Retinoids Delivery Systems in Cancer: Liposomal Fenretinide for Neuroectodermal-Derived Tumors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
4-Hydroxyphenyiretinamide
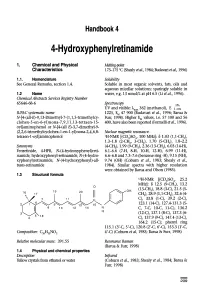
Handbook 4 4-Hydroxyphenyiretinamide 1. Chemical and Physical Melting-point Characteristics 173-175 °C (Shealy etal., 1984; Budavari etal., 1996) 1.1. Nomenclature Solubility See General Remarks, section 1.4. Soluble in most organic solvents, fats, oils and aqueous micellar solutions; sparingly soluble in 1.2 Name water, e.g. 13 nmol/L at pH 6.5 (Li et al., 1996). Chemical Abstracts Services Registry Number 65646-68-6 Spectroscopy 1% UV and visible: ? 362 (methanol), E 1 IUPAC systematic name 1225, EM 47 900 (Budavari et al., 1996; Barua & N-[4-(all-E)-9, 13-Dimethyl-7-(1, 1,5-trimethylcy- Fun, 1998). Higher EM values, i.e. 57 100 and 56 clohex-5 -en-6-yl)nona- 7,9,11,1 3-tetraen- 15- 400, have also been reported (Formelli et al., 1996). oyl]aminophenol or N-[4-(all E)-3, 7-dimethyl-9- (2,2,6-trimethylcyclohex-1-en-1-yl)nona-2,4,6,8- Nuclear magnetic resonance: tetraen-1-oyl]aminophenol 'H-NMR [(CD3)SO4, 100 MHz]: 8 1.03 (1,1-CH3), 1.3-1.8 (2-CH2, 3-CH), 1.70 (5-CH), 1.8-2.2 Synonyms (4-CH2), 1.99 (9-CH), 2.36 (13-CH), 6.03 (14-H), Fenretinide, 4-HPR, N-(4-hydroxyphenyl)reti- 6.1-6.6 (7-H, 8-H, 10-H, 12-H), 6.99 (11-H), namide, hydroxyphenyl-retinamide, N-(4-hydro- 6.6-6.8 and 7.3-7.6 (benzene ring -H), 9.15 (NH), xyphenyl)retinamide, N-(4-hydroxyphenyl)-all- 9.74 (OH) (Coburn et al., 1983; Shealy et al., tnins-retinamide 1984). -

Microencapsulation of Amorphous Solid Dispersions of Fenretinide Enhances Drug Solubility and Release from PLGA in Vitro and in Vivo T ⁎ Kari Nietoa, Susan R
International Journal of Pharmaceutics 586 (2020) 119475 Contents lists available at ScienceDirect International Journal of Pharmaceutics journal homepage: www.elsevier.com/locate/ijpharm Microencapsulation of amorphous solid dispersions of fenretinide enhances drug solubility and release from PLGA in vitro and in vivo T ⁎ Kari Nietoa, Susan R. Malleryb, Steven P. Schwendemana,c, a Department of Pharmaceutical Sciences and The Biointerfaces Institute, University of Michigan, Ann Arbor, MI, United States b Division of Oral Maxillofacial Pathology & Radiology, College of Dentistry, Ohio State University, Columbus, OH, United States c Department of Biomedical Engineering, University of Michigan, Ann Arbor, MI, United States ARTICLE INFO ABSTRACT Keywords: The purpose of this study was to develop solid dispersions of fenretinide(4HPR), incorporate them into poly Fenretinide (4HPR) (lactic-co-glycolic)(PLGA) millicylindrical implants, and evaluate the resulting implants in vitro and in vivo for polyvinylpyrrolidone (PVP) future applications in oral cancer chemoprevention. Due to the extreme hydrophobicity of 4HPR, 4HPR-poly- amorphous solid dispersion (ASD) vinylpyrrolidone (PVP) amorphous solid dispersions(ASDs) were prepared for solubility enhancement. The Solubility enhancement optimal PVP-4HPR ratio of 9/1(w/w) provided a 50-fold solubility enhancement in aqueous media, which was Poly(lactic-co-glycolic) (PLGA) sustained over 1 week. PVP-4HPR ASD particles were loaded into PLGA millicylinders and drug release was In vivo release long-acting release (LAR) evaluated in vitro in PBST and in vivo by recovery from subcutaneous injection in rats. While initial formulations of PLGA PVP-4HPR millicylinders only released 10% 4HPR in vitro after 28 days, addition of the plasticizer triethyl-o-acetyl-citrate(TEAC) into PVP-4HPR ASDs resulted in a 5.6-fold total increase in drug release. -

Agonist and Antagonist of Retinoic Acid Receptors Cause Similar Changes in Gene Expression and Induce Senescence-Like Growth Arrest in MCF-7 Breast Carcinoma Cells
Research Article Agonist and Antagonist of Retinoic Acid Receptors Cause Similar Changes in Gene Expression and Induce Senescence-like Growth Arrest in MCF-7 Breast Carcinoma Cells Yuhong Chen,1 Milos Dokmanovic,1 Wilfred D. Stein,1,2 Robert J. Ardecky,3 and Igor B. Roninson1 1Cancer Center, Ordway Research Institute, Albany, New York; 2Institute of Life Sciences, Hebrew University, Jerusalem, Israel; and 3Ligand Pharmaceuticals, Inc., San Diego, California Abstract retinoids is most often attributed to the induction of differentia- Biological effects of retinoids are mediated via retinoic acid tion, but these compounds were also shown to stop the growth of (RA) receptors (RAR) and retinoid X receptors (RXR). The tumor cells by inducing apoptosis or accelerated senescence (1, 2). best-characterized mechanism of retinoid action is stimula- In particular, treatment of two human breast carcinoma cell lines tion of transcription from promoters containing RA response with all-trans retinoic acid (RA) or fenretinide, in vitro or in vivo, elements (RARE). Retinoids induce senescence-like growth induces a senescence-like phenotype characterized by increased h arrest in MCF-7 breast carcinoma cells; this effect is cell size and expression of senescence-associated -galactosidase h associated with the induction of several growth-inhibitory (SA- -gal; refs. 3, 4). This phenotype, as investigated in MCF-7 cells, genes. We have nowfound that these genes are induced by is associated with irreversible growth arrest and up-regulation of RAR-specific but not by RXR-specific ligands. Genome-scale several intracellular and secreted proteins with known growth- microarray analysis of gene expression was used to compare inhibitory activities. -

The Mechanisms of Fenretinide-Mediated Anti-Cancer Activity and Prevention of Obesity and Type-2 Diabetes
*Manuscript Click here to view linked References The mechanisms of Fenretinide-mediated anti-cancer activity and 1 2 3 prevention of obesity and type-2 diabetes. 4 5 Authors: Nimesh Mody* and George D. Mcilroy. 6 7 8 Institute of Medical Sciences, College of Life Sciences & Medicine, University of Aberdeen, 9 10 Aberdeen, UK 11 12 * corresponding author 13 14 15 Running title: The synthetic retinoid, Fenretinide. 16 17 Abbreviations: Fenretinide, FEN; 18 19 20 Keywords: apoptosis, autophagy, reactive oxygen species, retinoic acid, adipogenesis, 21 22 obesity, type-2 diabetes. 23 24 25 Word count: 7169 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 1 63 64 65 ABSTRACT 1 2 3 4 Fenretinide remains the most investigated retinoid compound for the prevention of cancer. Its 5 6 clinical use remains a genuine possibility due to a favourable toxicological profile and 7 8 accumulation in fatty tissues. Like other well-characterised pharmacological therapies, 9 10 11 Fenretinide has been shown to affect multiple signalling pathways. Recent findings have 12 13 discovered additional beneficial properties the synthetic retinoid was not intentionally 14 15 16 designed for, including the prevention of high-fat diet-induced obesity and insulin resistance. 17 18 These preclinical findings in rodents are timely since obesity has reached pandemic 19 20 21 proportions and safe effective therapeutics are severely lacking. Recent investigations have 22 23 proposed various mechanisms of action for the beneficial effects of Fenretinide. -

A Group of Chimeric Antigen Receptors (Cars)
(19) *EP003632461A1* (11) EP 3 632 461 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.04.2020 Bulletin 2020/15 A61K 39/00 (2006.01) (21) Application number: 18198850.2 (22) Date of filing: 05.10.2018 (84) Designated Contracting States: (72) Inventors: AL AT BE BG CH CY CZ DE DK EE ES FI FR GB • SALZER, Benjamin GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO 3744 Stockern (AT) PL PT RO RS SE SI SK SM TR •LEHNER, Manfred Designated Extension States: 1090 Vienna (AT) BA ME • TRAXLMAYR, Michael Designated Validation States: 1180 Vienna (AT) KH MA MD TN (74) Representative: Sonn & Partner Patentanwälte (71) Applicants: Riemergasse 14 • St. Anna Kinderkrebsforschung 1010 Wien (AT) 1090 Vienna (AT) • Universität für Bodenkultur Wien 1180 Wien (AT) (54) A GROUP OF CHIMERIC ANTIGEN RECEPTORS (CARS) (57) Disclosed is a group of chimeric antigen recep- regulating molecule and optionally reduced by another tors (CARs) consisting of two, three or four CAR mole- regulating molecule, or occurs in the absence of a regu- cules, lating molecule and is reduced by a regulating molecule, wherein the members of the group of CARs can be dif- and ferent or identical in their amino acid sequences to one wherein the ectodomain of each CAR molecule of the another, and group in its prevalent conformation is free of cysteine wherein each of the CAR molecules of the group com- amino acid moieties which are able to form intermolecular prise at least a transmembrane domain and an ectodo- disulphide bonds with other CAR molecules of the -

The Effects of N-3 Fatty Acids and Bexarotene on Breast Cancer Cell Progression
Journal of Cancer Therapy, 2011, 2, 710-714 doi:10.4236/jct.2011.25096 Published Online December 2011 (http://www.SciRP.org/journal/jct) The Effects of n-3 Fatty Acids and Bexarotene on Breast Cancer Cell Progression Jessica Trappmann, Susan N. Hawk Department of Nutrition, Exercise and Health Sciences, Central Washington University, Ellensburg, USA. E-mail: [email protected] Received September 28th, 2011; revised October 25th, 2011; accepted November 7th, 2011. ABSTRACT Breast cancer cell growth can be inhibited in vivo by retinoid X receptor (RXR) specific retinoids. In both animal and cell culture studies, omega-3 fatty acids share growth regulatory effects similar to those of RXR specific retinoids (rex- inoids). One synthetic rexinoid, bexarotene (LCD 1069, Targretin), is used clinically to treat cancer patients. Of con- cern is that some patients are unable to tolerate high doses of such treatment drugs. We hypothesized that n-3 fatty ac- ids and bexarotene may work synergistically to slow breast cancer cell growth. To test our hypothesis, we used MCF-7 human mammary carcinoma cells and an in vitro cell culture model. We investigated the relationship between the omega-3 fatty acids docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) alone and in conjunction with bex- arotene in slowing MCF-7 cell growth. Following a 72 hr incubation with the respective treatments, bexarotene en- hanced cell growth (p < 0.05) while DHA showed a strong growth inhibitory effect which was not enhanced by the ad- dition of bexarotene (p < 0.05). EPA alone was not effective in altering cell growth (p < 0.05). -

Retinoid-Induced Apoptosis in Normal and Neoplastic Tissues
Cell Death and Differentiation (1998) 5, 11 ± 19 1998 Stockton Press All rights reserved 13509047/98 $12.00 Review Retinoid-induced apoptosis in normal and neoplastic tissues Laszlo Nagy1,3,4, Vilmos A. Thomazy1, Richard A. Heyman2 retinoic acid receptor (RAR), which belongs to the superfamily and Peter J.A. Davies1,3 of ligand-activated transcription factors (nuclear receptors) revolutionized our understanding as to how retinoids exert 1 Department of Pharmacology, University of Texas-Houston, Medical School, their pleiotropic effects (for reviews see Chambon (1996); Houston, Texas 77225 USA Mangelsdorf et al (1994)). Members of the nuclear receptor 2 Ligand Pharmaceuticals, San Diego, California, 92121 USA superfamily mediate the biological effects of many hormones, 3 Corresponding author: PJAD, tel: 713-500-7480; fax: 713-500-7455; vitamins and drugs (i.e. steroid hormones, thyroid hormones, e-mail: [email protected] 4 vitamin D, prostaglandin-J (PG-J ) and drugs that activate Present address for correspondence: The Salk Institute for Biological Studies, 2 2 Gene Expression Laboratory, La Jolla, California 92037; peroxisomal proliferation). There are two families of retinoid tel: (619) 453-4100 fax:(619) 455-1349; e-mail: [email protected] receptors, Retinoid X Receptors (RXRs) that bind 9-cis retinoic acid (9-cis RA) and Retinoic Acid Receptors (RARs) Received 18.8.97; revised 19.9.97; accepted 22.9.97 that bind both 9-cis RA and all-trans retinoic acid (ATRA) (for Edited by M. Piacentini reviews see Chambon 1996; Mangelsdorf et al, 1994)). Each of these receptor families includes at least three distinct genes, (RARa,b and g; RXRa,b and g) that through differential Abstract promoter usage and alternative splicing, give rise to a large number of distinct retinoid receptor proteins (for reviews see Vitamin A and its derivatives (collectively referred to as Chambon 1996; Mangelsdorf et al, 1994). -

Localized Transdermal Delivery of Chemopreventive Agents to the Breast Abdulsalam Alqahtani South Dakota State University
South Dakota State University Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange Electronic Theses and Dissertations 2019 Localized Transdermal Delivery of Chemopreventive Agents to the Breast Abdulsalam Alqahtani South Dakota State University Follow this and additional works at: https://openprairie.sdstate.edu/etd Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Alqahtani, Abdulsalam, "Localized Transdermal Delivery of Chemopreventive Agents to the Breast" (2019). Electronic Theses and Dissertations. 3399. https://openprairie.sdstate.edu/etd/3399 This Dissertation - Open Access is brought to you for free and open access by Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange. For more information, please contact [email protected]. LOCALIZED TRANSDERMAL DELIVERY OF CHEMOPREVENTIVE AGENTS TO THE BREAST BY ABDULSALAM ALQAHTANI A dissertation submitted in partial fulfillment of the requirements for the Doctor of Philosophy Major in Pharmaceutical Sciences South Dakota State University 2019 iii This dissertation is dedicated to my family iv ACKNOWLEDGMENTS I am very thankful to many people who contributed to my Ph.D. work presented in this dissertation. First of all, I would like to thank my major advisor Dr. Omathanu Perumal for giving me the opportunity to join his lab and work with him for my Ph.D. degree. I would like to express my sincere gratitude and appreciation to Dr. Perumal for his continuous support, guidance, motivation and mentorship during my Ph.D. -

Disturbed Vitamin a Metabolism in Non-Alcoholic Fatty Liver Disease (NAFLD)
nutrients Review Disturbed Vitamin A Metabolism in Non-Alcoholic Fatty Liver Disease (NAFLD) Ali Saeed 1,2, Robin P. F. Dullaart 3, Tim C. M. A. Schreuder 1, Hans Blokzijl 1 and Klaas Nico Faber 1,4,* 1 Department of Gastroenterology and Hepatology, University Medical Center Groningen, University of Groningen, 9713 GZ Groningen, The Netherlands; [email protected] (A.S.); [email protected] (T.C.M.A.S.); [email protected] (H.B.) 2 Institute of Molecular Biology & Bio-Technology, Bahauddin Zakariya University, Multan 60800, Pakistan 3 Department of Endocrinology, University Medical Center Groningen, University of Groningen, 9713 GZ Groningen, The Netherlands; [email protected] 4 Department of Laboratory Medicine, University Medical Center Groningen, University of Groningen, 9713 GZ Groningen, The Netherlands * Correspondence: [email protected]; Tel.: +31-(0)5-0361-2364; Fax: +31-(0)5-0361-9306 Received: 7 November 2017; Accepted: 19 December 2017; Published: 29 December 2017 Abstract: Vitamin A is required for important physiological processes, including embryogenesis, vision, cell proliferation and differentiation, immune regulation, and glucose and lipid metabolism. Many of vitamin A’s functions are executed through retinoic acids that activate transcriptional networks controlled by retinoic acid receptors (RARs) and retinoid X receptors (RXRs).The liver plays a central role in vitamin A metabolism: (1) it produces bile supporting efficient intestinal absorption of fat-soluble nutrients like vitamin A; (2) it produces retinol binding protein 4 (RBP4) that distributes vitamin A, as retinol, to peripheral tissues; and (3) it harbors the largest body supply of vitamin A, mostly as retinyl esters, in hepatic stellate cells (HSCs). -

Differentiating Neuroblastoma: a Systematic Review of the Retinoic Acid, Its Derivatives, and Synergistic Interactions
Journal of Personalized Medicine Systematic Review Differentiating Neuroblastoma: A Systematic Review of the Retinoic Acid, Its Derivatives, and Synergistic Interactions Nadiya Bayeva 1,2, Erin Coll 1,2 and Olga Piskareva 1,2,3,* 1 Cancer Bio-Engineering Group, Department of Anatomy and Regenerative Medicine, RCSI University of Medicine and Health Sciences, D02 YN77 Dublin, Ireland; [email protected] (N.B.); [email protected] (E.C.) 2 School of Pharmacy and Biomolecular Sciences, RCSI University of Medicine and Health Sciences, D02 YN77 Dublin, Ireland 3 National Children’s Research Centre, Our Lady’s Children’s Hospital Crumlin, D12 8MGH Dublin, Ireland * Correspondence: [email protected] Abstract: A neuroblastoma (NB) is a solid paediatric tumour arising from undifferentiated neuronal cells. Despite the recent advances in disease management and treatment, it remains one of the leading causes of childhood cancer deaths, thereby necessitating the development of new therapeutic agents and regimens. Retinoic acid (RA), a vitamin A derivative, is a promising agent that can induce differentiation in NB cells. Its isoform, 13-cis RA or isotretinoin, is used in NB therapy; however, its effectiveness is limited to treating a minimal residual disease as maintenance therapy. As such, research focuses on RA derivatives that might increase the anti-NB action or explores the potential synergy between RA and other classes of drugs, such as cellular processes mediators, epigenetic modifiers, and immune modulators. This review summarises the in vitro, in vivo, and clinical data of RA, its derivatives, and synergising compounds, thereby establishing the most promising RA derivatives and combinations of RA for further investigation. -

Formulation Approaches for Improved Retinoids Delivery in the Treatment of Several Pathologies T ⁎ Antónia Gonçalves, Berta N
European Journal of Pharmaceutics and Biopharmaceutics 143 (2019) 80–90 Contents lists available at ScienceDirect European Journal of Pharmaceutics and Biopharmaceutics journal homepage: www.elsevier.com/locate/ejpb Formulation approaches for improved retinoids delivery in the treatment of several pathologies T ⁎ Antónia Gonçalves, Berta N. Estevinho , Fernando Rocha LEPABE, Departamento de Engenharia Química, Faculdade de Engenharia da Universidade do Porto, Rua Dr. Roberto Frias, 4200-465 Porto, Portugal ARTICLE INFO ABSTRACT Keywords: Retinoid acid (RA) and other retinoids are extensively used as therapeutic agents in the treatment of several Cancer types of cancer and skin disorders. However, the efficiency of these medical agents is compromised due to the Controlled release unsatisfactory concentration of retinoids in the target cells/tissues. Furthermore, severe side-effects are related Encapsulation to retinoids administration. Incorporation of retinoids into carrier-based delivery systems using encapsulation Retinoids technology has been proposed in order to overcome the limitations of using free retinoids in the treatment of Skin disorders several pathologies. The present work starts exploring the competences and the difficulties of using retinoids in health care. The metabolism and the main considerations about the mechanism of action of retinoids are also discussed. The final sections are focused on the most recent studies about RA controlled delivery systems to be used in the medical field. 1. Introduction administrated), tazarotene (topically administrated), adapalene (topi- cally administrated) and fenretinide (orally administrated) [3,8,11].At Retinoids are a set of bioactive molecules which includes vitamin A last, seletinoid G (topically administrated) fits in pyranone retinoids (retinol) and its natural and synthetic derivatives. -

Retinoic Acid Receptor Alpha Drives Cell Cycle Progression and Is Associated with Increased Sensitivity to Retinoids in T-Cell Lymphoma
www.impactjournals.com/oncotarget/ Oncotarget, 2017, Vol. 8, (No. 16), pp: 26245-26255 Research Paper Retinoic acid receptor alpha drives cell cycle progression and is associated with increased sensitivity to retinoids in T-cell lymphoma Xueju Wang1,2, Surendra Dasari3, Grzegorz S. Nowakowski4, Konstantinos N. Lazaridis5,6, Eric D. Wieben5,7, Marshall E. Kadin8, Andrew L. Feldman1,*, Rebecca L. Boddicker1,* 1Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota, United States of America 2Department of Pathology, China-Japan Union Hospital of Jilin Province, Changchun, Jilin Province, China 3Division of Biomedical Statistics and Informatics, Department of Health Sciences Research, Mayo Clinic, Rochester, Minnesota, United States of America 4Division of Hematology, Department of Medicine, Mayo Clinic, Rochester, Minnesota, United States of America 5Center for Individualized Medicine, Mayo Clinic, Rochester, Minnesota, United States of America 6Division of Gastroenterology and Hepatology, Department of Medicine, Mayo Clinic, Rochester, Minnesota, United States of America 7Department of Biochemistry and Molecular Biology, Mayo Clinic, Rochester, Minnesota, United States of America 8Department of Pathology and Laboratory Medicine, Rhode Island Hospital and Department of Dermatology, Roger Williams Medical Center, Providence, Rhode Island, United States of America *These authors have contributed equally to this work Correspondence to: Andrew L. Feldman, email: [email protected] Rebecca L. Boddicker, email: [email protected] Keywords: T-cell lymphoma, retinoids, retinoic acid receptor alpha, all-trans retinoic acid, cell cycle, individualized medi- cine Received: October 04, 2016 Accepted: February 06, 2017 Published: February 17, 2017 Copyright: Wang et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC-BY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.