Cerebral Folate Deficiency: Analytical Tests and Differential Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Folate Receptor Alpha Defect Causes Cerebral Folate Transport Deficiency: a Treatable Neurodegenerative Disorder Associated with Disturbed Myelin Metabolism
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector ARTICLE Folate Receptor Alpha Defect Causes Cerebral Folate Transport Deficiency: A Treatable Neurodegenerative Disorder Associated with Disturbed Myelin Metabolism Robert Steinfeld,1,5,* Marcel Grapp,1,5 Ralph Kraetzner,1 Steffi Dreha-Kulaczewski,1 Gunther Helms,2 Peter Dechent,2 Ron Wevers,3 Salvatore Grosso,4 and Jutta Ga¨rtner1 Sufficient folate supplementation is essential for a multitude of biological processes and diverse organ systems. At least five distinct in- herited disorders of folate transport and metabolism are presently known, all of which cause systemic folate deficiency. We identified an inherited brain-specific folate transport defect that is caused by mutations in the folate receptor 1 (FOLR1) gene coding for folate receptor alpha (FRa). Three patients carrying FOLR1 mutations developed progressive movement disturbance, psychomotor decline, and epilepsy and showed severely reduced folate concentrations in the cerebrospinal fluid (CSF). Brain magnetic resonance imaging (MRI) demon- strated profound hypomyelination, and MR-based in vivo metabolite analysis indicated a combined depletion of white-matter choline and inositol. Retroviral transfection of patient cells with either FRa or FRb could rescue folate binding. Furthermore, CSF folate concen- trations, as well as glial choline and inositol depletion, were restored by folinic acid therapy and preceded clinical improvements. Our studies not only characterize -

B Vitamin Polymorphisms and Behavior: Evidence of Associations
G Model NBR 2010 1–14 ARTICLE IN PRESS Neuroscience and Biobehavioral Reviews xxx (2014) xxx–xxx Contents lists available at ScienceDirect Neuroscience and Biobehavioral Reviews jou rnal homepage: www.elsevier.com/locate/neubiorev 1 Review 2 B vitamin polymorphisms and behavior: Evidence of associations 3 with neurodevelopment, depression, schizophrenia, bipolar disorder 4 and cognitive decline ∗ 5 Q1 E. Siobhan Mitchell , Nelly Conus, Jim Kaput 6 Nestle Institute of Health Science, Innovation Park, EPFL Campus, Lausanne 1015, Switzerland 7 298 a r t i c l e i n f o a b s t r a c t 9 10 Article history: The B vitamins folic acid, vitamin B12 and B6 are essential for neuronal function, and severe deficiencies 11 Received 16 December 2013 have been linked to increased risk of neurodevelopmental disorders, psychiatric disease and dementia. 12 Received in revised form 11 July 2014 Polymorphisms of genes involved in B vitamin absorption, metabolism and function, such as methylene 13 Accepted 18 August 2014 tetrahydrofolate reductase (MTHFR), cystathionine  synthase (CS), transcobalamin 2 receptor (TCN2) 14 Available online xxx and methionine synthase reductase (MTRR), have also been linked to increased incidence of psychiatric 15 and cognitive disorders. However, the effects of these polymorphisms are often quite small and many 16 Keywords: studies failed to show any meaningful or consistent associations. This review discusses previous findings 17 Folate from clinical studies and highlights gaps in knowledge. Future studies assessing B vitamin-associated 18 Vitamin B9 polymorphisms must take into account not just traditional demographics, but subjects’ overall diet, 19 Vitamin B12 20 Vitamin B6 relevant biomarkers of nutritional status and also analyze related genetic factors that may exacerbate 21 Dementia behavioral effects or nutritional status. -

(FOLR1) Mrna Expression, Its Specific Promoter
Notaro et al. BMC Cancer (2016) 16:589 DOI 10.1186/s12885-016-2637-y RESEARCH ARTICLE Open Access Evaluation of folate receptor 1 (FOLR1) mRNA expression, its specific promoter methylation and global DNA hypomethylation in type I and type II ovarian cancers Sara Notaro1,2, Daniel Reimer1, Heidi Fiegl1, Gabriel Schmid1, Annamarie Wiedemair1, Julia Rössler1, Christian Marth1 and Alain Gustave Zeimet1* Abstract Background: In this retrospective study we evaluated the respective correlations and clinical relevance of FOLR1 mRNA expression, FOLR1 promoter specific methylation and global DNA hypomethylation in type I and type II ovarian cancer. Methods: Two hundred fifty four ovarian cancers, 13 borderline tumours and 60 samples of healthy fallopian epithelium and normal ovarian epithelium were retrospectively analysed for FOLR1 expression with RT-PCR. FOLR1 DNA promoter methylation and global DNA hypomethylation (measured by means of LINE1 DNA hypomethylation) were evaluated with MethyLight technique. Results: No correlation between FOLR1 mRNA expression and its specific promoter DNA methylation was found neither in type I nor in type II cancers, however, high FOLR1 mRNA expression was found to be correlated with global DNA hypomethylation in type II cancers (p = 0.033). Strong FOLR1 mRNA expression was revealed for Grades 2-3, FIGO stages III-IV, residual disease > 0, and serous histotype. High FOLR1 expression was found to predict increased platinum sensitivity in type I cancers (odds ratio = 3.288; 1.256-10.75; p = 0.020). One-year survival analysis showed in type I cancers an independent better outcome for strong expression of FOLR1 in FIGO stage III and IV. -

Novel Anti-FOLR1 Antibody–Drug Conjugate Morab-202 in Breast Cancer and Non-Small Cell Lung Cancer Cells
antibodies Article Novel Anti-FOLR1 Antibody–Drug Conjugate MORAb-202 in Breast Cancer and Non-Small Cell Lung Cancer Cells Yuki Matsunaga 1, Toshimitsu Yamaoka 2,* , Motoi Ohba 2, Sakiko Miura 3, Hiroko Masuda 1, Takafumi Sangai 4 , Masafumi Takimoto 3, Seigo Nakamura 1 and Junji Tsurutani 2 1 Department of Breast Surgical Oncology, School of Medicine, Showa University, 1-5-8 Hatanodai, Shinagawa-ku, Tokyo 142-8666, Japan; [email protected] (Y.M.); [email protected] (H.M.); [email protected] (S.N.) 2 Advanced Cancer Translational Research Institute, Showa University, 1-5-8 Hatanodai, Shinagawa-ku, Tokyo 142-8555, Japan; [email protected] (M.O.); [email protected] (J.T.) 3 Department of Pathology, School of Medicine, Showa University, Tokyo 142-8666, Japan; [email protected] (S.M.); [email protected] (M.T.) 4 Department of Breast and Thyroid Surgery, School of Medicine, Kitasato University, Kanagawa 252-0375, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-3-3784-8146 Abstract: Antibody–drug conjugates (ADCs), which are currently being developed, may become promising cancer therapeutics. Folate receptor α (FOLR1), a glycosylphosphatidylinositol-anchored membrane protein, is an attractive target of ADCs, as it is largely absent from normal tissues but is overexpressed in malignant tumors of epithelial origin, including ovarian, lung, and breast cancer. In this study, we tested the effects of novel anti-FOLR1 antibody–eribulin conjugate MORAb-202 in breast cancer and non-small cell lung cancer (NSCLC) cell lines. -

Photodynamic Therapy Using a New Folate Receptor-Targeted Photosensitizer on Peritoneal Ovarian Cancer Cells Induces the Release
Journal of Clinical Medicine Article Photodynamic Therapy Using a New Folate Receptor-Targeted Photosensitizer on Peritoneal Ovarian Cancer Cells Induces the Release of Extracellular Vesicles with Immunoactivating Properties 1, 1,2, 3 3 Martha Baydoun y, Olivier Moralès y ,Céline Frochot , Colombeau Ludovic , Bertrand Leroux 1, Elise Thecua 1 , Laurine Ziane 1, Anne Grabarz 1,4, Abhishek Kumar 1, 1 1,4 1,5 1, , Clémentine de Schutter , Pierre Collinet , Henri Azais , Serge Mordon * y and 1, , Nadira Delhem * y 1 Université de Lille, Faculté des Sciences et Technologies, INSERM, CHU-Lille, U1189-ONCO-THAI–Assisted Laser Therapy and Immunotherapy for Oncology, F-59000 Lille, France; [email protected] (M.B.); [email protected] (O.M.); [email protected] (B.L.); [email protected] (E.T.); [email protected] (L.Z.); [email protected] (A.G.); [email protected] (A.K.); [email protected] (C.d.S.); [email protected] (P.C.); [email protected] (H.A.) 2 CNRS UMS 3702, Institut de Biologie de Lille, 59 021 Lille, France 3 LGRGP, UMR-CNRS 7274, University of Lorraine, 54 001 Nancy, France; [email protected] (C.F.); [email protected] (C.L.) 4 Unité de Gynécologie-Obstétrique, Hôpital Jeanne de Flandre, 59 000 CHU Lille, France 5 Service de Chirurgie et Cancérologie Gynécologique et Mammaire, Hôpital de la Pitié-Salpêtrière, AP-HP, 75 013 Paris, France * Correspondence: [email protected] (S.M.); [email protected] (N.D.); Tel./Fax: +33-32044-6708 (S.M.); Tel.: +33-3208-71253/1251 (N.D.); Fax: +33-32087-1019 (N.D.) These authors contributed equally to this work. -

Detection of Folate Receptor from FR+ Cells Gopikrishna Pinnaka Governors State University
Governors State University OPUS Open Portal to University Scholarship All Capstone Projects Student Capstone Projects Spring 2012 Detection of Folate Receptor from FR+ Cells Gopikrishna Pinnaka Governors State University Follow this and additional works at: http://opus.govst.edu/capstones Part of the Analytical Chemistry Commons Recommended Citation Pinnaka, Gopikrishna, "Detection of Folate Receptor from FR+ Cells" (2012). All Capstone Projects. 11. http://opus.govst.edu/capstones/11 For more information about the academic degree, extended learning, and certificate programs of Governors State University, go to http://www.govst.edu/Academics/Degree_Programs_and_Certifications/ Visit the Governors State Analytical Chemistry Department This Project Summary is brought to you for free and open access by the Student Capstone Projects at OPUS Open Portal to University Scholarship. It has been accepted for inclusion in All Capstone Projects by an authorized administrator of OPUS Open Portal to University Scholarship. For more information, please contact [email protected]. Detection of Folate Receptor from FR+ Cells A Project Submitted To Governors State University By Gopikrishna Pinnaka In Partial Fulfillment of the Requirements for the Degree Of Masters in Science May 2012 Governors State University University Park, Illinois 1 Dedicated to My Parents, Wife & Friends 2 Acknowledgement: I would like to take this opportunity to offer my sincere thanks to each and every person for helping me to accomplish this task . This research project would not have been possible without the support of many people. I would like to express my gratitude thank to Dr. Walter Henne who was abundantly helpful and offered invaluable assistance, guidance and support throughout my project, without whose knowledge and assistance this study would not have been successful. -

CIC De Novo Loss of Function Variants Contribute to Cerebral Folate Deficiency by Downregulating FOLR1 Expression Xuanye Cao,1 Annika Wolf,2 Sung-Eun Kim,3 Robert M
Neurogenetics J Med Genet: first published as 10.1136/jmedgenet-2020-106987 on 20 August 2020. Downloaded from Original research CIC de novo loss of function variants contribute to cerebral folate deficiency by downregulating FOLR1 expression Xuanye Cao,1 Annika Wolf,2 Sung- Eun Kim,3 Robert M. Cabrera,1 Bogdan J. Wlodarczyk,1 Huiping Zhu,4 Margaret Parker,3 Ying Lin,1 John W. Steele,1,5 Xiao Han,1 Vincent Th Ramaekers ,6 Robert Steinfeld,2,7 Richard H. Finnell,3,8,9 Yunping Lei 1 2 ► Additional material is ABSTRact epilepsy, ataxia and pyramidal tract signs. Folate is published online only. To view Background Cerebral folate deficiency (CFD) absorbed into the bloodstream via the gastrointes- please visit the journal online (http:// dx. doi. org/ 10. 1136/ syndrome is characterised by a low concentration of tinal tract mainly through two uptake systems: the jmedgenet- 2020- 106987). 5- methyltetrahydrofolate in cerebrospinal fluid, while reduced folate carrier 1 (RFC1; SLC19A1) and the folate levels in plasma and red blood cells are in the low proton- coupled folate transporter (PCFT).3 From For numbered affiliations see normal range. Mutations in several folate pathway genes, the bloodstream, folate binds to the folate receptor end of article. including FOLR1 (folate receptor alpha, FRα), DHFR alpha (FRα/FOLR1) on the basolateral endothelial (dihydrofolate reductase) and PCFT (proton coupled surface of the choroid plexus. Through receptor- Correspondence to Dr. Yunping Lei, Baylor College folate transporter) have been previously identified in mediated endocytosis and transcytosis, folate is of Medicine, Houston, Texas, patients with CFD. then transported across the blood- CSF- barrier USA; yunpinglei@ gmail. -
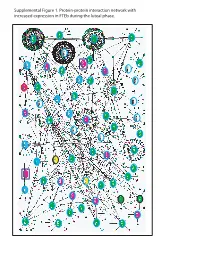
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

Figure S1. 17-Mer Distribution in the Yangtze Finless Porpoise Genome
Figure S1. 17-mer distribution in the Yangtze finless porpoise genome. The x-axis is 17-mer depth (X); the y-axis is the number of sequencing reads at that depth. Figure S2. Sequence depth distribution of the assembly data. The x-axis shows the sequencing depth (X) and the y-axis shows the number of bases at a given depth. The results demonstrate that 99% of bases sequencing depth is more than 20. Figure S3. Comparison of gene structure characteristics of Yangtze finless porpoise and other cetaceans. The x-axis represents the length of corresponding genetic element of exon number and the y-axis represents gene density. Figure S4. Phylogeny relationships between the Yangtze finless porpoise and other mammals reconstructed by RAxML with the GTR+G+I model. Table S1. Summary of sequenced reads Raw Reads Qualified Reads1 Total Read Sequence Physical Total Read Sequence Physical Library SRA Data Length Coverage2 Coverage2 Data Length Coverage2 Coverage2 Insert Size (bp) Number (Gb) (bp) (×) (×) (Gb) (bp) (×) (×) 289 58.94 150.00 23.67 22.80 57.84 149.75 23.23 22.41 SRR6923836 462 71.33 150.00 28.65 44.12 70.12 149.74 28.16 43.44 SRR6923837 624 67.47 150.00 27.10 56.36 63.90 149.67 25.66 53.50 SRR6923834 791 57.58 150.00 23.12 60.97 55.39 149.67 22.24 58.78 SRR6923835 4,000 108.73 150.00 43.67 582.22 70.74 150.00 28.41 378.80 SRR6923832 7,000 115.4 150.00 46.35 1,081.39 84.76 150.00 34.04 794.27 SRR6923833 11,000 107.37 150.00 43.12 1,581.08 79.78 150.00 32.04 1,174.81 SRR6923830 18,000 127.46 150.00 51.19 3,071.33 97.75 150.00 39.26 2,355.42 SRR6923831 Total 714.28 - 286.87 6,500.27 580.28 - 233.04 4,881.43 - 1Raw reads in mate-paired libraries were filtered to remove duplicates and reads with low quality and/or adapter contamination, raw reads in paired-end libraries were filtered in the same manner then subjected to k-mer-based correction. -

Immunotherapy Targeting Folate Receptor Induces Cell Death Associated with Autophagy in Ovarian Cancer Yunfei Wen1, Whitney S
Published OnlineFirst November 21, 2014; DOI: 10.1158/1078-0432.CCR-14-1578 Cancer Therapy: Preclinical Clinical Cancer Research Immunotherapy Targeting Folate Receptor Induces Cell Death Associated with Autophagy in Ovarian Cancer Yunfei Wen1, Whitney S. Graybill2, Rebecca A. Previs1,WeiHu1, Cristina Ivan3, Lingegowda S. Mangala1, Behrouz Zand1, Alpa M. Nick1, Nicholas B. Jennings1, Heather J. Dalton1, Vasudha Sehgal4, Prahlad Ram4, Ju-Seog Lee5, Pablo E. Vivas-Mejia6, Robert L. Coleman1, and Anil K. Sood1,3,7 Abstract Purpose: Cancer cells are highly dependent on folate metab- the low-FRa A2780 model. MORAB-003 reduced prolifera- olism, making them susceptible to drugs that inhibit folate tion,buthadnosignificant effect on apoptosis. Protein receptor activities. Targeting overexpressed folate receptor alpha expression and cDNA microarray analyses showed that (FRa) in cancer cells offers a therapeutic opportunity. We inves- MORAB-003 regulated an array of autophagy-related genes. tigated the functional mechanisms of MORAB-003 (farletuzu- It also significantly increased expression of LC3 isoform II and mab), a humanized mAb against FRa, in ovarian cancer models. enriched autophagic vacuolization. Blocking autophagy with Experimental Design: We first examined FRa expression in an hydroxychloroquine or bafilomycin A1 reversed the growth array of human ovarian cancer cell lines and then assessed the in inhibition induced by MORAB-003. In addition, alteration vivo effect of MORAB-003 on tumor growth and progression in of FOLR1 gene copy number significantly correlated with several orthotopic mouse models of ovarian cancer derived from shorter disease-free survival in patients with ovarian serous these cell lines. Molecular mechanisms of tumor cell death induced cancer. -

Folate Receptor-Α Expression in Resectable Hepatic Colorectal Cancer Metastases
Modern Pathology (2011) 24, 1221–1228 & 2011 USCAP, Inc. All rights reserved 0893-3952/11 $32.00 1221 Folate receptor-a expression in resectable hepatic colorectal cancer metastases: patterns and significance Michael D’Angelica1, John Ammori1, Mithat Gonen2, David S Klimstra3, Philip S Low4, Linda Murphy5, Martin R Weiser1, Philip B Paty1, Yuman Fong1, Ronald P DeMatteo1, Peter Allen1, William R Jarnagin1 and Jinru Shia3 1Department of Surgery, Memorial Sloan-Kettering Cancer Center, New York, NY, USA; 2Department of Biostatistics, Memorial Sloan-Kettering Cancer Center, New York, NY, USA; 3Department of Pathology, Memorial Sloan-Kettering Cancer Center, New York, NY, USA; 4Department of Chemistry and Weldon School of Biomedical Engineering, Purdue University, West Lafayette, IN, USA and 5Department of Biochemistry and Molecular Biology, Mayo Clinic College of Medicine, Rochester, MN, USA Folate receptor alpha (FRa), encoded by folate receptor 1 (adult) gene, has emerged as a cancer biomarker and potential therapeutic target. In addition, its expression in tumors may offer prognostic information. The aim of this study was to assess the prognostic value of FRa expression and other common molecular markers in resected liver metastases from colorectal cancer. To maximize potential biological differences, we selected two groups of patients with markedly different outcomes as study subjects. Immunohistochemical analysis of FRa expression and other common markers (thymidylate synthase, p53, p27, BCL2, ki67, MLH1, MSH2 and MGMT) on tissue microarrays was carried out on samples from 160 patients; 56 patients survived at least 10 years following liver resection, and 104 died within 2 years of surgery. These markers were evaluated and compared with standard clinical predictors of outcome including a previously validated clinical risk score. -
Characterization and Use of Folate Receptor Isoforms for Targeting of Epithelial and Myeloid Cells Sreya Biswas University of Wisconsin-Milwaukee
University of Wisconsin Milwaukee UWM Digital Commons Theses and Dissertations December 2016 Characterization and Use of Folate Receptor Isoforms for Targeting of Epithelial and Myeloid Cells Sreya Biswas University of Wisconsin-Milwaukee Follow this and additional works at: https://dc.uwm.edu/etd Part of the Biology Commons, and the Molecular Biology Commons Recommended Citation Biswas, Sreya, "Characterization and Use of Folate Receptor Isoforms for Targeting of Epithelial and Myeloid Cells" (2016). Theses and Dissertations. 1352. https://dc.uwm.edu/etd/1352 This Dissertation is brought to you for free and open access by UWM Digital Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UWM Digital Commons. For more information, please contact [email protected]. CHARACTERIZATION AND USE OF FOLATE RECEPTOR ISOFORMS FOR TARGETING OF EPITHELIAL AND MYELOID CELLS by Sreya Biswas A Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Biological Sciences at The University of Wisconsin-Milwaukee December 2016 ABSTRACT CHARACTERIZATION AND USE OF FOLATE RECEPTOR ISOFORMS FOR TARGETING OF EPITHELIAL AND MYELOID CELLS by Sreya Biswas The University of Wisconsin-Milwaukee, 2016 Under the Supervision of Professor Douglas A. Steeber Folate receptor (FR) is a GPI-anchored glycoprotein with high binding affinity for folic acid. FR has two membrane-associated isoforms, α and β, that are overexpressed on epithelial and myeloid tumors, respectively. Normal cells may also exhibit FR expression at very low levels but interestingly, FR-α on normal cells is restricted to the apical surface i.e., away from the blood stream.