HEALTH EDUCATION for and by CHILDREN Report of Workshop
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
(Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl
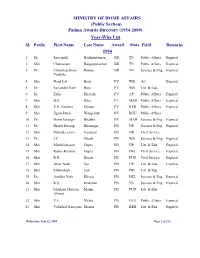
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl. Prefix First Name Last Name Award State Field Remarks 1954 1 Dr. Sarvapalli Radhakrishnan BR TN Public Affairs Expired 2 Shri Chakravarti Rajagopalachari BR TN Public Affairs Expired 3 Dr. Chandrasekhara Raman BR TN Science & Eng. Expired Venkata 4 Shri Nand Lal Bose PV WB Art Expired 5 Dr. Satyendra Nath Bose PV WB Litt. & Edu. 6 Dr. Zakir Hussain PV AP Public Affairs Expired 7 Shri B.G. Kher PV MAH Public Affairs Expired 8 Shri V.K. Krishna Menon PV KER Public Affairs Expired 9 Shri Jigme Dorji Wangchuk PV BHU Public Affairs 10 Dr. Homi Jehangir Bhabha PB MAH Science & Eng. Expired 11 Dr. Shanti Swarup Bhatnagar PB UP Science & Eng. Expired 12 Shri Mahadeva Iyer Ganapati PB OR Civil Service 13 Dr. J.C. Ghosh PB WB Science & Eng. Expired 14 Shri Maithilisharan Gupta PB UP Litt. & Edu. Expired 15 Shri Radha Krishan Gupta PB DEL Civil Service Expired 16 Shri R.R. Handa PB PUN Civil Service Expired 17 Shri Amar Nath Jha PB UP Litt. & Edu. Expired 18 Shri Malihabadi Josh PB DEL Litt. & Edu. 19 Dr. Ajudhia Nath Khosla PB DEL Science & Eng. Expired 20 Shri K.S. Krishnan PB TN Science & Eng. Expired 21 Shri Moulana Hussain Madni PB PUN Litt. & Edu. Ahmed 22 Shri V.L. Mehta PB GUJ Public Affairs Expired 23 Shri Vallathol Narayana Menon PB KER Litt. & Edu. Expired Wednesday, July 22, 2009 Page 1 of 133 Sl. Prefix First Name Last Name Award State Field Remarks 24 Dr. -
Revised NGO List Under Registration Category
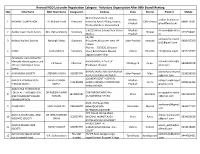
Revised NGO List under Registration Category - Voluntary Organization After 80th Board Meeting SNo NGO Name NGO Head Name Designation Address State District Email id Mobile 48 Panchwati Ward, Opp. Madhya aadhar.foundation 1 AADHAR FOUNDATION ER. Mahesh Kinth President Narendra Ayush Dhaba, Poama, Chhindwara 8989173581 Pradesh @rediffmail.com P/o Kundali Kala, Parasia Road E-4/223,Arera Colony,Near 10 no. Madhya [email protected] 2 Aadhar Gyan Dhatri Samiti Mrs. Ratna Mukerji Secretary Bhopal 9755554401 Market Pradesh m S2/258 adityawelfaresocie 3 Aaditya Welfare Society Narsingh Yadav Secretary Bhojubeer,Bhojubeer,Near UP Uttar Pradesh Varanasi 9936437260 [email protected] College Plot No. - 70/3530, (Ground 4 AAINA Sneha Mishra Secretary Floor),Behind Hotel Mayfair Odisha Khordha [email protected] 9437017967 Lagoon,Jaydev Vihar Aakanksha Lions School for Mentally Handicapped a unit Awanti Vihar,,In front of aakankshalsmh@y 5 K K Nayak Chairman Chattisgarh Raipur 9826845678 of Lions Club Raipur Sewa Bhaktawar Bhawan ahoo.com Samiti KHARAGIPUR,GANGAUPUR,RAM akankshasocietyma 6 AAKANKSHA SOCIETY JITENDRA YADAV SECRETARY Uttar Pradesh Mau 9258038100 AUPUR SUWAH LINK MARG [email protected] 120 NEAR GOVT HOSPITAL AARIOLA PRAKASH PUNJ BALVEER SINGH Madhya balveer.singhrajput 7 CHAIRMAN HARDA,AWASTHI COMPOUND Harda 9009616393 SHIKSHA SAMITI RAJPUT Pradesh @yahoo.com HARDA,HARDA AAROGYAA FOUNDATION FOR HEALTH PROMOTION DR RAJESH KUMAR COAT BAZAR,WARD No aarogyaafoundatio 8 SECERETARY Bihar Sitamarhi 9934691872 AND COMMUNITY BASED SUMAN 13,MAHARANI STHAN -

CHINMAYA MISSION SAN JOSE PUBLICATION November
100years November/December 2015 Vol. 26, No.6 CHINMAYA MISSION SAN JOSE PUBLICATION MISSION STATEMENT To provide to individuals, from any background, the wisdom of Vedanta and practical means for spiritual growth and happiness, enabling them to become a positive contributor to the society. See Infinite Possibilities Open Up There are infinite possibilities in each one of us. We must learn the art of tapping these mighty resources within. The only way to explore these unknown veins of power and strength, efficiency and ability, success and glory, is to put forth our sincere efforts into the work at hand, more diligently, more industriously. Let us keep very high visions of achievement; they by themselves will come to serve as intimations of what we can be; they will summon us to larger and more earnest efforts. Let us realize that whatever we have done so far is nothing and that we can still do much better, and even more to be sure. Immense possibilities are before us. The fields of splendid possibilities, we shall see, widen all by themselves, as we persevere to act and achieve with a sincere spirit of dedication and honesty of purpose. SWAMI CHINMAYANANDA CONTENTS Volume 26 No. 6 November/December 2015 From The Editors Desk . 2 Chinmaya Tej Editorial Staff . 2 Mahasamadhi Camp Experience . 3 Cord Overview . 5 The Lord is With You . 17 Financial Empowerment through Self-Help Groups . 19 Swaranjali Youth Choir . 21 Tapovan Prasad . 21 Chinmaya Study Groups . 22 Adult Classes at Sandeepany . 23 Shiva Abhisheka & Puja . 23 Bala Vihar/Yuva Kendra & Language Classes . -

Annual Report (2014
AANNNNUUAALL RREEPPOORRTT ((22001144 -- 22001155)) People’s Science Institute 653, Indira Nagar, Dehra Doon – 248006 Uttarakhand People’s Science Institute About Peoples’ Science Institute (PSI) People’s Science Institute (PSI) is registered as a society in New Delhi under the Societies Act (1860) and the Foreign Contributions Regulations Act (FCRA). Its stated mission is, “To help eradicate poverty through the empowerment of the poor and the productive, sustainable and equitable use of available human and natural resources.” Operationally it provides technical and managerial support to communities and organizations that work with them, implements development programs and undertakes public interest research. The Institute is known in India’s voluntary sector for its pioneering work in the fields of community-based natural resources and watershed management for improved livelihoods, environmental quality monitoring, river conservation and dissemination of appropriate technologies. PSI has active units for natural resources management, disaster mitigation and response, environmental quality monitoring and innovative projects. Each unit implements development projects, undertakes research and provides training as well as professional support. The Institute has a competent staff of socially conscious engineers, scientists and social workers to carry out these tasks. This annual report outlines the major activities of each group in 2014-15. I. Natural Resources Management The Natural Resources Management (NRM) Group executes the Institute’s natural resource management activities. It assists rural communities to fulfill their basic needs in a sustainable, self-reliant, democratic and socially just manner. It promotes community-led micro-planning for food and livelihoods security and participatory watershed development projects. It also undertakes research in improved agricultural practices, hydrology, water technologies, and NRM institutions and policies. -

(1954-2014) Year-Wise List 1954
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2014) Year-Wise List Sl. Prefix First Name Last Name Award State Field 1954 1 Dr. Sarvapalli Radhakrishnan BR TN Public Affairs 2 Shri Chakravarti Rajagopalachari BR TN Public Affairs 3 Shri Chandrasekhara Raman BR TN Science & Venkata 4 Dr. Satyendra Nath Bose PV WB Litt. & Edu. 5 Shri Nandlal Bose PV WB Art 6 Dr. Zakir Husain PV AP Public Affairs 7 Shri Bal Gangadhar Kher PV MAH Public Affairs 8 Shri V.K. Krishna Menon PV KER Public Affairs 9 Shri Jigme Dorji Wangchuk PV BHU Public Affairs 10 Dr. Homi Jehangir Bhabha PB MAH Science & 11 Dr. Shanti Swarup Bhatnagar PB UP Science & 12 Shri Mahadeva Iyer Ganapati PB OR Civil Service 13 Dr. Jnan Chandra Ghosh PB WB Science & 14 Shri Radha Krishna Gupta PB DEL Civil Service 15 Shri Maithilisharan Gupta PB UP Litt. & Edu. 16 Shri R.R. Handa PB PUN Civil Service 17 Shri Amarnath Jha PB UP Litt. & Edu. 21 May 2014 Page 1 of 193 Sl. Prefix First Name Last Name Award State Field 18 Shri Ajudhia Nath Khosla PB DEL Science & 19 Dr. K.S. Krishnan PB TN Science & 20 Shri Moulana Hussain Madni PB PUN Litt. & Edu. Ahmad 21 Shri Josh Malihabadi PB DEL Litt. & Edu. 22 Shri V.L. Mehta PB GUJ Public Affairs 23 Shri Vallathol Narayan Menon PB KER Litt. & Edu. 24 Dr. Arcot Mudaliar PB TN Litt. & Edu. Lakshamanaswami 25 Lt. (Col) Maharaj Kr. Palden T Namgyal PB PUN Public Affairs 26 Shri V. Narahari Raooo PB KAR Civil Service 27 Shri Pandyala Rau PB AP Civil Service Satyanarayana 28 Shri Jamini Roy PB WB Art 29 Shri Sukumar Sen PB WB Civil Service 30 Shri Satya Narayana Shastri PB UP Medicine 31 Late Smt. -
(Public Section) Padma Awards Directory (1954-2017) Year-Wise List
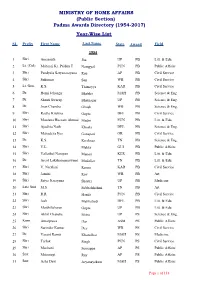
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2017) Year-Wise List SL Prefix First Name Last Name State Award Field 1954 1 Shri Amarnath Jha UP PB Litt. & Edu. 2 Lt. (Col) Maharaj Kr. Palden T Namgyal PUN PB Public Affairs 3 Shri Pandyala Satyanarayana Rau AP PB Civil Service 4 Shri Sukumar Sen WB PB Civil Service 5 Lt. Gen. K.S. Thimayya KAR PB Civil Service 6 Dr. Homi Jehangir Bhabha MAH PB Science & Eng. 7 Dr. Shanti Swarup Bhatnagar UP PB Science & Eng. 8 Dr. Jnan Chandra Ghosh WB PB Science & Eng. 9 Shri Radha Krishna Gupta DEL PB Civil Service 10 Shri Moulana Hussain Ahmad Madni PUN PB Litt. & Edu. 11 Shri Ajudhia Nath Khosla DEL PB Science & Eng. 12 Shri Mahadeva Iyer Ganapati OR PB Civil Service 13 Dr. K.S. Krishnan TN PB Science & Eng. 14 Shri V.L. Mehta GUJ PB Public Affairs 15 Shri Vallathol Narayan Menon KER PB Litt. & Edu. 16 Dr. Arcot Lakshamanaswami Mudaliar TN PB Litt. & Edu. 17 Shri V. Narahari Raooo KAR PB Civil Service 18 Shri Jamini Roy WB PB Art 19 Shri Satya Narayana Shastri UP PB Medicine 20 Late Smt. M.S. Subbalakshmi TN PB Art 21 Shri R.R. Handa PUN PB Civil Service 22 Shri Josh Malihabadi DEL PB Litt. & Edu. 23 Shri Maithilisharan Gupta UP PB Litt. & Edu. 24 Shri Akhil Chandra Mitra UP PS Science & Eng. 25 Kum. Amalprava Das ASM PS Public Affairs 26 Shri Surinder Kumar Dey WB PS Civil Service 27 Dr. Vasant Ramji Khanolkar MAH PS Medicine 28 Shri Tarlok Singh PUN PS Civil Service 29 Shri Machani Somappa AP PS Public Affairs 30 Smt. -

Annual Report Summary – 1St April 2019 –31St March 2020
Annual Report Summary – 1st April 2019 –31st March 2020 Office of National Director and CORD Training Centre Sidhbari, Tehsil Dharamshala, District Kangra, Himachal Pradesh Email: [email protected], URL: www.cordindia.in, Facebook: www.facebook.com/CORD.India Phone No: +91-1892-236987, 234322, Fax: +91-1892-235829; +91-981-665-5592 1 Introduction: CORD’s thrust is to harness human resources and enable poorest of the poor to transform their lives through programs driven by themselves in rural India. Comprehensive nature of integrated programs components of CORD have a strong faith in inner divine potential of human being and hence brings the most vulnerable and needy ones in rural communities to the centrestage of their development and empowerment through their organisations and self efforts. All program components briefly described in this narrative report suplement and complement national and global development efforts i.e 17 Sustaibale Development Goals (SDGs) – Agenda 2030; 14 SDGs directly and 3 SDGs indirectly. To know more about CORD’s evolution and Panchayat based adaptable, scalable and replicable comprehensive integrated rural development model, please visit, www.cordindia.in and stay updated with work atwww.facebook.com/CORD.India. Each CORD sites and thematic programs have their detail reports of comprehensive program activities. CORD sites could be contacted through their contact details given at the end of this report. Please contact Shri Narender Paul, Chief Operating Officer CORD in case you need more detail reports or anything specific information at +91-9816655592; Email: [email protected] Reach: 286 Gram Panchayats (1130 Wards) and 09 Municipal Panchayats in six States covering 904 villages (734 villages at CORD Sidhbari and its Satellite Sites in Uttrakhand, Chamba & Punjab).