Regional Breastfeeding Services Directory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Careflight Air and Mobile Services Adds Fourth Aircraft Base in Darke
Miami Valley Hospital Nonprofi t Organization IN THIS ISSUE CareFlight Air and Mobile Services U.S. Postage Paid One Wyoming St. Dayton, OH 45409 Dayton, OH 45409 Permit Number 79 CareFlight Adds Aircraft Base ADDRESS SERVICE REQUESTED New Mobile Intensive Care Units COVID-19 Mitigation Risk CareFlight Air and Mobile App CareFlight Reunion Distance Learning CareFlight Air and Mobile Services FALL 2020 CareFlight Air and Mobile Services Brings New MICUs On Board By Jennifer Schueler, MSN, APRN, NREMT-P, CEN, Flight Nurse TOLEDO 2 CLEVELAND March 2020 brought many changes to our world time around, allowing each MICU to be placed into 7 that will undoubtedly remain etched into our service in early March. 71 memories. While the COVID-19 pandemic within Aside from ODPS inspection, the MICU also had to 11 the United States was just starting to ramp up, meet all24 standards set forth by the Commission of the CareFlight Air and Mobile Services quietly focused 20 33 Accreditation of Medical Transport Systems (CAMTS).23 on acquiring new Mobile Intensive Care Unit The accrediting body of CAMTS is dedicated to 18 Miami Valley Hospital (MICU) vehicles. ensuring that each patient will receive quality and 250 One Wyoming Street CareFlight Air and Mobile Services Adds American Medical Response (AMR) is the ground safe care within the transport environment no Distance Learning (continued) Dayton, Ohio 45409 medical transportation division of Global469 Medical matter if transported by air or a critical care ground 224 CareFlight Fourth Aircraft Base in Darke County 15 (800) 251-2273 Response (GMR) and serves as the vendor for the unit. -

Miami Valley Hospital
MIAMI VALLEY HOSPITAL HEART AND ORTHOPEDIC CENTER DAYTON, OHIO MIAMI VALLEY HOSPITAL A NEW CHAPTER HEART AND ORTHOPEDIC CENTER ON EFFICIENCY Dayton, Ohio Using Lean design principles and Lean construction methods, the new Center challenges the assumption that there must be a trade-off between time, cost and quality. CLIENT VISION DESIGN BREAKTHROUGH ORGANIZATIONAL VALUE SPRINGBOARD INSIGHT As demand at Southwest Ohio’s busiest cardiac care center NBBJ drew on experience from vastly different building The use of Building Information Modeling (BIM) to test When the facility and delivery process are designed together, continued to grow, Miami Valley Hospital sought to increase types to drive innovative solutions. For example, the patient new ideas for patient experience and a Lean construction they better reveal and support client goals. capacity and consolidate operations into a single state-of-the-art floor design took a page from corporate offices with a approach resulted in a savings of over $1 million and a two- facility. The transformation would redefine the patient experience, double-loaded corridor and modular, centralized caregiver month reduction in schedule. Applied research on patient embrace advanced methods of care, and position the hospital stations. This resulted in reduced travel times and increased room configurations reduced patient transfers by 66%, and as an accessible and engaging community landmark. visibility into the rooms. increased the time clinicians are able to spend with patients. Main Entry Patient Resource Center Information Desk Main Entry and Information Desk Concourse Cafe A WELCOMING Patient Resource Center GESTURE As Dayton’s busiest cardiac care center, Miami Valley Hospital The tower addition is designed with a flexible and clear The existing central courtyard which had been congested struggled to deliver advanced care in three 1970s-era facilities. -

Trauma Centers
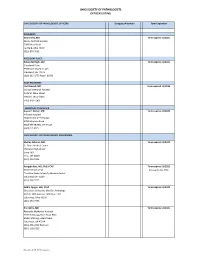
Updated: 5/5/2021 TRAUMA CENTERS Location Level EMS Adult Pediatric HOSPITAL CITY COUNTY Status Expires Visit Date Region Level Level Akron Children's Hospital Akron Summit 5 ACS 9/10/2022 2 Atrium Medical Center Franklin Butler 6 ACS 11/6/2022 3 Aultman Hospital Canton Stark 5 ACS 10/24/2021 6/4/2021 V 2 Bethesda North Cincinnati Hamilton 6 ACS 6/9/2022 3 Blanchard Valley Hospital Findlay Hancock 1 ACS 1/15/2024 3 Cincinnati Children's Hospital Medical Center Cincinnati Hamilton 6 ACS 1/23/2022 1 Cleveland Clinic Akron General Akron Summit 5 ACS 4/17/2022 1 Cleveland Clinic Fairview Hospital Cleveland Cuyahoga 2 ACS 3/9/2022 2 Cleveland Clinic Hillcrest Hospital Mayfield Heights Cuyahoga 2 ACS 12/9/2021 2 Dayton Children's Hospital Dayton Montgomery 3 ACS 2/12/2024 1 Firelands Regional Medical Center Sandusky Erie 1 ACS 2/23/2023 3 Fisher-Titus Medical Center Norwalk Huron 1 ACS 11/23/2022 3 Genesis HealthCare System Zanesville Muskingum 8 ACS 10/6/2024 3 Grandview Medical Center Dayton Montgomery 3 ACS 10/26/2022 3 Kettering Health Network Fort Hamilton Hospital Hamilton Butler 6 Ohio-18 8/24/2022 *3* Kettering Health Network Soin Medical Center Beavercreek Greene 3 ACS 11/13/2023 3 Kettering Medical Center Kettering Montgomery 3 ACS 1/11/2023 2 Lima Memorial Hospital Lima Allen 1 ACS 5/13/2021 5/4-5/2021 V 2 Marietta Memorial Hospital Marietta Washington 8 ACS 11/20/2022 3 Mercy Health St. Charles Hospital Toledo Lucas 1 ACS 12/8/2022 3 Mercy Health St. -

Allen Ashland Ashtabula Athens Auglaize Belmont Butler Clark Clinton Columbiana Crawford Cuyahoga Darke Defiance Delaware Erie F
Central Paternity Registry | Birthing Facilities Directory ALLEN CLARK PROMEDICA DEFIANCE REGIONAL BLANCHARD VALLEY HOSPITAL – SPRINGFIELD REGIONAL MEDICAL CENTER BLUFFTON CAMPUS MEDICAL CENTER 1200 RALSTON AVENUE 139 GARAU STREET 100 MEDICAL CENTER DRIVE DEFIANCE, OH 43512 BLUFFTON, OH 45817 SPRINGFIELD, OH 45504 DELAWARE LIMA MEMORIAL HOSPITAL CLINTON GRADY MEMORIAL HOSPITAL 1001 BELLEFONTAINE AVENUE CLINTON MEMORIAL HOSPITAL 561 WEST CENTRAL AVENUE LIMA, OH 45804 610 WEST MAIN STREET DELAWARE, OH 43015 WILMINGTON, OH 45177 ST RITA'S MEDICAL CENTER ERIE 730 WEST MARKET STREET COLUMBIANA FIRELANDS COMMUNITY HOSPITAL LIMA, OH 45801 1101 DECATUR ST SALEM REGIONAL MEDICAL CENTER 1995 EAST STATE STREET SANDUSKY, OH 44870 ASHLAND SALEM, OH 44460 UNIVERSITY HOSPITALS FAIRFIELD SAMARITAN MEDICAL CENTER FAIRFIELD MEDICAL CENTER 1025 CENTER STREET CRAWFORD GALION COMMUNITY HOSPITAL 401 NORTH EWING STREET ASHLAND, OH 44805 LANCASTER,OH 43130 269 PORTLAND WAY SOUTH GALION, OH 44833 ASHTABULA FRANKLIN ASHTABULA COUNTY CUYAHOGA DOCTORS HOSPITAL WEST MEDICAL CENTER 5100 WEST BROAD STREET 2420 LAKE AVENUE FAIRVIEW HEALTH SYSTEM 18101 LORAIN AVENUE COLUMBUS, OH 43228 ASHTABULA, OH 44004 CLEVELAND, OH 44111 DUBLIN METHODIST HOSPITAL ATHENS MERIDIA HILLCREST HOSPITAL 7500 HOSPITAL DRIVE O'BLENESS MEMORIAL HOSPITAL 6780 MAYFIELD ROAD DUBLIN, OH 43016 55 HOSPITAL DRIVE MAYFIELD HEIGHTS, OH 44124 ATHENS, OH 45701 GRANT MEDICAL CENTER METROHEALTH MEDICAL CENTER 111 SOUTH GRANT AVENUE AUGLAIZE 2500 METROHEALTH DRIVE COLUMBUS, OH 43215 ST MARY'S JOINT TOWNSHIP CLEVELAND, OH 44109 DISTRICT MOUNT CARMEL EAST MEMORIAL HOSPITAL SOUTHWEST GENERAL 6001 EAST BROAD STREET 200 ST. CLAIR STREET HEALTH CENTER COLUMBUS, OH 43213 SAINT MARYS, OH 45885 18697 BAGLEY ROAD MIDDLEBURG HEIGHTS, OH 44130 OHIO STATE UNIVERSITY MEDICAL BELMONT CENTER ST. -

1 CURRICULUM VITAE Mary C. Mccarthy, M.D., FACS Academic Address: Department of Surgery Boonshoft School of Medicine Wright
CURRICULUM VITAE Mary C. McCarthy, M.D., FACS Academic Address: Department of Surgery Boonshoft School of Medicine Wright State University One Wyoming St., Suite 7800 Dayton, Ohio 45409 937-208-3771 Fax 937-208-6231 [email protected] Present Academic Rank: Elizabeth Berry Gray Chair and Professor, Department of Surgery EDUCATION University of Texas Southwestern Medical School & Affiliated Hospitals, Dallas, TX, General Surgery Internship and Residency 1977-1983 Indiana University School of Medicine, Indianapolis, Indiana, M.D. 1973-1977 Stanford University, Stanford, California, B.S. Biology 1969-1973 ACADEMIC APPOINTMENTS Wright State University Boonshoft School of Medicine Elizabeth Berry Gray Chair and Professor, 04/13/2010-current Associate Professor of Surgery, 1/1/91-6/30/94 Professor of Surgery, 7/1/94-current School of Nursing Associate Graduate Faculty Membership, 7/93-6/98 School of Engineering Adjunct Graduate Faculty 7/2012-6/2017 Indiana University School of Medicine Assistant Professor of Surgery, 7/1/83-12/1/88 Clinical Assistant Professor of Surgery, 12/1/88-6/30/89 Clinical Associate Professor of Surgery, 7/1/89-12/31/90 Hospital Appointments Miami Valley Hospital 1991-current Indiana University Hospitals 1983-90 Wishard Memorial Hospital 1983-90, Trauma Director 1983-90 BOARD CERTIFICATION American Board of Surgery, Certificate in Surgery, April 11, 1984 (#29564) – Recertification: October 23, 1992, October 18, 2002, December 3, 2013, expiration December 31, 2024. American Board of Surgery, Certificate in Surgical -

Premier Health Launches Mass Vaccination Drive-Through Clinic at UD Arena Clinic Limited to Ohioans Age 80 and Older, in Keeping with State Guidance
Media Contact: Ben Sutherly (937) 524-3264 [email protected] Premier Health Launches Mass Vaccination Drive-Through Clinic at UD Arena Clinic Limited to Ohioans Age 80 and Older, In Keeping With State Guidance DAYTON, Ohio (January 20, 2021) – Thousands of Ohioans age 80 and older starting today can schedule their first dose of the two-dose COVID-19 vaccine through a mass drive-through vaccination clinic (operated by Miami Valley Hospital) at UD Arena. The drive-through clinic is by appointment only; no unscheduled vaccinations will be given. Premier Health will be vaccinating more than 5,000 eligible Ohioans (age 80 and older) within the next week. This includes 1,100 Ohioans who scheduled vaccines late last week and are receiving them this week, as well as nearly 4,000 Ohioans who will be vaccinated between this afternoon and Saturday at UD Arena. The mass vaccination clinic at UD Arena will run between 2 pm and 4 pm today, and from 8:30 am to 5:30 pm this Thursday through Saturday. Additional clinics might be scheduled depending on the receipt of additional vaccine from the State of Ohio. To schedule a vaccine, while supplies last, Ohioans 80 and older can: Visit www.premierhealth.com/vaccine, view appointment times that are available, and self- schedule their vaccinations; Call (937) 276-4141 between 8:30 a.m. and 5 p.m. seven days a week (due to high call volumes, we recommend that you schedule your vaccine online, if possible) In addition to the previous two options, eligible Premier Health patients can schedule an appointment through MyChart. -

First Steps for Healthy Babies – Bag Free
First Steps for Healthy Babies – Bag Free Maternity Care Best Practice Award 2017 - Recognized Hospitals The Ohio Hospital Association, Ohio Department of Health, Ohio Lactation Consultant Association, and Ohio Breastfeeding Alliance are pleased to announce that the following hospitals have achieved recognition as being a "Bag Free" facility in 2017: • Adena Regional Medical Center • OhioHealth Doctor's Hospital • Atrium Medical Center • OhioHealth Dublin Methodist Hospital • Aultman Orrville Hospital • OhioHealth Grady Memorial Hospital • Berger Health System • OhioHealth Grant Medical Center • Cleveland Clinic Akron General Medical • OhioHealth Mansfield Hospital Center • OhioHealth Marion General Hospital • Cleveland Clinic Fairview Hospital • OhioHealth Riverside Methodist Hospital • Cleveland Clinic Hillcrest Hospital • OhioHealth Shelby Hospital • Clinton Memorial Hospital • The Ohio State University Wexner Medical • Community Hospitals & Wellness Centers - Center Bryan Hospital • ProMedica Bay Park Hospital • Fairfield Medical Center • ProMedica Defiance Regional Hospital • Firelands Regional Medical Center • ProMedica Flower Hospital • Fisher-Titus Medical Center • ProMedica Memorial Hospital • Fulton County Health Center • ProMedica Toledo Hospital • Galion Community Hospital • Southern Ohio Medical Center • Genesis Hospital • Southview Medical Center • Good Samaritan Hospital - Dayton • Southwest General Health Center • Henry County Hospital • St. Elizabeth Boardman Hospital • Holzer Gallipolis • St. Joseph Warren Hospital • -

2016 Annual Report • Miami Valley Hospital Foundation
Annual Report 2016 Board of Trustees Chris G. Pulos, Chair Kim Belcastro, Vice Chair Jessica Barry Robert H. Brethen Michael W. Craig, MD Charles L. Ellington II Fr. Mark Emroll John L. Green Denise Hale Nicole M. Luisi Elaine T. Mattox Donna Milam 3 ••• Philanthropy and Volunteerism at MVH Miguel A. Parilo, MD, FACP Table of Contents Ann Reynolds 4 ••• 2016 Disbursements and Contributions Gregory A. Robinson Robert Siebenthaler 5 ••• The Hospital Elder Life Program: HELP Emeritus Members Edward J. Blake 6 ••• Promise to Hope Combines Community Support Richard C. Cammerer, MD Richard F. Carlile 8 ••• Employees Assist Campus Police Officer Kathleen A. Carlson Deanna J. Chapman, DPM 9 ••• Legacy Giving Profile: Mikki Clancy Parviz Daneshjoo, MD Richard P. Davis 10 ••• The Book-Fairy Godmother of Abby’s Nook Matthew O. Diggs, Jr. Jeanne N. Eickman Michael J. Emoff 11 ••• Brethen Center Offers New Technology Joseph Gordon Ken Herr 12 ••• Patients and Physicians Benefitting from MD Macy P. Janney Rodney W. Kennedy, Ph.D. Anderson Susan M. Lipowicz Jack Lohbeck 14 ••• Paying It Forward: Dave and Janet Merrelli John M. Manier Randy Marriott, MD 15 ••• Renovation Helps Attract New Physicians Mary B. McIntosh CRPC, CDFA Vail K. Miller Shirley A. Murphy 16 ••• Thank You to Our Donors! David L. Neer Robert W. Nutter 30 ••• Businesses, Organizations and Foundations Ratna K. Palakodeti, MD Laura B. Pannier 31 ••• Estates and Trusts James R. Payne Sara E. Rich Lois H. Ross William K. Rundell, MD R. Daniel Sadlier William J. Schneider Norman J. Schneiderman, MD Enhance the patient and family experience at Miami Wendy B. -

Premier Pulse
Premier Pulse News for Premier Health Physicians VOLUME 4 | ISSUE 10 | OCTOBER 2017 New Ohio Opioid Prescribing Rules Unveiled By Tammy Lundstrom, MD, JD, interim chief clinical officer and interim president, Premier Physician Network, Premier Health The Ohio Board of a prescription for acute pain cannot or CPT code to the prescription when of Medicine has exceed an average of 30 MED per day. prescribing opioids for acute pain becomes released the • Health care providers may prescribe effective in December 2017. On June 1, long-awaited opioids in excess of the day supply limits 2018, this will be a requirement for all rules on opioid only if they provide a specific reason controlled substance prescriptions. Our IT prescribing that documented in the medical record. team is working with the EPIC developers track the Centers on strategies to assist providers in meeting for Disease Control The new limits do not apply to opioids these requirements. The OSBM has also and Prevention prescribed for cancer, palliative care, end- announced that it intends to audit providers guidelines. These of-life/hospice care or medication-assisted who exceed the guidelines and promised rules took effect on August 31. They include treatment for addiction. Prescribers should strict enforcement per Gov. John Kasich’s the following basics that apply to the be aware that MED will be calculated direction. first opioid analgesic prescription for the on the maximum use potential on PRN The MED limit is one that will likely trip treatment of an episode of acute pain: prescriptions. Those allowing for more than four Vicodin tablets or the equivalent will be up some doctors. -

2021 Molina Ohio Marketplace Fact Sheet
Ohio Marketplace Fact Sheet Marketplace Counties: Allen Ashtabula Why Choose Molina? Athens Butler Champaign Member Benefits Clark Clermont • NEW $0 deductible Silver and Bronze plans Clinton Coshocton • NEW copay driven plan designs for 2021! Crawford Cuyahoga • FREE 24/7 Teladoc virtual care services and 24-hour nurse advice line Erie Fairfield • FREE child vision benefits include free annual exam and frames/lenses Fayette • FREE annual wellness exams and preventative prescription drugs Franklin Greene • Urgent Care copays are the same as PCP visit copays on all plans Hamilton Hancock • No referral required for specialist visits Highland Holmes • Adult vision services provided by VSP available on select plans Huron Lake • Ability to set up reoccurring premium payments with autopay Lawrence Licking • Ability to choose your PCP at the time of enrollment Lorain Lucas • Mail Order Pharmacy benefit is available to all members Madison Mahoning Molina Healthcare has more than 40 Montgomery Broker Benefits Muskingum years of experience providing quality Pickaway health care for those in need. We offer • Increased renewal commission rates Pike Richland Marketplace plans in California, Florida, • Improved new and renewal member bonus program Ross Michigan, Mississippi, New Mexico, Scioto • One of the best Broker Support Units in the industry Stark Ohio, South Carolina, Texas, Utah, Trumbull • CARE Team can assist with member access to care, claims, and billing Warren Washington, and Wisconsin. Wood www.MolinaHealthcare.com issues without member -

Designated Hospitals and Outpatient Surgery Centers
Ohio and Northern Kentucky UnitedHealthcare Directory of Designated Hospitals and Outpatient Surgery Centers With Choice Plus Advanced with Hospital Tiering, UnitedHealthcare encourages members to make well-informed decisions about who to see and where to go for quality, cost-efficient care through the UnitedHealth Premium® designation program, Place of Service and Hospital Tiering. This directory is a listing of the Designated hospitals and Outpatient Surgery Centers that offer services to UnitedHealthcare members enrolled in our Choice Plus Advanced with Hospital Tiering health plans in Ohio and Northern Kentucky. Members may pay lower co-payments and co-insurance amounts for services provided by Designated hospitals and surgery centers. The providers on this list may change. The Ohio Designated Hospitals and Outpatient Surgery Centers Allen: Belmont: Springfield Regional Cleveland Association Digestive Health Endoscopy Digestive Health Complex Medical Center* 5106 Wilson Mills Rd 375 N Eastown Rd 300 W Main St 100 Medical Center Drive Richmond Heights, OH 44143 Springfield, OH 45504 Lima, OH 45807 Saint Clairsville, OH 43950 Cleveland Center For Digestive Endoscopy Center Valley Endoscopy Center Mercy Memorial Hospital* Health & Endoscopy Of West Central Ohio 68377 STEwart Dr STE 202 904 Scioto St 3700 Park East Dr STE 100A 2793 Shawnee Rd Saint Clairsville, OH 43950 Urbana, OH 43078 Beachwood, OH 44122 Lima, OH 45806 Cleveland Eye/Laser Butler: Clermont: Endoscopy Center Surgery Center GI Endoscopy Center Midwest Eye Surgery Center -
Full Officer List
OHIO SOCIETY OF PATHOLOGISTS OFFICER LISTING OHIO SOCIETY OF PATHOLOGISTS OFFICERS: Delegate/Alternate Term Expiration PRESIDENT: Sean Kirby, MD Term expires 11/2021 Mercy Fairfield Hospital 3000 Mack Road Fairfield, Ohio 45014 (513) 870‐7032 PRESIDENT‐ELECT: Kelsey McHugh, MD Term expires 11/2021 Cleveland Clinic 9500 Euclid Avenue, L25 Cleveland, OH 44195 (216) 212‐3776 Pager: 86690 PAST PRESIDENT: Lori Elwood, MD Term expired 11/2019 Licking Memorial Hospital 1320 W. Main Street Newark, Ohio 43055 (740) 348‐4160) SECRETARY‐TREASURER Susan E. Porter, MD Term expires 11/2020 Hillcrest Hospital Department of Pathology 6780 Mayfield Road Mayfield Heights, OH 44124 (440)312‐4525 OHIO SOCIETY OF PATHOLOGISTS GOVERNORS: Shelley Odronic, MD Term expires 11/2022 St. Rita's Medical Center 750 West High Street Suite 400 Lima, OH 45801 (419) 226‐9224 Rongqin Ren, MD, PhD, FCAP Term expires 11/2022 S305 B Rhodes Hall (moving October 2020) The Ohio State University Medical Center Columbus OH 43210 (614) 366‐5717 Debra Zynger, MD, FCAP Term expires 11/2020 Ohio State University Med Ctr, Pathology 410 W. 10th Avenue, E401 Doan Hall Columbus, Ohio 43210 (614) 293‐7705 Eric Willis, MD Term expires 11/2021 Riverside Methodist Hospital 3535 Olentangy River Road RMH RMH Pathology Department Columbus, OH 43214 (614) 566‐2392 Business (614) 209‐5159 Revised July 26, 2020 vcampana OHIO SOCIETY OF PATHOLOGISTS OFFICER LISTING M. Atef Shrit, M.D. Term expires 11/2021 Miami Valley Hospital One Wyoming Street Dayton, OH 45409 (937) 208‐3588 OSMA REP: Robert G. Gurdak, M.D. Term expires 11/2022 Pathology Consultants, LLC/ Trumbull Memorial Department of Pathology 1350 E.