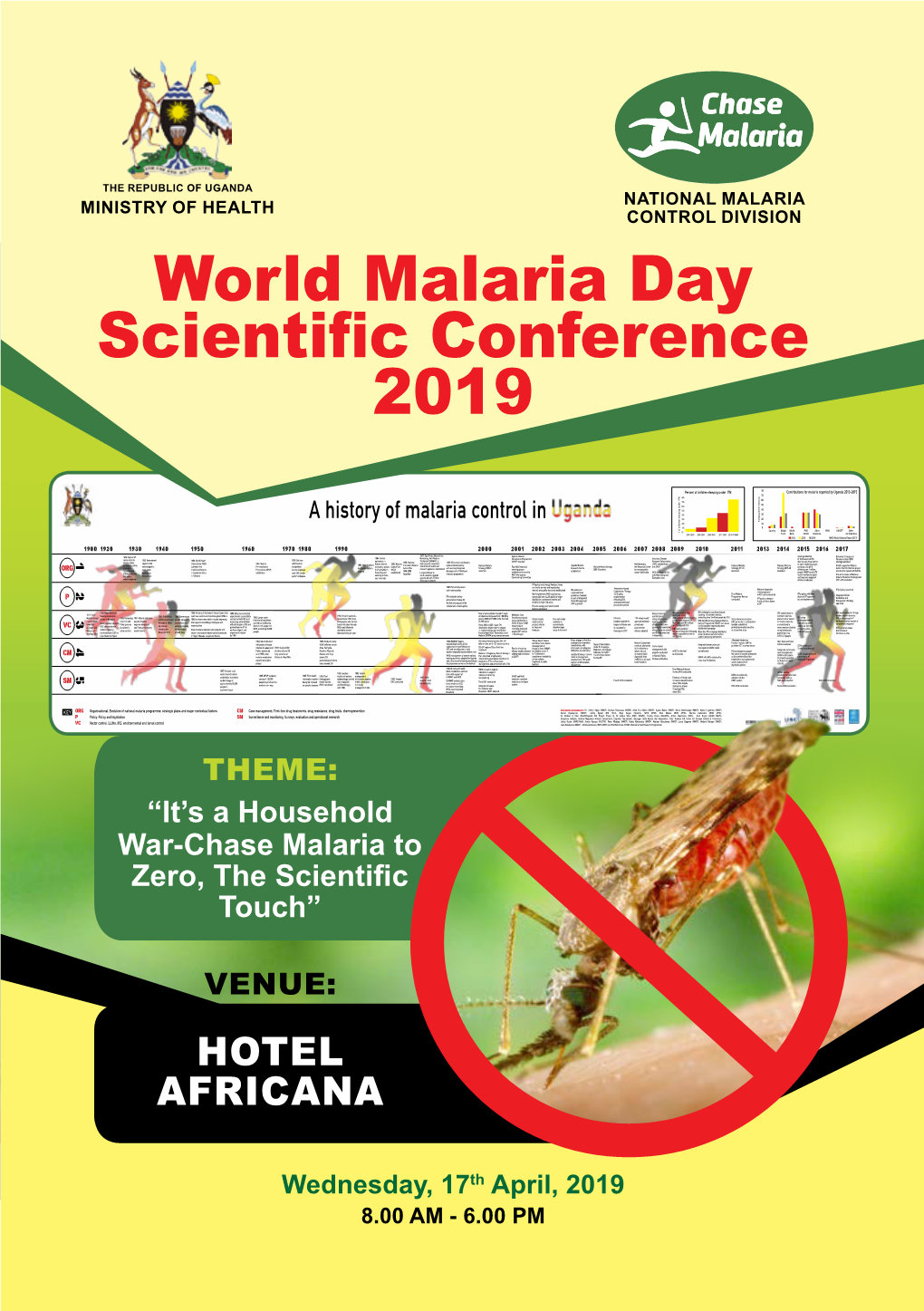
World Malaria Day Scientific Conference 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Malaria Day 2021
This year, World Malaria Day is running with the backdrop of countries around the world continuing to fight the COVID-19 pandemic. Apr 25, 2021 The COVID-19 pandemic highlights the importance of robust health systems to respond to disease outbreaks and to control other deadly diseases such as malaria. On World Malaria Day, April 25, we are calling on the global health community to continue to uphold progress and commitments made in the fight to end malaria. Follow us on social media at #MalariaFuture In 1999, Novartis launched the first fixed-dose Artemisinin-based Combination Therapy (ACT) and in 2009, the first dispersible pediatric ACT developed in partnership with Medicines for Malaria Venture (MMV). Over the past 20 years, together with our partners, we have delivered nearly 1 billion treatments, including over 430 million pediatric treatments to malaria-endemic countries. Working on next-generation antimalarials Novartis is advancing Research & Development of next-generation treatments to combat emerging drug resistance. We lead five malaria development programs worldwide, featuring three compounds that employ new mechanisms of action and activity against artemisinin-resistant strains of the disease. KAF156 belongs to a novel class of antimalarial compounds that act against both the blood and liver stages of the parasite's lifecycle. It demonstrated activity against both vivax and falciparum malaria, including artemisinin-resistant parasites. Novartis leads the development of this compound with scientific and financial support from MMV in collaboration with the Bill & Melinda Gates Foundation. KAE609 is another novel antimalarial compound demonstrating rapid clearance of parasites pre-clinically and in patients. Novartis is leading the development of KAE609 in collaboration with MMV and with financial support from the Wellcome Trust. -

Malaria Consortium
Malaria Consortium 2003-2013: a decade in communicable disease control and child health Contents 1 Chair’s foreword 2 Our birth and growth 6 Malaria Consortium, 2003-2013 8 Our evolution at country level 14 Disease control: malaria and neglected tropical diseases 22 Linking the community to health systems 30 Moving to elimination 38 Going forward Thank you The last 10 years for Malaria Consortium have been made possible thanks to the unwavering support of our donors, partners and collaborators from across the world. Collaboration and cooperation with others has been the cornerstone of all our achievements in the fight against malaria and other communicable childhood and neglected tropical diseases. It is thanks to these partnerships that we are able to provide some of the world’s most vulnerable people with better health care and offer them a chance for a future free from the burden of diseases which are treatable and preventable. t A key focus of Malaria Consortium has been effective diagnosis of malaria which helps save millions of lives Tadej Znidarcic Tadej Growing through innovation and partnership Malaria Consortium was founded by a small team of people with a vision – to build the capacity of malaria-endemic countries worldwide to deal with a common and treatable disease that was devastating the lives of poor and vulnerable communities. Over the course of a decade of innovation and Whilst the organisation has grown significantly, our strong partnerships, this vision has grown from focus on the national and grassroots level has enabled focusing solely on malaria control and prevention, us to remain an effective on-the-ground partner, which to include integrated approaches to improving child has meant that in all that we have done, we have health and neglected tropical diseases. -

Urban Malaria, the Malaria of the Future?
Urban Malaria, the Malaria of the Future? Following the ongoing rural exodus and rapid, unregulated urban development around large African cities, malaria – once viewed as a rural disease – is becoming a growing health problem in urban and suburban areas. Introduction Half the world’s population is at risk of malaria; close to 100 Along with AIDS and tuberculosis, malaria is one of the main public countries across Africa, Asia-Pacific and the Americas. Every year, health problems threatening the development of the poorest malaria causes over 200 million cases and over 400,000 deaths, countries. more than 90% of which occur in Africa. Despite significant progress since 2000, with 7.6 million lives It is estimated that in Africa, a child dies from malaria every two saved and 1.5 billion new infections averted, the number of cases minutes and that the disease is one of the leading causes of is stagnating for the first time, particularly in highest burden death in children under 5 on the continent. Many children who African countries. The uncontrolled development of some African survive a case of severe malaria present with learning difficulties cities and global warming are resulting in a dangerous increase or suffer brain damage. Pregnant women and unborn babies are in the number of breeding grounds for the mosquitoes that carry also particularly vulnerable to malaria, which is a major cause of the malaria parasite and we are seeing the emergence of urban perinatal mortality, low birth weight and maternal anaemia. malaria, which could develop into an epidemic at any time. -

Press Release, World Malaria Day Press Release
PRESS RELEASE We need more investment, commitment to defeat malaria Accra, 25th April 2015. Despite declines in malaria cases and deaths in recent years, many lives are still lost to the disease each year. But it can be treated, and eventually eradicated. As we celebrate the World Malaria Day today, we must recognize the need for sufficient global commitment and investment if we are to win the fight against malaria. “Malaria is still a major cause of morbidity and mortality with up to 60% of the admissions locally attributed to malaria or malaria and other co-infections. The burden to the health care is huge and every effort should be directed to fight this disease and reduce the human suffering and especially for the children,” says Dr Walter Otieno, Director of the Kombewa Clinical Research Centre, an INDEPTH member centre in Kenya. At least three quarters of malaria deaths occur in children under 5. But according to WHO, in 2013, only about 1 in 5 African children with malaria received effective treatment for the disease, 15 million pregnant women did not receive a single dose of the recommended preventive drugs, and an estimated 278 million people in Africa still live in households without a single insecticide-treated bednet. It is important we recognize the need to invest in all aspects of malaria prevention, control, treatment and in research in order to win the war against the disease and its devastating effects. Already, the Malaria Consortium notes that drug resistance is a global problem that threatens the progress made in recent years. -

WHA60.18 Malaria, Including Proposal for Establishment of World Malaria Day 60Th World Health Assembly (May 2007)
WHA60.18 Malaria, including proposal for establishment of World Malaria Day 60th World Health Assembly (May 2007) The Sixtieth World Health Assembly, Having considered the report on malaria, including a proposal for the establishment of Malaria Day; Concerned that malaria continues to cause more than one million preventable deaths a year; Noting that the Global Fund to Fight AIDS, Tuberculosis and Malaria, the World Bank Global Strategy and Booster Program, the Bill & Melinda Gates Foundation, the Malaria Initiative of the President of the United States of America, and other donors have made substantial resources available; Welcoming the contribution to the mobilization of resources for development of voluntary innovative financing initiatives taken by groups of Member States and, in this regard, noting the activities of the International Drug Purchase Facility (UNITAID); Recalling that combating HIV/AIDS, malaria and other diseases is included in internationally agreed health-related development goals, including those contained in the Millennium Declaration; Mindful that the global burden of malaria needs to be decreased in order to reach the Millennium Development Goal of reducing the mortality rate among children under five by two thirds by 2015 and to help to achieve the Millennium Development Goals of improving maternal health and eradicating extreme poverty, URGES Member States: (1) to apply to their specific contexts the evidence-based policies, strategies and tools recommended by WHO and performance-based monitoring and evaluation -

World Malaria Day 2021
World Malaria Day 2021 drishtiias.com/printpdf/world-malaria-day-2021 Why in News The report, titled ‘Zeroing in on malaria elimination’, was released by the World Health Organization (WHO) ahead of World Malaria Day 2021. World Malaria Day is observed on 25th April every year. The 2021 theme is “Reaching the Zero Malaria target". The WHO has also identified 25 countries with the potential to eradicate malaria by 2025 under its ‘E-2025 Initiative’. Key Points 1/3 Malaria: About: Malaria is a life threatening mosquito borne blood disease caused by plasmodium parasites. It is predominantly found in the tropical and subtropical areas of Africa, South America as well as Asia. The parasites spread through the bites of infected female Anopheles mosquitoes. After entering the human body, parasites initially multiply within the liver cells and then attack the Red Blood Cells (RBCs) resulting in their rupture. There are 5 parasite species that cause malaria in humans, and 2 of these species – Plasmodium falciparum and Plasmodium vivax – pose the greatest threat. Symptoms of malaria include fever and flu-like illness, including shaking chills, headache, muscle aches, and tiredness. It is preventable as well as curable. Malaria Vaccine: Known by its lab initials as RTS,S but branded as Mosquirix, the vaccine has passed lengthy scientific trials that found it to be safe and reducing the risk of malaria by nearly 40%, the best ever recorded. It was developed by GlaxoSmithKline (GSK) company and approved by the European Medicines Agency in 2015. The RTS,S vaccine trains the immune system to attack the malaria parasite (Plasmodium (P.) falciparum, the most deadly species of the malaria parasite). -

Malaria Controls That Work
PRESS RELEASE Nernstweg 32, 22765 Hamburg, Tel. 040-399 19 10-0, Fax 040-399 19 10-30, [email protected], www.pan-germany.org Hamburg, 19 April 2010 Malaria controls that work Global network points to successful, safe solutions on World Malaria Day Every day, children are still dying of malaria - a devastating disease that is both preventable and curable. To mark World Malaria Day this April 25th, Pesticide Action Network (PAN) International is calling on public health experts, national malaria control officials and health aid funders to adopt all available effective, safe and sustainable malaria control measures. “Malaria is devastating to many communities in Africa,” said Dr. Abou Thiam of PAN Africa, based in Dakar, Senegal. “To control this horrible disease African health officials must invest in safe solutions that are best for each community. Possibilities include environmental management, biological controls, correct use of bednets, preventative medication, effective treatment, community participation – and especially carefully chosen combinations of these methods and approaches. There is no magic bullet.” Holistic malaria control efforts have shown good results in Africa, Asia and Latin America. The network highlighted a new report by PAN Germany documenting successful community-based malaria control programs worldwide. “We have many successful malaria control projects in urban and rural areas in Kenya,” said Dr. Charles Mbogo of the International Center for Insect Physiology and Ecology in Kenya. “We have reduced rates of infection by up to 50% by raising awareness about malaria and involving the community in managing the environment to control mosquito populations. We also promote the use of bednets and in some cases apply environmentally safe larvicides.” Mexico has seen great successes with its national malaria control program that was designed to eliminate the country’s reliance on indoor spraying of the pesticide DDT, which has been slated for international phase-out under the Stockholm Convention on Persistent Organic Pollutants. -

African Letter on World Malaria
25 th April 2011 To: African Ministers of Health Dear Hon. Ministers, We the undersigned public health and environmental NGOs from Africa and elsewhere share a deep concern about the catastrophic public health tragedy that malaria represents for Africa and other regions. On the occasion of World Malaria Day on April 25, we urge you to conduct the fight against malaria using the most effective, least toxic, sustainable malaria control approaches. We urge you not to allow a handful of people with ulterior motives to derail this movement with false arguments manufactured to rehabilitate ineffective interventions which are harmful to human health — such as widespread spraying of the insecticide DDT i inside homes. Our groups fully support the approach to DDT outlined in the Stockholm Convention, which allows use only for malaria vector control in accordance with WHO guidelines, in countries where no locally safe, effective and affordable alternatives are currently available. The Convention emphasizes attention to alternatives that will allow for ultimate elimination of DDT. Through a process initiated by the Stockholm Convention- called the Global Alliance for Alternatives to DDT — the global community is moving towards finding safe effective ways to control malaria and phase out this dangerous toxic chemical. We urge you to support this process. Over the past few years there has been an increase in misinformed calls for using toxic- and ultimately ineffective strategies for malaria control such as Indoor Residual Spraying with the insecticide DDT. A barrage of misinformation and falsehoods is being spread by a few advocates of DDT, whose concern for malaria control is questionable and their larger goal seems to be to undermine the global processes moving towards finding alternatives to this toxic insecticide. -

MALARIA Pharmacy Department, Hospital Segamat
Bulletin Pharmacy 2/2015 MALARIA Pharmacy Department, Hospital Segamat INTRODUCTION [1] Malaria is caused by a parasite called Plasmodium, which Editorial Board: is transmitted via the bites of infected Anopheles mosqui- Advisor: toes, called "malaria vectors", which bite mainly between dusk and dawn. In the human body, the parasites multiply in the liver, and then infect Pn Siti Asmah Basimin red blood cells. Editor: Symptoms of malaria include fever, headache, and vomiting, and usually appear between Miss Yee Chiou Yann 10 and 15 days after the mosquito bite. If not treated, malaria can quickly become life- Co-editor: threatening by disrupting the blood supply to vital organs. In many parts of the world, Lim Xin Ru the parasites have developed resistance to a number of malaria medicines. Lawrence Lim Hsien Sheng Fairuz Binti Mu- [1,2] hammad Fakha- KEY FACTS ruddin According to the latest estimates, released in December 2014, there were about 198 million cases of malaria in 2013 (with an Nur Syafiqah Binti Anuar uncertainty range of 124 million to 283 million) and an estimated 584 000 deaths (with an uncertainty range of 367 000 to 755 000). Inside this issue: Malaria mortality rates have fallen by 47% globally since 2000, and by 54% in the Introduction 1 WHO African Region. Key Facts 1 Symptoms 2 Most deaths occur among children living in Africa where a child dies every minute Who is at risk? 2 from malaria. Malaria mortality rates among children in Africa have been reduced by Diagnosis 3 an estimated 58% since 2000. Treatment 3-5 Malaria is preventable and curable. -

Malaria Elimination in China, Evolution and Challenges with Respect to Cross Border Transmission Shaosen Zhang
Malaria elimination in China, evolution and challenges with respect to cross border transmission Shaosen Zhang To cite this version: Shaosen Zhang. Malaria elimination in China, evolution and challenges with respect to cross bor- der transmission. Human health and pathology. Université Montpellier, 2019. English. NNT : 2019MONTT027. tel-02464817 HAL Id: tel-02464817 https://tel.archives-ouvertes.fr/tel-02464817 Submitted on 3 Feb 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. THÈSE POUR OBTENIR LE GRADE DE DOCTEUR DE L’UNIVERSITÉ DE MONTPELLIER Spécialité : Biologie Santé École doctorale Sciences Chimiques et Biologiques pour la Santé (CBS2) Unité de recherches HSM-HydroSciences Montpellier (UMR 5569 IRD-CNRS-UM) et Intertryp (UMR 17 CIRAD-IRD) Elimination du paludisme en Chine, évolution et défis de la transmission transfrontalière Présentée par Shaosen ZHANG Soutenue le 21/11/2019 devant le jury composé de Mme. Evelyne Ollivier, Professeur à l’Université Aix-Marseille Rapporteur M. Theeraphap Chareonviriyaphap, Professeur à l’Université Kasetsart Rapporteur M. Emmanuel Cornillot, Professeur à l’Université de Montpellier Examinateur M. Shuisen Zhou, Professeur au National Institute of Parasitic Diseases Examinateur Mme Sylvie Manguin, Directrice de Recherche à l’IRD Directrice de Thèse M. -

World Malaria Day 2020 Malaria: Status Update on Children 25 April 2020
WORLD MALARIA DAY 2020 MALARIA: STATUS UPDATE ON CHILDREN 25 APRIL 2020 THE OVERLAP OF COVID-19 AND MALARIA COULD HAVE POTENTIALLY HIGHLY LETHAL CONSEQUENCES FOR CHILDREN UNDER-FIVE IF WE DON’T RESPOND SOON TO ENSURE CONTINUITY OF SERVICES © UNICEF/UN0318098/Frank Dejongh Every two minutes, a child under the age of five dies • Over the past two decades, substantial work has been done to from malaria. According to the 2019 World Malaria Report, dramatically control malaria by ministries of health, national children under five accounted for 67 percent of all malaria deaths malaria control programs, district health offices, health facilities worldwide in 2018. Most of these over 272,000 deaths occurred in and community health workers. However, despite major gains, sub-Saharan Africa where approximately 24 million children were even before the onset of COVID-19, sub-Saharan African estimated to be infected with the deadliest form of malaria. In addition countries were already falling short of the global target of to being the third highest infectious disease killer of children, malaria universal use of insecticide treated mosquito nets. Sleeping infection and the costs of treatment traps families in a cycle of illness, under insecticide-treated mosquito nets (ITNs) on a regular basis suffering and poverty1. is one of the most effective ways to prevent malaria transmission and reduce malaria related deaths. Consistent use of an effective The primary focus of UNICEF’s malaria efforts is to reduce the number insecticide-treated net – particularly one that is long-lasting - by at of children’s lives lost to the disease to zero. -

Efficacy of Seasonal Intermittent Preventive Treatment With
EFFICACY OF SEASONAL INTERMITTENT PREVENTIVE TREATMENT WITH SULPHADOXINE-PYRIMETHAMINE ON REDUCTION OF CLINICAL MALARIA AND ANAEMIA IN UNDER FIVE CHILDREN PRESENTING IN SEVENTH-DAY ADVENTIST HOSPITAL, JENGRE, PLATEAU STATE. A DISSERTATION SUBMITTED TO NATIONAL POSTGRADUATE MEDICAL COLLEGE OF NIGERIA (NPMCN) IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE AWARD OF FELLOWSHIP OF THE COLLEGE IN FAMILY MEDICINE (FMCFM) BY DR. EVEREST KEMAS (MBBS, UNIVERSITY OF JOS, 2006) DEPARTMENT OF FAMILY MEDICINE, JOS UNIVERSITY TEACHING HOSPITAL, JOS, NIGERIA. MAY 2016. 1 DECLARATION I, Dr EVEREST KEMAS, hereby declare that this research work is original and that no part or whole work has been submitted to another examination body for Fellowship. Also that this work has not been submitted to any journal for publication. ___________________________________________ DR. EVEREST KEMAS DATE: ___________________________________ 2 DEDICATION This work is dedicated to GOD Almighty and to all under five children affected by malaria in Nigeria and in Africa. 3 ACKNOWLEDGEMENT I am eternally indebted to my supervisors Drs. Pitmang and Lar for painstakingly guiding me through this part of my training and investing their time and knowledge to make me what I am today.I am also grateful to Drs. Agaba and Isandu for reading through my script and for their most valued criticisms and encouragement that spurred me on. To late Dr Dawam for providing me with materials that helped me in the course of writing this book. To my entire family and friends, their support has been vital for me to accomplish this project. To Mr Chris, the Laboratory technician for assisting me in analyzing my samples.