Impaired HSF1 Transactivation Drives Proteostasis Collapse and Senescent Phenotype of IPF Lung Fibroblast
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Supporting Information for a Microrna Network Regulates
Supporting Information for A microRNA Network Regulates Expression and Biosynthesis of CFTR and CFTR-ΔF508 Shyam Ramachandrana,b, Philip H. Karpc, Peng Jiangc, Lynda S. Ostedgaardc, Amy E. Walza, John T. Fishere, Shaf Keshavjeeh, Kim A. Lennoxi, Ashley M. Jacobii, Scott D. Rosei, Mark A. Behlkei, Michael J. Welshb,c,d,g, Yi Xingb,c,f, Paul B. McCray Jr.a,b,c Author Affiliations: Department of Pediatricsa, Interdisciplinary Program in Geneticsb, Departments of Internal Medicinec, Molecular Physiology and Biophysicsd, Anatomy and Cell Biologye, Biomedical Engineeringf, Howard Hughes Medical Instituteg, Carver College of Medicine, University of Iowa, Iowa City, IA-52242 Division of Thoracic Surgeryh, Toronto General Hospital, University Health Network, University of Toronto, Toronto, Canada-M5G 2C4 Integrated DNA Technologiesi, Coralville, IA-52241 To whom correspondence should be addressed: Email: [email protected] (M.J.W.); yi- [email protected] (Y.X.); Email: [email protected] (P.B.M.) This PDF file includes: Materials and Methods References Fig. S1. miR-138 regulates SIN3A in a dose-dependent and site-specific manner. Fig. S2. miR-138 regulates endogenous SIN3A protein expression. Fig. S3. miR-138 regulates endogenous CFTR protein expression in Calu-3 cells. Fig. S4. miR-138 regulates endogenous CFTR protein expression in primary human airway epithelia. Fig. S5. miR-138 regulates CFTR expression in HeLa cells. Fig. S6. miR-138 regulates CFTR expression in HEK293T cells. Fig. S7. HeLa cells exhibit CFTR channel activity. Fig. S8. miR-138 improves CFTR processing. Fig. S9. miR-138 improves CFTR-ΔF508 processing. Fig. S10. SIN3A inhibition yields partial rescue of Cl- transport in CF epithelia. -

Gene and Protein Expression Profiling of Human Ovarian Cancer Cells Treated with the Heat Shock Protein 90 Inhibitor 17-Allylamino-17-Demethoxygeldanamycin
Research Article Gene and Protein Expression Profiling of Human Ovarian Cancer Cells Treated with the Heat Shock Protein 90 Inhibitor 17-Allylamino-17-Demethoxygeldanamycin Alison Maloney,1 Paul A. Clarke,1 Soren Naaby-Hansen,3,4 Rob Stein,3,5 Jens-Oliver Koopman,3,4 Akunna Akpan,3,4 Alice Yang,3,4 Marketa Zvelebil,3,4 Rainer Cramer,3,4 Lindsay Stimson,1 Wynne Aherne,1 Udai Banerji,1,2 Ian Judson,1,2 Swee Sharp,1 Marissa Powers,1 Emmanuel deBilly,1 Joanne Salmons,1 Michael Walton,1 Al Burlingame,3,4 Michael Waterfield,3,4 and Paul Workman1 1Haddow Laboratories, Cancer Research UK Centre for Cancer Therapeutics, The Institute of Cancer Research; 2Royal Marsden NHS Foundation Trust, Sutton, Surrey, United Kingdom; 3Ludwig Institute for Cancer Research and Departments of 4Biochemistry and Molecular Biology and 5Oncology, University College London, London, United Kingdom Abstract anticancer agents and provide a means of obtaining a detailed The promising antitumor activity of 17-allylamino-17-deme- molecular signature of drug action (1, 2). In addition, these thoxygeldanamycin (17AAG) results from inhibition of the methods may identify pharmacodynamic markers that can be used molecular chaperone heat shock protein 90(HSP90)and to evaluate drugs in clinical trials. Gene expression microarrays are subsequent degradation of multiple oncogenic client proteins. increasingly used to investigate the molecular responses to cancer Gene expression microarray and proteomic analysis were used drugs in tumor cells (1). Although valuable, analysis of gene to profile molecular changes in the A2780human ovarian expression at the mRNA level alone cannot adequately predict cancer cell line treated with 17AAG. -

Heat Shock Proteins in Vascular Diabetic Complications: Review and Future Perspective
International Journal of Molecular Sciences Review Heat Shock Proteins in Vascular Diabetic Complications: Review and Future Perspective Stefania Bellini 1,†, Federica Barutta 1,†, Raffaella Mastrocola 2 ID , Luigi Imperatore 1, Graziella Bruno 1 and Gabriella Gruden 1,* 1 Laboratory of Diabetic Nephropathy, Department of Medical Sciences, University of Turin, Corso Dogliotti 14, 10126 Turin, Italy; [email protected] (S.B.); [email protected] (F.B.); [email protected] (L.I.); [email protected] (G.B.) 2 Department of Clinical and Biological Sciences, University of Turin, Corso Raffaello 30, 10125 Turin, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-011-633-6035 † These authors contribute equally to this work. Received: 27 November 2017; Accepted: 11 December 2017; Published: 14 December 2017 Abstract: Heat shock proteins (HSPs) are a large family of proteins highly conserved throughout evolution because of their unique cytoprotective properties. Besides assisting protein refolding and regulating proteostasis under stressful conditions, HSPs also play an important role in protecting cells from oxidative stress, inflammation, and apoptosis. Therefore, HSPs are crucial in counteracting the deleterious effects of hyperglycemia in target organs of diabetes vascular complications. Changes in HSP expression have been demonstrated in diabetic complications and functionally related to hyperglycemia-induced cell injury. Moreover, associations between diabetic complications and altered circulating levels of both HSPs and anti-HSPs have been shown in clinical studies. HSPs thus represent an exciting therapeutic opportunity and might also be valuable as clinical biomarkers. However, this field of research is still in its infancy and further studies in both experimental diabetes and humans are required to gain a full understanding of HSP relevance. -

Figure S1. HAEC ROS Production and ML090 NOX5-Inhibition
Figure S1. HAEC ROS production and ML090 NOX5-inhibition. (a) Extracellular H2O2 production in HAEC treated with ML090 at different concentrations and 24 h after being infected with GFP and NOX5-β adenoviruses (MOI 100). **p< 0.01, and ****p< 0.0001 vs control NOX5-β-infected cells (ML090, 0 nM). Results expressed as mean ± SEM. Fold increase vs GFP-infected cells with 0 nM of ML090. n= 6. (b) NOX5-β overexpression and DHE oxidation in HAEC. Representative images from three experiments are shown. Intracellular superoxide anion production of HAEC 24 h after infection with GFP and NOX5-β adenoviruses at different MOIs treated or not with ML090 (10 nM). MOI: Multiplicity of infection. Figure S2. Ontology analysis of HAEC infected with NOX5-β. Ontology analysis shows that the response to unfolded protein is the most relevant. Figure S3. UPR mRNA expression in heart of infarcted transgenic mice. n= 12-13. Results expressed as mean ± SEM. Table S1: Altered gene expression due to NOX5-β expression at 12 h (bold, highlighted in yellow). N12hvsG12h N18hvsG18h N24hvsG24h GeneName GeneDescription TranscriptID logFC p-value logFC p-value logFC p-value family with sequence similarity NM_052966 1.45 1.20E-17 2.44 3.27E-19 2.96 6.24E-21 FAM129A 129. member A DnaJ (Hsp40) homolog. NM_001130182 2.19 9.83E-20 2.94 2.90E-19 3.01 1.68E-19 DNAJA4 subfamily A. member 4 phorbol-12-myristate-13-acetate- NM_021127 0.93 1.84E-12 2.41 1.32E-17 2.69 1.43E-18 PMAIP1 induced protein 1 E2F7 E2F transcription factor 7 NM_203394 0.71 8.35E-11 2.20 2.21E-17 2.48 1.84E-18 DnaJ (Hsp40) homolog. -

Investigation Into the Structure and Function of Hsp47
Investigation into the structure and function of Hsp47 Umbreen Ahmed A thesis submitted to the University of Birmingham for the degree of Doctor of Philosophy School of Biosciences University of Birmingham Birmingham B15 2TT May 2009 University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. Acknowledgements Firstly, a huge thanks to my supervisor, Dr Timothy Dafforn for his continuous support, enthusiasm and patience throughout my PhD. It has been a pleasure working for him, even when the lab work has not been particularly rewarding! Our many conversations on cars and formula 1 have been especially enjoyable and will be missed. I would also like to thank our collaborators from Imperial College (Andrew Miller, Dee Olerenshaw, Takayuki Homma, Micheal Wright and Firdaus Abdul) who provided me with the Mus musculus Hsp47 clones. Their mutagenesis work has made this thesis possible and our fruitful discussions have been both interesting and helpful. Thanks also to the James Whisstock group at Monash University, Australia, for providing me with the opportunity to work with such enthusiastic and dedicated scientists. I am indebted to others for their valuable time, expertise and use of instrumentation with regard to specific techniques; Dr Corrine Smith for electron microscopy and Dr Klaus Fütterer for protein crystallography. -

Heat Shock Proteins in Diabetes and Wound Healing
Current Protein and Peptide Science, 2009, 10, 85-95 85 Heat Shock Proteins in Diabetes and Wound Healing Mustafa Atalay1,*, Niku Oksala1, 2, Jani Lappalainen1,3, David E. Laaksonen1,4, Chandan K. Sen5 and 5 Sashwati Roy 1Institute of Biomedicine, Physiology, University of Kuopio, Finland; 2Department of Surgery, Tampere University Hos- pital, Finland; 3Wihuri Research Institute, Helsinki, Finland; 4Institute of Clinical Medicine, Internal Medicine, Univer- sity of Kuopio, Kuopio, Finland; 5Comprehensive Wound Center, Department of Surgery, Dorothy M. Davis Heart & Lung Research Institute, The Ohio State University Medical Center, Columbus, OH, USA Abstract: The heat shock proteins (HSPs), originally identified as heat-inducible gene products, are a highly conserved family of proteins that respond to a wide variety of stress. Although HSPs are among the most abundant intracellular pro- teins, they are expressed at low levels under normal physiological conditions, and show marked induction in response to various stressors. HSPs function primarily as molecular chaperones, facilitating the folding of other cellular proteins, pre- venting protein aggregation, or targeting improperly folded proteins to specific pathways for degradation. By modulating inflammation, wound debris clearance, cell proliferation, migration and collagen synthesis, HSPs are essential for normal wound healing of the skin. In this review, our goal is to discuss the role and clinical implications of HSP with respect to skin wound healing and diabetes. The numerous defects in the function of HSPs associated with diabetes could contribute to the commonly observed complications and delayed wound healing in diabetics. Several physical, pharmacological and genetic approaches may be considered to address HSP-directed therapies both in the laboratory and in the clinics. -

Functional Genomics Study of Acute Heat Stress Response in the Small
www.nature.com/scientificreports OPEN Functional genomics study of acute heat stress response in the small yellow follicles of layer-type Received: 30 January 2017 Accepted: 11 December 2017 chickens Published: xx xx xxxx Chuen-Yu Cheng1, Wei-Lin Tu1, Chao-Jung Chen2,3, Hong-Lin Chan4,5, Chih-Feng Chen1,6,7, Hsin-Hsin Chen1, Pin-Chi Tang1,2, Yen-Pai Lee1, Shuen-Ei Chen1,6,7 & San-Yuan Huang 1,6,7,8 This study investigated global gene and protein expression in the small yellow follicle (SYF; 6–8 mm in diameter) tissues of chickens in response to acute heat stress. Twelve 30-week-old layer-type hens were divided into four groups: control hens were maintained at 25 °C while treatment hens were subjected to acute heat stress at 36 °C for 4 h without recovery, with 2-h recovery, and with 6-h recovery. SYFs were collected at each time point for mRNA and protein analyses. A total of 176 genes and 93 distinct proteins with diferential expressions were identifed, mainly associated with the molecular functions of catalytic activity and binding. The upregulated expression of heat shock proteins and peroxiredoxin family after acute heat stress is suggestive of responsive machineries to protect cells from apoptosis and oxidative insults. In conclusion, both the transcripts and proteins associated with apoptosis, stress response, and antioxidative defense were upregulated in the SYFs of layer-type hens to alleviate the detrimental efects by acute heat stress. However, the genomic regulations of specifc cell type in response to acute heat stress of SYFs require further investigation. -
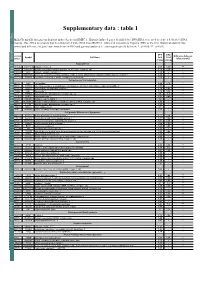
Supplementary Data : Table 1
Supplementary data : table 1 Table 1: Chemically and gazeous hypoxia-induced genes in HMEC-1. Hypoxia-induced genes identified by cDNA RDA were used to create a dedicated cDNA microarray. This cDNA microarray was then hybridized with cDNA from HMEC-1 cultured in normoxia or hypoxia (DFO or 2% O2). Statistical analysis was performed and difference of gene expression between DFO and gaz was analysed ( - : non significatively different; * : p<0,05; ** : p<0,01). DFO GAZ Accession Difference between Symbol Full Name Fold Fold Number DFO and GAZ change change Angiogenesis AF202636 ANGPTL4 angiopoietin-like 4 2,68 1,89 ** K03021 unknown Human tissue plasminogen activator (PLAT) gene, complete cds 1,73 1,26 * AF028593 JAG1 jagged 1 (Alagille syndrome) 1,35 - - M14083 SERPINE1 serine (or cysteine) proteinase inhibitor, clade E (nexin, plasminogen activator inhibitor type 1), member 1 1,28 - - AK025195 ROBO4 roundabout homolog 4, magic roundabout (Drosophila) 1,16 - - Cell adhesion/ Cell migration M84150 LOX lysyl oxidase 2,48 1,78 * U90441 P4HA2 procollagen-proline, 2-oxoglutarate 4-dioxygenase (proline 4-hydroxylase), alpha polypeptide II 1,93 - - AB023207 CHSY1 carbohydrate (chondroitin) synthase 1 1,78 1,62 - M10905 FN1 fibronectin 1 1,74 1,34 ** X54131 PTPRB protein tyrosine phosphatase, receptor type, B 1,6 1,3 * XM_031617 THBS1 thrombospondin 1 1,53 1,42 - M76729 COL5A1 collagen, type V, alpha 1 1,4 - - J05593 HUMTIMP2 Human metalloproteinase-2 inhibitor (TIMP-2) mRNA, complete cds 1,39 - - Y00815 PTPRF protein tyrosine phosphatase, receptor type, F 1,35 - - NM_002318 LOXL2 lysyl oxidase-like 2 1,3 - - E10341 unknown cDNA encoding human pro-cathepsin B. -

Shock Transcription Factor 1 Heat Shock Element Binding Activity Of
Induction of Heat Shock Protein 47 Synthesis by TGF- β and IL-1β Via Enhancement of the Heat Shock Element Binding Activity of Heat Shock Transcription Factor 1 This information is current as of September 29, 2021. Hiroyoshi Sasaki, Tsutomu Sato, Naofumi Yamauchi, Tetsuro Okamoto, Daisuke Kobayashi, Satoshi Iyama, Junji Kato, Takuya Matsunaga, Rishu Takimoto, Tetsuji Takayama, Katsuhisa Kogawa, Naoki Watanabe and Yoshiro Niitsu Downloaded from J Immunol 2002; 168:5178-5183; ; doi: 10.4049/jimmunol.168.10.5178 http://www.jimmunol.org/content/168/10/5178 http://www.jimmunol.org/ References This article cites 32 articles, 11 of which you can access for free at: http://www.jimmunol.org/content/168/10/5178.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 29, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2002 by The American Association of Immunologists All rights reserved. -

Protein Quality Control in the Endoplasmic Reticulum and Cancer
Review Protein Quality Control in the Endoplasmic Reticulum and Cancer Hye Won Moon 1,2,†, Hye Gyeong Han 1,2,† and Young Joo Jeon 1,2,* 1 Department of Biochemistry, Chungnam National University College of Medicine, Daejeon 35015, Korea; [email protected] (H.W.M.); [email protected] (H.G.H.) 2 Department of Medical Science, Chungnam National University College of Medicine, Daejeon 35015, Korea * Correspondence: [email protected]; Tel.: +82-42-280-6766; Fax: +82-42-280-6769 † These authors contributed equally to this work. Received: 8 September 2018; Accepted: 1 October 2018; Published: 3 October 2018 Abstract: The endoplasmic reticulum (ER) is an essential compartment of the biosynthesis, folding, assembly, and trafficking of secretory and transmembrane proteins, and consequently, eukaryotic cells possess specialized machineries to ensure that the ER enables the proteins to acquire adequate folding and maturation for maintaining protein homeostasis, a process which is termed proteostasis. However, a large variety of physiological and pathological perturbations lead to the accumulation of misfolded proteins in the ER, which is referred to as ER stress. To resolve ER stress and restore proteostasis, cells have evolutionary conserved protein quality-control machineries of the ER, consisting of the unfolded protein response (UPR) of the ER, ER-associated degradation (ERAD), and autophagy. Furthermore, protein quality-control machineries of the ER play pivotal roles in the control of differentiation, progression of cell cycle, inflammation, immunity, and aging. Therefore, severe and non-resolvable ER stress is closely associated with tumor development, aggressiveness, and response to therapies for cancer. In this review, we highlight current knowledge in the molecular understanding and physiological relevance of protein quality control of the ER and discuss new insights into how protein quality control of the ER is implicated in the pathogenesis of cancer, which could contribute to therapeutic intervention in cancer. -

Heat Shock Protein 70 (HSP70) Protein-Protein Interactions and a Putative Mechanism for the Potential Benefits of Heat Therapy for Type 2 Diabetes Mellitus
Biochemistry and Molecular Biology 2021; 6(2): 19-24 http://www.sciencepublishinggroup.com/j/bmb doi: 10.11648/j.bmb.20210602.11 ISSN: 2575-5064 (Print); ISSN: 2575-5048 (Online) Heat Shock Protein 70 (HSP70) Protein-Protein Interactions and a Putative Mechanism for the Potential Benefits of Heat Therapy for Type 2 Diabetes Mellitus Magellan Guewo-Fokeng 1, 2, Eugene Sobngwi 2, 3, 4, Barbara Atogho-Tiedeu 2, 5, Jean-Claude Mbanya 2, 3, 4, Wilfred Mbacham 1, 2, * 1Department of Biochemistry, Faculty of Medicine and Biomedical Sciences, University of Yaounde I, Yaounde, Cameroon 2The Biotechnology Centre, University of Yaounde I, Nkolbisson, Yaounde, Cameroon 3Department of Internal Medicine and Specialties, Faculty of Medicine and Biomedical Sciences, University of Yaounde I, Yaounde, Cameroon 4National Obesity Centre, Diabetes, Endocrinology and Metabolic Diseases, Yaounde Central Hospital, Yaounde, Cameroon 5Department of Biochemistry, Faculty of Science, University of Yaounde I, Yaounde, Cameroon Email address: *Corresponding author To cite this article: Magellan Guewo-Fokeng, Eugene Sobngwi, Barbara Atogho-Tiedeu, Jean-Claude Mbanya, Wilfred Mbacham. Heat Shock Protein 70 (HSP70) Protein-Protein Interactions and a Putative Mechanism for the Potential Benefits of Heat Therapy for Type 2 Diabetes Mellitus. Biochemistry and Molecular Biology . Vol. 6, No. 2, 2021, pp. 19-24. doi: 10.11648/j.bmb.20210602.11 Received : March 4, 2021; Accepted : April 30, 2021; Published : May 8, 2021 Abstract: The use of heat therapy to treat diseases was very common in Africa. To date, the number of people using this form of therapy is very much on the decrease. Data on the molecular action mechanisms of how it might induce beneficial effects remain unknown. -

Exploring Cellular Stress Response and Chaperones
cells Editorial Exploring Cellular Stress Response and Chaperones Alessandra Stacchiotti 1,2 1 Anatomy and Physiopathology Division, Department of Clinical and Experimental Sciences, Viale Europa 11, 25123 Brescia, Italy; [email protected]; Tel.: +39-030-3717478; Fax: +39-030-3717486 2 Interdepartmental University Center of Research “Adaptation and Regeneration of Tissues and Organs-(ARTO)”, University of Brescia, 25123 Brescia, Italy Received: 30 April 2019; Accepted: 2 May 2019; Published: 2 May 2019 Abstract: Since the pioneering discovery of heat shock proteins in Drosophila by Ferruccio Ritossa in 1960s, a long and exciting journey has been undertaken by molecular biologists and researchers worldwide. Not only lower organisms like worms, yeast, amoeba, and flies but also eukaryotes share common cellular response signals to stressful conditions that can arise from the outside but also from the inside. Moreover, extraordinary interplay between nucleus and subcellular organelles, and between different organelles, like mitochondria and the endoplasmic reticulum called mitochondria-associated endoplasmic reticulum membranes (MAMs), are involved in aging and human diseases like obesity, diabetes, inflammation, neurodegeneration, autoimmune diseases, atherosclerosis, and cancer. Actually, we know that to hit abnormal proteostasis and lipid exchanges in the endoplasmic reticulum is crucial to best guide effective therapies or discover new drugs. Indeed, restoration or impairment of endoplasmic reticulum shape and function lead to cellular homeostasis by autophagy or to final death generally by apoptosis or pyroptosis. This Special Issue collects current valuable articles or reviews on cellular stress research and each contribution opens a new window for further studies and hypothesis. I hope that readers interested in this fascinating topic may be stimulated to know more and more.