H Ica Thera Ractic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Uila Supported Apps
Uila Supported Applications and Protocols updated Oct 2020 Application/Protocol Name Full Description 01net.com 01net website, a French high-tech news site. 050 plus is a Japanese embedded smartphone application dedicated to 050 plus audio-conferencing. 0zz0.com 0zz0 is an online solution to store, send and share files 10050.net China Railcom group web portal. This protocol plug-in classifies the http traffic to the host 10086.cn. It also 10086.cn classifies the ssl traffic to the Common Name 10086.cn. 104.com Web site dedicated to job research. 1111.com.tw Website dedicated to job research in Taiwan. 114la.com Chinese web portal operated by YLMF Computer Technology Co. Chinese cloud storing system of the 115 website. It is operated by YLMF 115.com Computer Technology Co. 118114.cn Chinese booking and reservation portal. 11st.co.kr Korean shopping website 11st. It is operated by SK Planet Co. 1337x.org Bittorrent tracker search engine 139mail 139mail is a chinese webmail powered by China Mobile. 15min.lt Lithuanian news portal Chinese web portal 163. It is operated by NetEase, a company which 163.com pioneered the development of Internet in China. 17173.com Website distributing Chinese games. 17u.com Chinese online travel booking website. 20 minutes is a free, daily newspaper available in France, Spain and 20minutes Switzerland. This plugin classifies websites. 24h.com.vn Vietnamese news portal 24ora.com Aruban news portal 24sata.hr Croatian news portal 24SevenOffice 24SevenOffice is a web-based Enterprise resource planning (ERP) systems. 24ur.com Slovenian news portal 2ch.net Japanese adult videos web site 2Shared 2shared is an online space for sharing and storage. -
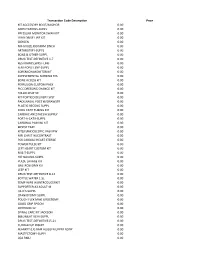
Transaction Code Description
Transaction Code Description Price KIT ACCESSORY BOOT/ANCHOR 0.00 AMPUTATIONS-SUPPL 0.00 PRESSURE MONITOR SWAN KIT 0.00 LVAD DRIVE LINE KIT 0.00 OXYGEN 0.00 NU-GAUZE,IODAFRM 1INCH 0.00 ARTHROTMY-SUPPL 0.00 BONE & OTHER-SUPPL 0.00 DRUG TEST-DEFINITIVE 1-7 0.00 RESTRAINTS,WRST-LMB 0.00 FEM-POPLIT.BYP-SUPPL 0.00 SORENSON MONITOR KIT 0.00 SUPPLEMENTAL NURSING SYS 0.00 BONE ACCESS KIT 0.00 PERFUSION CUSTOM PACK 0.00 PICC DRESSING CHANGE KIT 0.00 FOLLOLWUP 30 0.00 KIT PORTICO DELIVERY SYST 0.00 PACK,NASAL POST W/DRAWSTR 0.00 PLASTIC RECONS-SUPPL 0.00 COOL CATH TUBING KIT 0.00 CARDIAC ANESTHESIA SUPPLY 0.00 PORT-A-CATH-SUPPL 0.00 CARDINAL PAIN INJ KIT 0.00 BIOPSY TRAY 0.00 KIT(LF)ENDOSCOPIC VASVIEW 0.00 MRI CHEST W/CONTRAST 0.00 PCK CARDIAC HEART STERILE 0.00 POWER PULSE KIT 0.00 LEFT HEART CUSTOM KIT 0.00 M & T-SUPPL 0.00 HIP NAILING-SUPPL 0.00 PULSE LAVAGE KIT 0.00 GASTROSTOMY KIT 0.00 LEEP KIT 0.00 DRUG TEST-DEFINITIVE 8-14 0.00 BOTTLE WATER 1.5L 0.00 TEMP WIRE W/INTRODUCERKIT 0.00 SUPPORTER,A3 ADULT-M 0.00 I & D'S-SUPPL 0.00 CRANIOTOMY-SUPPL 0.00 POUCH FLEX MAXI UROSTOMY 0.00 GOOD GRIP SPOON 0.00 OXYHOOD 12- 0.00 SPINAL CARE KIT JACKSON 0.00 BI&UNILAT VEIN-SUPPL 0.00 DRUG TEST-DEFINITIVE15-21 0.00 CUDDLECUP INSERT 0.00 BLANKET (LF) BAIR HUGGER UPPER BODY 0.00 MASTECTOMY-SUPPL 0.00 LOA RMU 0.00 PACK LINQ 0.00 CHOLECYSTECTOM-SUPPL 0.00 RES BWL,SIG,AP-SUPPL 0.00 TRAY BIOPSY GENERAL UTIL 0.00 KIT(LF)CUSTOM SYRINGE ANGIO 0.00 OXISENSOR(LF)PEDI (PINK) 0.00 THORACIC SURG-SUPPL 0.00 NU-GAUZE PLAIN 1/2INCH 0.00 NU-GAUZE,IODAFRM 1/4INCH 0.00 PICC -

Euphemism in Animated Films a Multimodal And
Seeing the unseen: Euphemism in Animated Films A Multimodal and Critical Discourse Study by Dalia Abyd Asseel M.A. (Linguistics) A thesis submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy in THE DEPARTMENT OF LINGUISTICS AND ENGLISH LANGUAGE LANCASTER UNIVERSITY, UK JULY 2020 Abstract Animated films are contemporary popular cultural products recreating the ‘real’ world and engaging massive worldwide audiences of adults and children. Children as the ostensible viewers of animated films may acquire their cultural and ideological knowledge and beliefs about the world from the representations in animated films. Although during the past decade animated films have increasingly been the focus of attention of researchers across different disciplines, including education, gender, sexuality and literacy, studies tackling the discourse and language of animated films are still in their early stages. More specifically, very few studies have investigated the use of euphemism as a major micro-level linguistic device reflecting macro-level discourse and extending to sociocultural structures. To this end, this thesis examines euphemism constructed through the discourse of animated films by employing the strategies of Critical Discourse Studies (CDS). Moreover, Multimodal Discourse Analysis (MDA) is employed to examine discursive strategies involving visual representations accompanying euphemism and what underpins those strategies, and to shed light on the multimodal relations between the representation of both. Euphemism is frequently associated with the notion of taboo. Consequently, new words or phrases are designated to refer to linguistic taboos as alternatives used by speakers to minimise the threat to the audience’s face as well as to their own. -

After the Ball David Williamson
David Williamson’s first full-length play, The Coming of Stork, premiered at the La Mama Theatre, Carlton, in 1970 and later became the film Stork, directed by Tim Burstall. The Removalists and Don’s Party followed in 1971, then Jugglers Three (1972), What If You Died Tomorrow? (1973), The Department (1975), A Handful of Friends (1976), The Club (1977) and Travelling North (1979). In 1972 The Removalists won the Australian Writers’ Guild AWGIE Award for best stage play and the best script in any medium and the British production saw Williamson nominated most promising playwright by the London Evening Standard. The 1980s saw his success continue with Celluloid Heroes (1980), The Perfectionist (1982), Sons of Cain (1985), Emerald City (1987) and Top Silk (1989); whilst the 1990s produced Siren (1990), Money and Friends (1991), Brilliant Lies (1993), Sanctuary (1994), Dead White Males (1995), Heretic (1996), Third World Blues (an adaptation of Jugglers Three) and After the Ball (both in 1997), and Corporate Vibes and Face to Face (both in 1999). The Great Man (2000), Up for Grabs, A Conversation, Charitable Intent (all in 2001), Soulmates (2002), Birthrights (2003), Amigos, Flatfoot (both in 2004), Operator and Influence(both 2005) have since followed. Williamson is widely recognised as Australia’s most successful playwright and over the last thirty years his plays have been performed throughout Australia and produced in Britain, United States, Canada and many European countries. A number of his stage works have been adapted for the screen, including The Removalists, Don’s Party, The Club, Travelling North, Emerald City, Sanctuary and Brilliant Lies. -

The Place of Music, Race and Gender in Producing Appalachian Space
University of Kentucky UKnowledge Theses and Dissertations--Geography Geography 2012 PERFORMING COMMUNITY: THE PLACE OF MUSIC, RACE AND GENDER IN PRODUCING APPALACHIAN SPACE Deborah J. Thompson University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Thompson, Deborah J., "PERFORMING COMMUNITY: THE PLACE OF MUSIC, RACE AND GENDER IN PRODUCING APPALACHIAN SPACE" (2012). Theses and Dissertations--Geography. 1. https://uknowledge.uky.edu/geography_etds/1 This Doctoral Dissertation is brought to you for free and open access by the Geography at UKnowledge. It has been accepted for inclusion in Theses and Dissertations--Geography by an authorized administrator of UKnowledge. For more information, please contact [email protected]. STUDENT AGREEMENT: I represent that my thesis or dissertation and abstract are my original work. Proper attribution has been given to all outside sources. I understand that I am solely responsible for obtaining any needed copyright permissions. I have obtained and attached hereto needed written permission statements(s) from the owner(s) of each third-party copyrighted matter to be included in my work, allowing electronic distribution (if such use is not permitted by the fair use doctrine). I hereby grant to The University of Kentucky and its agents the non-exclusive license to archive and make accessible my work in whole or in part in all forms of media, now or hereafter known. I agree that the document mentioned above may be made available immediately for worldwide access unless a preapproved embargo applies. -

Acme Brick Company: 125 Years Across Three Centuries Is One of His Latest
ACME BRICK COMPANY 125 YEARS ACROSS THREE CENTURIES ACME BRICK COMPANY ACME BRICK COMPANY 125 YEARS ACROSS THREE CENTURIES by Bill Beck Copyright © 2016 by the Acme Brick Company 3024 Acme Brick Plaza Fort Worth, TX 76109 All rights reserved, including the right to reproduce this work in any form whatsoever without permission in writing from the publisher, except for brief passages in connection with a review. For information, please write: The Donning Company Publishers 184 Business Park Drive, Suite 206 Virginia Beach, VA 23462 Lex Cavanah, General Manager Nathan Stufflebean, Production Supervisor Richard A. Horwege, Senior Editor Chad Harper Casey, Graphic Designer Monika Ebertz, Imaging Artist Kathy Snowden Railey, Project Research Coordinator Katie Gardner, Marketing and Production Coordinator James H. Railey, Project Director Library of Congress Cataloging-in-Publication Data Names: Beck, Bill, author. Title: Acme Brick Company : 125 years across three centuries / by Bill Beck. Description: Virginia Beach, VA : The Donning Company Publishers, [2016] | Includes index. Identifiers: LCCN 2016017757 | ISBN 9781681840390 (hard cover : alkaline paper) Subjects: LCSH: Acme Brick Company—History. | Acme Brick Company—Anniversaries, etc. | Brick trade—Texas—Fort Worth—History. | Brickworks—Texas—Fort Worth—History. | Acme Brick Company—Biography. | Fort Worth (Tex.)—Economic conditions. Classification: LCC HD9605.U64 A363 2016 | DDC 338.7/624183609764—dc23 LC record available at https://lccn.loc.gov/2016017757 Printed in the United States -

Trump, Kavanaugh Effect Bury Donnelly Mike Braun Pulls Off an Emphatic Upset As Voters Embrace the President by BRIAN A
V24, N13 Thursday, Nov. 8, 2018 Trump, Kavanaugh effect bury Donnelly Mike Braun pulls off an emphatic upset as voters embrace the president By BRIAN A. HOWEY INDIANAPOLIS – It would be easy to consign Mike Braun’s epic, not-even- close upset of U.S. Sen. Joe Donnelly to a Democratic blunder on Supreme Court Justice Brett Kavanaugh’s confirmation. Don- nelly, along with U.S. Sens. Heidi Heitkamp and Claire McCaskill all voted against Kavanaugh and lost emphatically. West Virginia Democrat U.S. Sen. Joe Manchin supported Kavana- Senator-elect Mike Braun addresses the GOP victory rally Election Night as U.S. Sen. ugh and won easily. Todd Young looks on. (HPI Photo by Mark Curry) Until the allegations of Dr. Christine Blasey Ford surfaced in mid-September, probable yea vote on Kavanaugh, which had that occurred, might have left this race on more parochial footing. Donnelly had narrow poll advantages and Democratic voter intensity far outpaced Republicans. He was a plausible and Continued on page 4 Big showdown that wasn’t By MARK SOUDER FORT WAYNE – The U.S. Senate election in Indi- ana was perceived to be a pivotal showdown for control of that body. It was supposed to be another test of the Republican-lite strategy employed by Evan Bayh to carry “I have supported the Mueller Indiana, a method he con- ceived after watching his father investigation from the beginning fall in an upset to Dan Quayle in 1980. because we need answers about What is hard to remem- Russia’s attempts to influence ber, even for those who re- member that there were two our elections. -

S T a T E D E L E G a T I O N S
S T A T E D E L E G A T I O N S 155 156 State Delegations Number which precedes name of Representative designates Congressional district. Democrats in roman; Republicans in italic; Independent in bold; Independent Democrat in . AlaBAMA SENATORS Richard C. Shelby Jeff Sessions REPRESENTATIVES [Republican, 6; Democrat, 1] 1. Jo Bonner 5. Mo Brooks 2. Martha Roby 6. Spencer Bachus 3. Mike Rogers 7. Terri A. Sewell 4. Robert B. Aderholt AlasKA SENATORS Lisa Murkowski Mark Begich REPRESENTATIVES [Republican, 1] At Large—Don Young 157 STATE DELEGATIONS ARIZONA SENATORS John McCain Jon Kyl REPRESENTATIVES [Republican, 5; Democrat, 3] 1. Paul A. Gosar 5. David Schweikert 2. Trent Franks 6. Jeff Flake 3. Benjamin Quayle 7. Raúl M. Grijalva 4. Ed Pastor 8. Ron Barber ARKansas SENATORS Mark Pryor John Boozman REPRESENTATIVES [Republican, 3; Democrat, 1] 1. Eric A. “Rick’’ Crawford 3. Steve Womack 2. Tim Griffin 4. Mike Ross 158 STATE DELEGATIONS CALIFORNIA SENATORS Dianne Feinstein Barbara Boxer REPRESENTATIVES [Republican, 19; Democrat, 34] 1. Mike Thompson 28. Howard L. Berman 2. Wally Herger 29. Adam B. Schiff 3. Daniel E. Lungren 30. Henry A. Waxman 4. Tom McClintock 31. Xavier Becerra 5. Doris O. Matsui 32. Judy Chu 6. Lynn C. Woolsey 33. Karen Bass 7. George Miller 34. Lucille Roybal-Allard 8. Nancy Pelosi 35. Maxine Waters 9. Barbara Lee 36. Janice Hahn 10. John Garamendi 37. Laura Richardson 11. Jerry McNerney 38. Grace F. Napolitano 12. Jackie Speier 39. Linda T. Sánchez 13. Fortney Pete Stark 40. Edward R. Royce 14. Anna G. -

WOLE SOYINKA: Politics, Poetics and Postcolonialism
This page intentionally left blank WOLE SOYINKA Politics, Poetics and Postcolonialism Biodun Jeyifo examines the connections between the innovative and influential writings of Wole Soyinka and his radical politi- cal activism. Jeyifo carries out detailed analyses of Soyinka’s most ambitious works, relating them to the controversies generated by Soyinka’s use of literature and theatre for radical political purposes. He gives a fascinating account of the profound but paradoxical affinities and misgivings Soyinka has felt about the significance of the avant-garde movements of the twentieth century. Jeyifo also explores Soyinka’s works with regard to the impact on his artistic sensibilities of the pervasiveness of representational ambiguity and linguistic exuberance in Yoruba culture. The analyses and evalu- ations of this study are presented in the context of Soyinka’s sus- tained engagement with the violence of collective experience in post-independence, postcolonial Africa and the developing world. No existing study of Soyinka’s works and career has attempted such a systematic investigation of their complex relationship to politics. is Professor of English at Cornell University. He is the author of The Popular Travelling Theatre of Nigeria () and The Truthful Lie: Essays in a Radical Sociology of African Drama (). He has written essays and monographs on Anglophone African and Caribbean literatures, Marxist cultural theory and colonial and postcolonial studies and has also edited several volumes on African drama and critical discourse. Series editor: Professor Abiola Irele, Ohio State University Each volume in this unique series of critical studies will offer a comprehensive and in-depth account of the whole œuvre of one individual writer from Africa or the Caribbean, in such a way that the book may be considered a complete coverage of the writer’s expression up to the time the study is undertaken. -

State Delegations
STATE DELEGATIONS Number before names designates Congressional district. Democrats in roman; Republicans in italic; Independent in SMALL CAPS; Independent Democrat in SMALL CAPS ITALIC; Resident Commissioner and Delegates in boldface. ALABAMA SENATORS 2. Terry Everett Richard C. Shelby 3. Mike Rogers Jeff Sessions 4. Robert B. Aderholt 5. Robert E. ‘‘Bud’’ Cramer, Jr. REPRESENTATIVES 6. Spencer Bachus [Democrats 2, Republicans 5] 7. Artur Davis 1. Jo Bonner ALASKA SENATORS REPRESENTATIVE Ted Stevens [Republican 1] Lisa Murkowski At Large - Don Young ARIZONA SENATORS 2. Trent Franks John McCain 3. John B. Shadegg Jon Kyl 4. Ed Pastor 5. Harry E. Mitchell REPRESENTATIVES 6. Jeff Flake [Democrats 4, Republicans 4] 7. Rau´l M. Grijalva 1. Rick Renzi 8. Gabrielle Giffords ARKANSAS SENATORS REPRESENTATIVES Blanche L. Lincoln [Democrats 3, Republicans 1] Mark L. Pryor 1. Marion Berry 2. Vic Snyder 3. John Boozman 4. Mike Ross CALIFORNIA SENATORS 2. Wally Herger Dianne Feinstein 3. Daniel E. Lungren Barbara Boxer 4. John T. Doolittle 5. Doris O. Matsui REPRESENTATIVES 6. Lynn C. Woolsey [Democrats 33, Republicans 19] 7. George Miller 1. Mike Thompson 8. Nancy Pelosi 295 296 Congressional Directory 9. Barbara Lee 32. Hilda L. Solis 10. Ellen O. Tauscher 33. Diane E. Watson 11. Jerry McNerney 34. Lucille Roybal-Allard 12. Tom Lantos 35. Maxine Waters 13. Fortney Pete Stark 36. Jane Harman 14. Anna G. Eshoo 37. —— 1 15. Michael M. Honda 38. Grace F. Napolitano 16. Zoe Lofgren 39. Linda T. Sa´nchez 17. Sam Farr 40. Edward R. Royce 18. Dennis A. Cardoza 41. Jerry Lewis George Radanovich 19. -

IGDA Online Games White Paper Full Version
IGDA Online Games White Paper Full Version Presented at the Game Developers Conference 2002 Created by the IGDA Online Games Committee Alex Jarett, President, Broadband Entertainment Group, Chairman Jon Estanislao, Manager, Media & Entertainment Strategy, Accenture, Vice-Chairman FOREWORD With the rising use of the Internet, the commercial success of certain massively multiplayer games (e.g., Asheron’s Call, EverQuest, and Ultima Online), the ubiquitous availability of parlor and arcade games on “free” game sites, the widespread use of matching services for multiplayer games, and the constant positioning by the console makers for future online play, it is apparent that online games are here to stay and there is a long term opportunity for the industry. What is not so obvious is how the independent developer can take advantage of this opportunity. For the two years prior to starting this project, I had the opportunity to host several roundtables at the GDC discussing the opportunities and future of online games. While the excitement was there, it was hard not to notice an obvious trend. It seemed like four out of five independent developers I met were working on the next great “massively multiplayer” game that they hoped to sell to some lucky publisher. I couldn’t help but see the problem with this trend. I knew from talking with folks that these games cost a LOT of money to make, and the reality is that only a few publishers and developers will work on these projects. So where was the opportunity for the rest of the developers? As I spoke to people at the roundtables, it became apparent that there was a void of baseline information in this segment. -

Doherty, Thomas, Cold War, Cool Medium: Television, Mccarthyism
doherty_FM 8/21/03 3:20 PM Page i COLD WAR, COOL MEDIUM TELEVISION, McCARTHYISM, AND AMERICAN CULTURE doherty_FM 8/21/03 3:20 PM Page ii Film and Culture A series of Columbia University Press Edited by John Belton What Made Pistachio Nuts? Early Sound Comedy and the Vaudeville Aesthetic Henry Jenkins Showstoppers: Busby Berkeley and the Tradition of Spectacle Martin Rubin Projections of War: Hollywood, American Culture, and World War II Thomas Doherty Laughing Screaming: Modern Hollywood Horror and Comedy William Paul Laughing Hysterically: American Screen Comedy of the 1950s Ed Sikov Primitive Passions: Visuality, Sexuality, Ethnography, and Contemporary Chinese Cinema Rey Chow The Cinema of Max Ophuls: Magisterial Vision and the Figure of Woman Susan M. White Black Women as Cultural Readers Jacqueline Bobo Picturing Japaneseness: Monumental Style, National Identity, Japanese Film Darrell William Davis Attack of the Leading Ladies: Gender, Sexuality, and Spectatorship in Classic Horror Cinema Rhona J. Berenstein This Mad Masquerade: Stardom and Masculinity in the Jazz Age Gaylyn Studlar Sexual Politics and Narrative Film: Hollywood and Beyond Robin Wood The Sounds of Commerce: Marketing Popular Film Music Jeff Smith Orson Welles, Shakespeare, and Popular Culture Michael Anderegg Pre-Code Hollywood: Sex, Immorality, and Insurrection in American Cinema, ‒ Thomas Doherty Sound Technology and the American Cinema: Perception, Representation, Modernity James Lastra Melodrama and Modernity: Early Sensational Cinema and Its Contexts Ben Singer