGRAVE NEWS The free community magazine delivered to homes and businesses in the Chalgrave Parish Publication No. 45 December 2014 1 Dates for Your Diary Day/Date Event Location/Contact Time 3rd Tuesday of each month Parish Council Meeting Memorial Hall 7.30pm Every other Sunday Quiz Night Plough Inn 8.00pm Mondays Dominoes Plough Inn Mondays & Fridays Live entertainment Queen’s Head 7.30pm Wednesdays Darts Queen’s Head Thursdays Dominoes Queen’s Head Weekdays Book Club Noeleen Thompson 2nd Tuesday of each month WI Memorial Hall 8–10pm th Senior Citizens’ Christmas Saturday 6 December Parkfields School Lunch th Toddington Village Sunday 7 December Christmas Concert 3pm Hall st Starting from From about Sunday, 21 December Santa Run Wingfield 5.30–6pm Front Cover: Fireworks at the Queen’s Head Deadline for next edition: Monday, 16 February 2015 Please submit entries by email to: [email protected] Or by phone to: Roger Parker on 01525 874910 The Chalgrave News team produce The Chalgrave News in good faith and do all we can to ensure that no offence is caused to any individual or organisation. We also reserve the right not to publish articles and contributions submitted to us if they do not comply with our policy. 2 Editorial Hello again! Back in September, JP, one of our regular contributors, tactfully suggested that it was time that the Chalgrave News entered the twenty-first century and got itself a Facebook page. In response, it was politely pointed out to JP that Facebook only started in 2004 and it’s generally considered wise to give these innovations time to settle down and for the bugs to be ironed out. -

Street Lighting Replacement 5 Year Programme
APPENDIX I - STREET LIGHTING REPLACEMENT 5 YEAR PROGRAMME Street Lighting Programme for 2014/15 Number Road of Ward Cost (£) columns Chequer Street 6 South 11,700 Crawley, High Town, Crawley Green Road 75 Round Green, South & 138,200 Wigmore Dallow Road 14 South 30,800 Grange Avenue 15 Leagrave 32,200 Gipsy Lane 13 South 33,800 Hatters Way 66 Dallow 167,500 Hitchin Road 28 56,000 Mayne Avenue 19 Leagrave 32,000 Midland Road 14 High Town 26,000 Northwell Drive (including roundabouts and new 57 Northwell 111,150 scheme at Lea Manor High School) Ravenhill Way 45 Lewsey 75,500 Skimpot Road 17 Challney 36,500 Station Road, Leagrave 2 Leagrave and Limbury 3,350 Wauluds Bank Drive 1 Northwell 1,950 372 Total Cost 756,650 Street Lighting Programme for 2015/16 Number Road of Ward Cost (£) columns Barton Road 70 Icknield & Bramingham 150,150 Sundon Park, Limbury & Bramingham Road 61 134,200 Northwell Burr Street 7 High Town 11,725 Coverdale 21 Leagrave 31,500 New Bedford Road 67 Barnfield & Icknield 143,750 High Town, Barnfield & Old Bedford Road 137 252,500 Icknield Wauluds Bank Drive RA 3 Northwell & Sundon Park 6,450 366 Total Cost 730,275 Street Lighting Programme for 2016/17 Number Road of Ward Cost (£) columns Abigale Close 7 Biscot 10,500 Addington Way LC 1 - 13 13 Challney 23,400 Back Street 8 High Town 12,000 Bampton Road 9 Challney 13,500 Barford Rise 6 Wigmore 9,000 Beech Road 6 Dallow 9,000 Beechwood Road 170 to Tenby Drive 60 2 Challney 3,000 Bellerby Rise 12 Leagrave 18,000 Belvedere Road 1 Limbury 1,500 9/42 Berrow Close 4 Wigmore -
Dunstable Bus Timetable
Pulloxhill Pulloxhill ◆ 79.89 162 Woburn Eversholt X31 .42 ◆ Holwell 77◆.197◆ 20 Higham 100 Woburn 138◆ 138◆ Apsley 150 20◆ Gobion 162 Abbey Eversholt 140◆ Westoning End 150◆ 139◆ 77◆ W14◆ 89 6 X31 138◆ 0 M1 4 140◆ 138◆ 2 Westoning 79 89 Dunstable Bus Timetable 1 Little 140◆ 5 Flitwick & Harlington W10◆ Brickhill 10 A F7◆ W12◆ 162 ◆ Tingrith PLUSBUS Zone Ickleford A 160◆ 138◆ 138 Barton-le-Clay Pirton 82 5 ◆ 20◆.X31◆ Windsor Parade 162 165◆ A 139 89 M2 4 M ◆ ◆ 79 A ◆ 0 Milton 140◆ 20◆ 42.77 .138 74◆ E7 1 1 74◆ 6 2 197◆ 0 th Bryan 42 Harlington 0 28 March 2011 www.centralbedfordshire.gov.uk 197◆ 20◆ Barton-le-Clay ◆ ton 8 X31 W14 gh u Sharpenhoe Hexton O Great B655 Pegsdon Flying Fox Harlington S1 Hitchin 82 Brickhill 20.X31◆ Sharpenhoe B65 5 Bancroft a 140◆ 20 79 77◆ 89◆ l M1 42.77◆.138◆ Clappers King’s Wood Junction 12 74◆ Barton M1.M2.E7◆ Hills 77◆ 77◆.82.89 This booklet also covers Houghton Regis, Eaton Bray, mond Stockgrove 165◆ 160◆ Hitchin Country Park 150 Sundon Hills S1.20◆ Caddington, Whipsnade and surrounding villages 162 20.X31◆ Country Park A Toddington Streatley 74◆.79 X31 4 42.77◆ 20◆ W14◆ ◆ 0 10 77 77◆ A 1 ◆ Toddington 138◆.140◆ Heath and 5 Battlesden 2 139 W10◆ 5 Reach X31.42.77◆ 50 W14◆ M Upper 79 A 77◆ ◆ ◆ ◆ 1 165 138 .140 Sundon 70 27 160◆ 74◆ 162 A 150 S1 6 27 42◆ 20 20 20◆ 100 Leighton Buzzard 27 Tebworth X31 A 74◆ Lower 79 PLUSBUS Zone 5 B Gosmore Hockliffe 1 57 Sundon X31 2 9 0 Lilley 2 139◆ Leighton Chalton 20 Great 69◆ Offley Buzzard 10 10◆ ◆ 69◆ Wingfield 05 139 Luton A5 X31 X31 74◆ PLUSBUS Zone A ◆ 5 42 X31 -

Premier Division Entry Requirements
SPORTSFORM Head Office Units 1 & 6 Fenlake Road Ind. Estate, Fenlake Road, Bedford MK42 0HB Tel; 01234 210005 Fax; 01234 229000 www.sportsform.co.uk Supporting the BEDFORDSHIRE COUNTY FOOTBALL LEAGUE Page 2 [Revision 2: 9th October 2015] Page 3 [Revision 2: 9th October 2015] BEDFORDSHIRE COUNTY FOOTBALL LEAGUE FOUNDED 1904 – RENAMED 2009 SEASON 2015-2016 FIXTURES, RESULTS, TABLES and NEWS www.bedfordshirefootballleague.co.uk http://full-time.thefa.com/Index.do?league=7195521 FRONT COVER PICTURE: Caldecote v Renhold United Bedfordshire County Football League Premier Division 1st November 2014 REVISION 1 dated 11th September 2015. Initial release. Major changes for this season highlighted in red in margin. REVISION 2 dated 9th October 2015. Alterations are shown highlighted in purple in margin. Page 4 [Revision 2: 9th October 2015] CONTENTS SPORTSFORM BEDFORD Page 2 BEDFORDSHIRE COUNTY FOOTBALL LEAGUE SUPPORTER WESTS CITROËN BEDFORD Page 3 BEDFORDSHIRE COUNTY FOOTBALL LEAGUE SUPPORTER FORMATION OF DIVISIONS Page 6 LEAGUE OFFICERS Page 7 RULES OF THE LEAGUE: FOR THE GUIDANCE OF CLUB SECRETARIES Page 8 HOW TO DECIDE ON THE MARK FOR THE REFEREE Page 12 FULL RULES OF THE LEAGUE Page 13 RULES FOR KNOCK-OUT COMPETITIONS Page 28 DIRECTORY OF CLUBS Page 30 REFEREES Page 38 FINAL TABLES 2013-2014 Page 40 MANAGEMENT COMMITTEE MEETING DATES Page 41 DATE FOR ANNUAL GENERAL MEETING 2016 Page 41 HONOURS BOARD 2014-2015 Page 41 PREMIER DIVISION SEASON 2015-2016 Page 42 LEAGUE RECORDS Page 43 REGULATIONS FOR THE OPERATION OF THE N.L.S. Page 48 Page 5 [Revision -

Existing Leisure Facilities in and Around Dacorum Borough Council
Existing Leisure Facilities in and around Dacorum Borough Council Table 6.1 Leisure Centres in and around Dacorum Area Name Address Postcode Hertfordshire Moat House, London Road, Markyate Club Motivation Markyate AL3 8HH Hemel Jarman Centre, Old Crabtree Lane, Hemel Hempstead Leisureworld Hempstead, Hertfordshire HP2 4JW Hemel Hempstead Sports Centre Park Road, Hemel Hempstead, Hertfordshire HP1 1JS Esporta Orchard Fields, Hemel Hempstead HP2 7DF Longdean Sports CentRumballs Road, Bennetts End HP3 8JB Shendish Manor Health Club London Road, Apsley HP3 0AA Marlowes Fitness Centre The Marlowes Centre, Hemel Hempstead HP1 1DX Spirit Health and Holiday Inn, Breakspear Way, Hemel Fitnesss Hempstead HP2 4UA Berkhamsted Sports Lagley Meadow, Douglas Gardens, Berkhamsted Centre Berkhamsted, Hertfordshire, HP4 3QQ 172-176, High Street, Berkhamsted, Fitness First Hertfordshire HP4 3AP Tring Tring Sports Centre Mortimer Hill, Tring, Hertfordshire HP23 5JU Champneys Health Resort Champneys, Wigginton, Tring, Hertfordshire HP23 6HY Harveys 58-59 High Street, Tring HP23 5AG Exclusively Ladies 68 - 70 Mortimer Hill, Tring HP23 5EE Other The Chiltern Pools Chiltern Avenue, Amersham, Buckinghamshire HP6 5AH The Riviera Suite Ski Centre Lakeside, Aylesbury, Buckinghamshire, HP19 0FX Hartwell House, Oxford Road, Stone, Aylesbury, The Hartwell Spa Buckinghamshire HP17 8NL Body Flex Gym 113, Cambridge St, Aylesbury, Buckinghamshire HP20 1BT Reflexions Health and Leisure Watermead, Aylesbury, Buckinghamshire HP19 0FY Curves 61-63 High Street, Aylesbury, Buckinghamshire -
Review Report Template
OVERVIEW AND SCRUTINY COMMITTEE THURSDAY 11 JUNE 2009 7.30 PM COMMITTEE AGENDA COMMITTEE ROOMS 1& 2 HARROW CIVIC CENTRE MEMBERSHIP (Quorum 4) Chairman: Councillor Stanley Sheinwald Councillors: Mrs Vina Mithani Mrs Margaret Davine Christopher Noyce Janet Mote B E Gate Anthony Seymour Mitzi Green (VC) Dinesh Solanki Jerry Miles Yogesh Teli Mrs Rekha Shah Mark Versallion Representatives of Voluntary Aided Sector: Mrs J Rammelt/Reverend P Reece Representatives of Parent Governors: Mrs Despo Speel/Mr Ramji Chauhan (Note: Where there is a matter relating to the Council’s education functions, the “church” and parent governor representatives have attendance, speaking and voting rights. They are entitled to speak but not vote on any other matter.) Reserve Members: 1. John Cowan 1. Krishna James 1. Paul Scott 2. Mrs Camilla Bath 2. Phillip O'Dell 3. Ashok Kulkarni 3. Ms Nana Asante 4. Manji Kara 4. Asad Omar 5. Narinder Singh Mudhar 5. Graham Henson 6. Don Billson 7. G Chowdhury Issued by the Democratic Services Section, Legal and Governance Services Department Contact: Daksha Ghelani, Senior Democratic Services Officer Tel: 020 8424 1881 E-mail: [email protected] HARROW COUNCIL OVERVIEW AND SCRUTINY COMMITTEE MOVED FROM 9 JUNE 2009 THURSDAY 11 JUNE 2009 AGENDA - PART I 1. Attendance by Reserve Members: To note the attendance at this meeting of any duly appointed Reserve Members. Reserve Members may attend meetings:- (i) to take the place of an ordinary Member for whom they are a reserve; (ii) where the ordinary Member will be absent for the whole of the meeting; and (iii) the meeting notes at the start of the meeting at the item ‘Reserves’ that the Reserve Member is or will be attending as a reserve; (iv) if a Reserve Member whose intention to attend has been noted arrives after the commencement of the meeting, then that Reserve Member can only act as a Member from the start of the next item of business on the agenda after his/her arrival. -

LTFC Issue 4
LTFC COMMUNITY TRUST NEWSLETTER | ISSUE 4 | MAY 2017 Leisure & Culture Award 2016 SPORT | EDUCATION | HEALTH | INCLUSION COMMUNITYTRUST Cohesion Sports Champions 2017 Registered Charity | Charity No. 1123078 GOLDEN OLDIES SPECIAL! MAN V FAT SUCCESS walking football regional win Our rst Man V Fat league 1 has just nished and The Luton Town Men’s Over 50’s Walking Football team been declared a huge success by our partners recently won the Regional Cup at Venue 360 in the EFL LiveWell Luton as they announced the total weight Walking Football national competition. loss by over 60 participants was a massive 227 kg The victory means the team set up by the Hatter’s Commu- – that’s like losing a couple of full backs! nity Trust are now through to the nals of the competition, On the pitch, it was a closely fought battle where they will ght it out for the title at Sky Bet Champion- between two teams for the league title, however ship club Aston Villa’s training ground-Bodymoor Heath. Exeter Gently came out on top, winning the league by 4 points after 14 games. It highlights a fantastic year for the group, who have also won the Beds County Cup, Advanced and intermediary Our rst season has been such a success that we are Cups and the Cedars Cup. That added to the fact that they starting Season 2 of our Man v Fat League straight were runners-up in the regionals to Bedford in the People’s away at Lea Manor Recreation Centre every Monday Cup, shows just how far the group have come in the 2 at 7.30 pm starting from 5th June. -

Ref Recorded Date Committed from Committed to Code Offence Street Area Beat/Ward Beat 40/1582/20 09/01/2020 09/01/2020 04:20
Ref Recorded Date Committed From Committed To Code Offence Street Area Beat/Ward Beat 40/1582/20 09/01/2020 09/01/2020 04:20 09/01/2020 04:30 29A Aggravated Burglary - Residential - Dwelling Liston Close Luton Leagrave 321 321 40/5742/20 28/01/2020 28/01/2020 00:00 105A Assault without Injury - Common assault and battery Acworth Crescent Luton Leagrave 321 321 40/5492/20 27/01/2020 01/09/2019 00:00 27/01/2020 00:00 105A Assault without Injury - Common assault and battery Brickly Road Luton Leagrave 321 321 40/4750/20 23/01/2020 23/01/2020 18:10 23/01/2020 18:36 105A Assault without Injury - Common assault and battery Home Court, Home Close Luton Leagrave 321 321 40/2207/20 12/01/2020 28/10/2019 00:00 28/10/2019 00:00 105A Assault without Injury - Common assault and battery Gilderdale Luton Leagrave 321 321 40/2186/20 12/01/2020 22/12/2019 00:00 22/12/2019 00:00 105A Assault without Injury - Common assault and battery Gilderdale Luton Leagrave 321 321 40/3192/20 16/01/2020 16/01/2020 00:00 104 Assault without injury on a constable (Police Act offence) Hockwell Ring Luton Leagrave 321 321 40/5184/20 25/01/2020 25/01/2020 16:00 25/01/2020 20:00 28E Burglary - Residential - Dwelling High Street Luton Leagrave 321 321 40/3593/20 18/01/2020 06/05/2017 06:45 06/05/2017 07:00 28E Burglary - Residential - Dwelling Brickly Road Luton Leagrave 321 321 40/3591/20 18/01/2020 04/05/2012 16:45 04/05/2012 21:20 28E Burglary - Residential - Dwelling Toddington Road Luton Leagrave 321 321 40/3590/20 18/01/2020 05/05/2017 23:30 06/05/2017 06:30 28E Burglary -
Luton & Dunstable University Hospital Annual Report and Accounts2011
Luton & Dunstable University Hospital NHS Foundation Trust NHS Foundation Hospital University & Dunstable Luton AnnualReport&Accounts2015-2016 Incorporating Quality Account Quality Incorporating Annual Report and Accounts AnnualReport &Accountsfor the period April 2015 to March 2016 2010-2011incorporating Quality Account Luton & Dunstable University Hospital NHS Foundation Trust Lewsey Road Luton LU4 0DZ Incorporating Quality Report Telephone 01582 49 11 66 Luton and Dunstable University Hospital www.ldh.nhs.uk NHS Foundation Trust Luton and Dunstable University Hospital NHS Foundation Trust Annual Report & Accounts for the period April 2015 to March 2016 incorporating Quality Account Presented to Parliament pursuant to Schedule 7, paragraph 25 (4) (a) of the National Health Service Act 2006 © 2016 Luton and Dunstable University Hospital NHS Foundation Trust Contents INTRODUCTION 3 FINANCIALPERFORMANCEREPORT 89 Awards and Congratulations 4 Review of Financial Performance 90 Introduction 8 Remuneration report 93 About this Report 9 Fundraising and Charitable Donations 94 Chairman’s Statement 10 ANNUALGOVERNANCESTATEMENTAND STRATEGY 13 ACCOUNTS 99 Strategic Vision 14 Statement of the Chief Executive’s Responsibilities 100 Performance against Corporate Objectives 2015/16 16 Annual Governance Statement 2015/16 101 Service Developments delivered in 2015/16 21 Independent Audit Opinion 109 2016/17 Strategic Approach 25 Foreword to the Accounts 113 Maintaining Performance 27 Statement of comprehensive income 114 Corporate Objectives 2016/17 28 Statement of financial position 115 Improving Quality 29 Statement of changes in equity 116 Service Developments planned for 2016/17 31 Statement of cash flows 117 Notes to the accounts 118 OPERATIONALPERFORMANCEREPORT 35 Principal activities of the Trust 36 APPENDIX1QUALITYACCOUNT 155 Review of Operational Performance 38 What is a Quality Account? 156 Quality 40 About Our Trust 157 Regulatory Performance Ratings 41 1. -
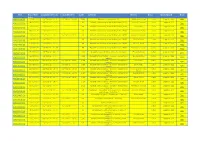
Ref Recorded Date Committed from Committed to Code
Ref Recorded Committed From Committed To Code Offence Street Area Beat/Ward Beat Date 40/23914/20 01/05/2020 01/05/2020 22:30 01/05/2020 22:45 56B Arson not endangering life Toddington Road Luton Leagrave 321 321 09/05/2020 09/05/2020 01:55 8N Assault occasioning actual bodily harm (ABH) Acworth Crescent Luton Leagrave 321 40/25155/20 321 03/05/2020 03/05/2020 00:00 8N Assault occasioning actual bodily harm (ABH) Coverdale Luton Leagrave 321 40/24231/20 321 19/05/2020 19/05/2020 10:30 8N Assault occasioning actual bodily harm (ABH) Acworth Crescent Luton Leagrave 321 40/26984/20 321 15/05/2020 15/05/2020 16:00 15/05/2020 16:30 8N Assault occasioning actual bodily harm (ABH) Acworth Crescent Luton Leagrave 321 40/26290/20 321 09/05/2020 09/05/2020 00:00 8N Assault occasioning actual bodily harm (ABH) Butely Road Luton Leagrave 321 40/25290/20 321 21/05/2020 21/05/2020 10:00 8N Assault occasioning actual bodily harm (ABH) Vincent Road Luton Leagrave 321 40/27434/20 321 03/05/2020 03/05/2020 20:25 8N Assault occasioning actual bodily harm (ABH) Acworth Crescent Luton Leagrave 321 40/24226/20 321 17/05/2020 17/05/2020 22:03 104 Assault or assault by beating of a constable Finsbury Road Luton Leagrave 321 40/26715/20 321 04/05/2020 04/05/2020 00:00 105A Assault without Injury - Common assault and Hockwell Ring Luton Leagrave 321 40/24392/20 battery 321 29/04/2020 28/04/2020 19:30 28/04/2020 19:50 105A Assault without Injury - Common assault and Coverdale Luton Leagrave 321 40/23470/20 battery 321 19/05/2020 19/05/2020 00:00 19/05/2020 00:00 -

Luton & Dunstable Hospital Annual Report and Accounts 2019-2020
Luton & Dunstable University Hospital NHS Foundation Trust NHS Foundation Hospital University & Dunstable Luton Luton and Dunstable University Hospital NHS Foundation Trust Annual Report & Accounts 2019-2020 2019-2020 & Accounts Annual Report Annual Report & Accounts 2010-2011 Luton & Dunstable University Hospital Annual Report NHS Foundation Trust Lewsey Road Luton LU4 0DZ Telephone 01582 49 11 66 and Accounts www.ldh.nhs.uk for the period April 2019 to March 2020 Luton and Dunstable University Hospital NHS Foundation Trust Annual Report & Accounts for the period April 2019 to March 2020 incorporating Quality Account Presented to Parliament pursuant to Schedule 7, paragraph 25 (4) (a) of the National Health Service Act 2006 © 2020 Luton and Dunstable University Hospital NHS Foundation Trust Contents INTRODUCTION 3 GOVERNANCE REPORT 49 About this Report 5 Board of Directors 50 Chief Executive and Chair Statement 6 Committees of the Board of Directors 58 Audit and Risk Committee 59 STRATEGY 7 Council of Governors 62 2020/21 Strategic Approach 8 Foundation Trust Membership 67 Maintaining our Performance 10 Corporate Objectives 2020/21 11 FINANCIAL PERFORMANCE REPORT 71 Performance 2019/20 12 Review of Financial Performance 72 Remuneration report 74 OPERATIONAL PERFORMANCE REPORT 15 Fundraising and Charitable Donations 75 Principal activities of the Trust 16 Review of Operational Performance 18 ANNUAL GOVERNANCE STATEMENT AND Regulatory Quality CQC Performance 19 ACCOUNTS 81 Regulatory Performance Ratings 20 Statement of the Chief Executive’s -

37 Bus Time Schedule & Line Route
37 bus time schedule & line map 37 Dallow View In Website Mode The 37 bus line (Dallow) has 3 routes. For regular weekdays, their operation hours are: (1) Dallow: 7:03 AM - 6:15 PM (2) Dunstable: 9:00 AM - 2:30 PM (3) Luton Town Centre: 6:44 AM - 5:56 PM Use the Moovit App to ƒnd the closest 37 bus station near you and ƒnd out when is the next 37 bus arriving. Direction: Dallow 37 bus Time Schedule 12 stops Dallow Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 7:03 AM - 6:15 PM Galaxy Centre, Luton Town Centre 5 New Bedford Road, Luton Tuesday 7:03 AM - 6:15 PM Liverpool Road, Luton Town Centre Wednesday 7:03 AM - 6:15 PM Dunstable Road, Luton Thursday 7:03 AM - 6:15 PM Dallow Road, Luton Town Centre Friday 7:03 AM - 6:15 PM Dunstable Road, Luton Saturday 8:30 AM - 5:30 PM Vestry Close, Dallow Dallow Primary School, Dallow Newcombe Road, Dallow 37 bus Info Direction: Dallow Bedfordshire Yeoman, Dallow Stops: 12 Trip Duration: 9 min Runley Road, Dallow Line Summary: Galaxy Centre, Luton Town Centre, Liverpool Road, Luton Town Centre, Dallow Road, Foxdell Infant School, Dallow Luton Town Centre, Vestry Close, Dallow, Dallow Primary School, Dallow, Newcombe Road, Dallow, Warren Road, Dallow Bedfordshire Yeoman, Dallow, Runley Road, Dallow, Foxdell Infant School, Dallow, Warren Road, Dallow, Easingwold Gardens, Dallow, Cosgrove Way, Dallow Easingwold Gardens, Dallow Cosgrove Way, Dallow Dallow Road, Luton Direction: Dunstable 37 bus Time Schedule 31 stops Dunstable Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational