Oral History Project
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Background to the Celebration of Herbert D. Kleber (1904 -2018) by Thomas A
1 Background to the Celebration of Herbert D. Kleber (1904 -2018) by Thomas A. Ban By the mid-1990s the pioneering generation in neuropsychopharmacology was fading away. To preserve their legacy the late Oakley Ray (1931-2007), at the time Secretary of the American College of Neuropsychopharmacology (ACNP), generated funds from Solway Pharmaceuticals for the founding of the ACNP-Solway Archives in Neuropsychopharmacology. Ray also arranged for the videotaping of interviews (mainly by their peers) with the pioneers, mostly at annual meetings, to be stored in the archives. Herbert Kleber was interviewed by Andrea Tone, a medical historian at the Annual Meeting of the College held in San Juan, Puerto Rico, on December 7, 2003 (Ban 2011a; Kleber 2011a). The endeavor that was to become known as the “oral history project” is based on 235 videotaped interviews conducted by 66 interviewers with 213 interviewees which, on the basis of their content, were divided and edited into a 10-volume series produced by Thomas A. Ban, in collaboration with nine colleagues who were to become volume editors. One of them, Herbert Kleber, was responsible for the editing of Volume Six, dedicated to Addiction (Kleber 2011b). The series was published by the ACNP with the title “An Oral History of Neuropsychopharmacology Peer Interviews The First Fifty Years” and released at the 50th Anniversary Meeting of the College in 2011 (Ban 2011b). Herbert Daniel Kleber was born January 19, 1934, in Pittsburgh, Pennsylvania. His family’s father’s side was from Vilnius, Lithuania, and the Mother’s side was from Germany. Both families came to the United State during the first decade of the 20th century. -

HEHS-96-80 Cocaine Treatment Outcomes B-265688
United States General Accounting Office GAO Report to Congressional Requesters June 1996 COCAINE TREATMENT Early Results From Various Approaches GOA years 1921 - 1996 GAO/HEHS-96-80 United States General Accounting Office GAO Washington, D.C. 20548 Health, Education, and Human Services Division B-265688 June 7, 1996 The Honorable William F. Clinger, Jr. Chairman The Honorable Cardiss Collins Ranking Minority Member Committee on Government Reform and Oversight House of Representatives The Honorable Henry A. Waxman House of Representatives Cocaine use in the United States remains a serious and costly epidemic. In 1994, the National Household Survey on Drug Abuse conservatively estimated that more than three-quarters of a million people had used cocaine at least once a week within the past year. In 1993, cocaine was associated with almost 4,000 deaths.1 Today, an estimated $10 billion per year is lost in cocaine-related crimes and productivity.2 Although cocaine admissions to state-supported drug abuse treatment programs between 1985 and 1990 increased dramatically—from almost 39,000 people to more than 200,000—we found in 1991 that an effective treatment for cocaine addiction had not yet been identified.3 Today, public/private expenditures on cocaine-related treatment total about $1 billion per year. Because of cocaine’s serious health, economic, and criminal justice implications for the nation, we have provided a status report on recent progress made in finding an effective treatment for cocaine users.4 Specifically, we reviewed the various types of federally funded treatment approaches evaluated over the past 5 years (1991 through 1995) to (1) determine the extent to which these therapies have proven successful and (2) identify additional research initiatives necessary to increase our knowledge of cocaine treatment effectiveness. -
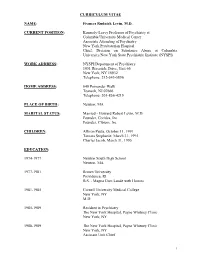
CV Levin.Pdf
CURRICULUM VITAE NAME: Frances Rudnick Levin, M.D. CURRENT POSITION: Kennedy-Leavy Professor of Psychiatry at Columbia University Medical Center Associate Attending of Psychiatry New York Presbyterian Hospital Chief, Division on Substance Abuse at Columbia University/New York State Psychiatric Institute (NYSPI) WORK ADDRESS: NYSPI/Department of Psychiatry 1051 Riverside Drive, Unit 66 New York, NY 10032 Telephone: 212-543-5896 HOME ADDRESS: 640 Pomander Walk Teaneck, NJ 07666 Telephone: 201-836-4219 PLACE OF BIRTH: Newton, MA MARITAL STATUS: Married - Howard Robert Levin, M.D. Founder, Coridea, Inc Founder, Cibiem, Inc. CHILDREN: Allison Paula, October 11, 1991 Tamara Stephanie, March 31, 1995 Charles Jacob, March 31, 1995 EDUCATION: 1974-1977 Newton South High School Newton, MA 1977-1981 Brown University Providence, RI B.S. - Magna Cum Laude with Honors 1981-1985 Cornell University Medical College New York, NY M.D. 1985-1989 Resident in Psychiatry The New York Hospital, Payne Whitney Clinic New York, NY 1988-1989 The New York Hospital, Payne Whitney Clinic New York, NY Assistant Unit Chief 1 1989-1990 National Institute on Drug Abuse and University of Maryland Baltimore, MD Research and Addiction Psychiatry Fellow ACADEMIC APPOINTMENTS: University of Maryland Medical Center, Department of Psychiatry 1990-1992 Assistant Professor Columbia University College of Physicians and Surgeons, Department of Psychiatry 1992-1999 Assistant Professor of Clinical Psychiatry 1999- 2006 Q.J. Kennedy Associate Professor of Clinical Psychiatry 2006-2013 -

AMERICAN PSYCHIATRIC ASSOCIATION 165Th Annual Meeting Philadelphia, PA • May 5-9, 2012 SATURDAY, MAY 5
Advancing Psychiatric Practice Through the Science of Addiction A Research Track From the NATIONAL INSTITUTE ON DRUG ABUSE AMERICAN PSYCHIATRIC ASSOCIATION 165th Annual Meeting Philadelphia, PA • May 5-9, 2012 SATURDAY, MAY 5 MISSION STATEMENT NIDA’s mission is to lead the Nation in bringing the power of science to bear on drug abuse and addiction. This charge has two critical components. The first is the strategic support and conduct of research across a broad range of disciplines from genetics and neurobiology to clinical and behavioral science to health services research. The second is ensuring the rapid and effective dissemination and use of the results of that research to improve prevention and treatment and to inform policy. EXHIBIT A wide variety of materials are available at the NIDA exhibit, at Booth 633, in the American Psychiatric Association Exhibit Hall. Please allow time to visit the NIDA exhibit to learn more about drug abuse. WEBSITE Information about NIDA research, programs, and events is accessible through NIDA’s website at www.drugabuse.gov. PAGE 1 PAGE 2 SATURDAY, MAY 5 Saturday, May 5 2:00 p.m.-5:00 p.m. (Symposium #S10) Social Stress and Drug Addiction in Preclinical and Clinical Studies: Sex/Gender Matters in Effects on Brain and Behavior and Treatment Implications Pennsylvania Convention Center, Room 103A, Level 1 Co-Chairs: Cora Lee Wetherington, Ph.D. National Institute on Drug Abuse Samia Noursi, Ph.D. National Institute on Drug Abuse Presenters: Michael Nader, Ph.D. Wake Forest University School of Medicine Monkey Models of Social Stress and Cocaine Abuse: Sex Differences Sari Izenwasser, Ph.D. -

National Drug Abuse Treatment Clincal Trials Network
NATIONAL DRUG ABUSE TREATMENT CLINCAL TRIALS NETWORK The National Drug Abuse Treatment Clinical Trials Network (CTN) provides an enterprise in which the National Institute on Drug Abuse, treatment researchers, and community-based service providers cooperatively develop, validate, refine, and deliver new treatment options to patients in Community Treatment Programs (CTPs). This unique partnership between CTPs and academic research leaders aims to achieve the following objectives: • Conducting studies of behavioral, pharmacological, and integrated behavioral and pharmacological treatment interventions of therapeutic effect in rigorous, multisite clinical trials to determine effectiveness across a broad range of community-based treatment settings and diversified patient populations; and • Ensuring the transfer of research results to physicians, clinicians, providers, and patients. The CTN framework consists of the National Institute on Drug Abuse, multiple Nodes, or Regional Research and Training Centers (RRTCs) – each linked with several CTPs – together with a Clinical Coordinating Center and two Data and Statistical Centers. This framework provide a broad and powerful infrastructure for the rapid, multisite testing and delivery of promising science-based therapies to patients in community-based treatment settings nationwide. The CTN Directory provides an overview of the active Nodes and Coordinating Centers, followed by membership information. For more information, visit the Web site at http://www.drugabuse.gov/CTN/. Nodes APPALACHIAN TRI-STATE NODE Regional Research and Training Center Principal Investigator University of Pittsburgh Dennis Daley, Ph.D., LSW Pittsburgh, Pennsylvania Email: [email protected] DELAWARE VALLEY NODE Regional Research and Training Center Principal Investigator University of Pennsylvania George Woody, M.D. Philadelphia, Pennsylvania Email: [email protected] FLORIDA NODE ALLIANCE Regional Research and Training Center Principal Investigators University of Miami José Szapocznik, Ph.D. -

1 Corporate Crime and the Regulatory State: the Case
CORPORATE CRIME AND THE REGULATORY STATE: THE CASE OF PURDUE PHARMA AND OXYCONTIN® By O. HAYDEN GRIFFIN, III A DISSERTATION PRESENTED TO THE GRADUATE SCHOOL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 2011 1 © 2011 O. HAYDEN GRIFFIN, III 2 To my mother and father, thanks for all the love and support through the odyssey that was my education. You both mean the world to me and none of this would have been possible without the two of you. 3 ACKNOWLEDGMENTS I would first like to thank Joe Spillane for being my mentor for the full five years I was a graduate student at the University of Florida. From the advice he provided on seminar papers, to suggesting books and articles I should read, to critiquing my ideas, to shaping my research agenda, to the endless work he did with me on my dissertation – no other person will likely have the same impact on my career. I have not always made things easy for myself and unfortunately, this has often provided him with more than a few headaches along the way. Thus, I would like to thank him for seeing me through; I will always be grateful. I would like to thank Lonn Lanza-Kaduce for all the help he has provided me as both an advisor, a teacher and a committee member. I would also like to thank him for providing me with the opportunity to teach and all the advice he provided, especially early in my tenure in graduate school. -
Yale Medicine Magazine
yale medicine autumn 2003 ’Round and ’round Local take on For sensory expert, the a global outbreak a taste of success early days of dna 24 30 14 16 autumn 2003 yale medicine CONTENTS 2 Letters 4 Chronicle 8 Rounds 10 Findings 12 Books 13 On Campus 14 Capsule on the cover 16 Building a better drug Academic researchers in pharma- The rational approach to drug discovery is changing cology have long relied on intuition to advance the process of drug pharmacology, but serendipity and imagination still play discovery. Even in today’s more a starring role. technology-driven and “rational” By Marc Wortman environment, there’s nothing like an inspired hunch. 24 Illustration by Gary Clement When a global outbreak becomes local For the shoe-leather work of public health, Connecticut officials seek help from Yale’s disease detectives. By Jennifer Kaylin 30 A matter of taste Debunking myths and shattering stereotypes has long been part of Linda Bartoshuk’s career path. By Peter Farley 34 Faculty 38 Students 46 Alumni 56 Faces 62 In Memoriam 64 Follow-Up 64 Archives On the Web info.med.yale.edu/ymm On our website, readers can submit class notes or a change of address, check the alumni events calendar, arrange for a lifelong Yale e-mail alias through the virtual Yale Station and search our electronic archive. 2 letters from the editor 3 the rest of the profession. The of going to my office and talk- People may think that you are ery. My experience is described The things that matter yale medicine conclusion is obvious: state ing with my patients, then I irrelevant, but as long as you are in a chapter in a book called Alumni Bulletin of the boards should recognize that it will move to another phase of convinced that you are not, you Doctors Afield, published by Yale As one can see from these pages, our mailbag has been Yale University School of Medicine Autumn 2003, Volume 38, No. -

0327 JN April Color
APRIL 1, 2003 Jeffwww.Jefferson.edu NEWS www.JeffersonHospital.org Jefferson Medical College Initiates ‘Hugs’ for Transplant Patients Landmark Study to Help Close Minority Physician Gap Students from Downingtown Middle School presented liver and kidney Five prominent faculty members of Research Activities,” the study is The study compared 148 living transplant recipients with brightly colored “hug” pillows. Jefferson Medical College (JMC) scheduled for publication in the African American alumni who At right: William Kerr, who received a donor kidney from his wife have joined in a landmark research Spring 2003 issue of Teaching and graduated from JMC between 1960 Cheryl, seated next to Lauren Hedrick, 11. study comparing like numbers of Learning in Medicine. An and 1995 with a matched control Below: Patricia Wallace, Director, white and African-American JMC International Journal. To date, no group of 148 white JMC alumni. Community, Pastoral and Volunteer Services, alumni. such comparison studies have been Both groups were found to be and the students’ faculty adviser, Sue Lackovic, The study is seen as a first step in published in the research literature. comparable as to satisfaction with who has been organizing the annual visits to comparing similar categories of data The five JMC authors are: their medical education, careers hospitals ever about minority and white physicians John J. Gartland, MD, University and professional and research since she received so that eventually the numbers of Medical Editor; Mohammadreza activities. No significant differences a kidney transplant under-represented minority Hojat, PhD, Research Professor of were noted between the two 10 years ago. physicians nationally will increase to Psychiatry and Human Behavior; groups, including satisfaction with match minority population numbers Edward B. -
Testing for Abuse Liability of Drugs in Humans
Testing for Abuse Liability of Drugs in Humans U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse, and Mental Health Administration Testing for Abuse Liability of Drugs in Humans Editors: Marian W. Fischman, Ph.D. The Johns Hopkins University School of Medicine Baltimore, MD Nancy K. Mello, Ph.D. Harvard Medical School/McLean Hospital Belmont, MA NIDA RESEARCH MONOGRAPH No. 92 1989 U.S. Department of Health and Human Services Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 i NIDA Research Monographs are prepared by the research divisions of the National Institute on Drug Abuse and published by its Office of Science. The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. Its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. MARY L. JACOBSON Temple University School of Medicine National Federation of Parents for Philadelphia, Pennsylvania Drug-Free Youth Omaha, Nebraska SYDNEY ARCHER, Ph.D. Rensselaer Polytechnic Institute REESE T. JONES, M.D. Troy, New York Langley Porter Neuropsychiatric Institute RICHARD E. BELLEVILLE, Ph.D. San Francisco, California NB Associates, Health Sciences DENISE KANDEL, Ph.D. Rockville, Maryland College of Physicians and Surgeons of Columbia University KARST J. BESTEMAN New York, New York Alcohol and Drug Problems Association of North America HERBERT KLEBER, M.D. Washington, D.C. Yale University School of Medicine New Haven, Connecticut GILBERT J. -

Problems of Drug Dependence, 1985
National Institute on Drug Abuse MONOGRAPH SERIES Problems of Drug Dependence, 1985 Proceedings of the 47th Annual Scientific Meeting The Committee on Problems of Drug Dependence, Inc. U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse, and Mental Health Administration Problems of Drug Dependence, 1985 Proceedings of the 47th Annual Scientific Meeting, The Committee on Problems of Drug Dependence, Inc. Editor: Louis S. Harris, Ph.D. NIDA Research Monograph 67 1986 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse Office of Science 5600 Fishers Lane Rockville, Maryland 20857 For sale by the Superintendent of Documents, US. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National Institute on Drug Abuse and published by its Office of Science. The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integra- tive research reviews. Its dual publication emphasis is rapid and targeted dissem- ination to the scientific and professional community. Editorial Advisors Martin W. Adler, Ph.D. Sidney Cohen, M.D. Temple University School of Medicine Los Angeles, California Philadelphia, Pennsylvania Sydney Archer, Ph.D. Mary L. Jacobson Rensselaer Polytechnic Institute National Federation of Parents for Troy, New York Drug-Free Youth Omaha, Nebraska Richard E. Belleville, Ph.D. NB Associates, Health Sciences Rockville, Maryland Reese T. Jones, M.D. Langley Porter Neuropsychiatrlc Institute Karst J. Besteman San Francisco, California Alcohol and Drug Problems Association of North America Washington, D.C. -

Drug Abuse Treatment
Drug Abuse Treatment NN0026 Introduction The National Institute on Drug Abuse (NIDA) supports more than 85 percent of the world’s research on drug abuse and addiction. NIDA-funded research enables scientists to apply the most advanced techniques available to the study of every aspect of drug abuse, including: • genetic and social determinants of vulnerability and response to drugs; • short- and long-term effects of drugs on the brain, including addiction; • other health and social impacts of drug abuse, including infectious diseases and economic costs; • development and testing of medication and behavioral treatments for abuse and addiction; and • development and evaluation of effective messages to deter young people, in particular, from abusing drugs. Included in this document are selections of topic-specific articles reprinted from NIDA’s research newsletter, NIDA NOTES. Six times per year, NIDA NOTES reports on important highlights from NIDA-sponsored research, in a format that specialists and lay readers alike can read and put to use. Selections like the current one are intended to remind regular NIDA NOTES readers and inform other readers of important research discoveries during the periods they cover. We hope the information contained here answers your needs and interests. To subscribe to NIDA NOTES and for further information on NIDA’s drug abuse and addiction research, please visit our Web site at www.drugabuse.gov. ii Table of Contents NIDA’s Clinical Trials Network Marks Progress Recovery Harder for Addicts Who Start Young Toward Improved Drug Abuse Treatment (V14-6; March 2000) . 31 (V16-6; February 2002) . 1 UCLA Study Looks at Women in Treatment Blood Pressure Medication May Improve Cocaine (V14-6; March 2000) . -

Substance Abuse and the American Woman. INSTITUTION Columbia Univ., New York, NY
DOCUMENT RESUME ED 400 494 CG 027 381 TITLE Substance Abuse and the American Woman. INSTITUTION Columbia Univ., New York, NY. National Center on Addiction and Substance Abuse. SPONS AGENCY Bristol-Myers Squibb Foundation, Inc., New York, NY.; Pew Charitable Trusts, Philadelphia, PA. PUB DATE Jun 96 NOTE 308p. PUB TYPE Reports Research/Technical (143) EDRS PRICE MFO1 /PC13 Plus Postage. DESCRIPTORS Alcoholism; At Risk Persons; *Behavior; Drug Abuse; Drug Addiction; *Drug Use; Family Environment; *Females; Literature Reviews; Sex Differences; *State of the Art Reviews; *Substance Abuse ABSTRACT The first comprehensive assessment of substance abuse and women, this report arose from an analysis of more than 1,700 scientific and technical articles, surveys, government reports and books. Results show that American women are closing the gap with men in that they are increasingly likely to abuse substances at the same rate as men. Findings show that women are starting to smoke, drink, and use drugs at earlier ages than ever before. Unlike men, though, women get drunk faster, become addicted quicker, and develop substance abuse-related diseases sooner. Furthermore, at least one of every five pregnant women uses drugs, drinks, or smokes. An enormous gap exists between what experts know about women's substance abuse and what is known and acted on by women and those who care for them. It is recommended that women be made aware of the dangers of substance abuse. Prevention programs must address the reasons why women abuse substances and such programs must identify girls at highest risk. Health professionals, too, must recognize that women will manifest symptoms of substance abuse that are different from those of men, which may include a woman trying harder to hide her substance abuse due to intense shame.