Idiopathic Pulmonary Fibrosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2014 05 08 BMJ Spontaneous Pneumothorax.Pdf
BMJ 2014;348:g2928 doi: 10.1136/bmj.g2928 (Published 8 May 2014) Page 1 of 7 Clinical Review CLINICAL REVIEW Spontaneous pneumothorax Oliver Bintcliffe clinical research fellow, Nick Maskell consultant respiratory physician Academic Respiratory Unit, School of Clinical Sciences, University of Bristol, Bristol BS10 5NB, UK Pneumothorax describes the presence of gas within the pleural and mortality than primary pneumothorax, in part resulting from space, between the lung and the chest wall. It remains a globally the reduction in cardiopulmonary reserve in patients with important health problem, with considerable associated pre-existing lung disease. morbidity and healthcare costs. Without prompt management Tension pneumothorax is a life threatening complication that pneumothorax can, occasionally, be fatal. Current research may requires immediate recognition and urgent treatment. Tension in the future lead to more patients receiving ambulatory pneumothorax is caused by the development of a valve-like leak outpatient management. This review explores the epidemiology in the visceral pleura, such that air escapes from the lung during and causes of pneumothorax and discusses diagnosis, evidence inspiration but cannot re-enter the lung during expiration. This based management strategies, and possible future developments. process leads to an increasing pressure of air within the pleural How common is pneumothorax? cavity and haemodynamic compromise because of impaired venous return and decreased cardiac output. Treatment is with Between 1991 and 1995 annual consultation rates for high flow oxygen and emergency needle decompression with pneumothorax in England were reported as 24/100 000 for men a cannula inserted in the second intercostal space in the and 9.8/100 000 for women, and admission rates were 16.7/100 midclavicular line. -

Pleural Effusion and Ventilation/Perfusion Scan Interpretation for Acute Pulmonary Embolus
ventricular function by radionuclide angiography during exercise in normal subjects 33. Verani MS. Myocardial perfusion imaging versus two-dimensional echocardiography: and patients with chronic coronary heart disease. J Am Coll Cardiol 1983;1:1518- comparative value in the diagnosis of coronary artery disease. J NucÃCardiol 1529. 1994;1:399-414. 29. Adam WE. Tarkowska A, Bitter F, Stauch M, Geffers H. Equilibrium (gated) 34. Foster T, McNeill AJ, Salustri A, et al. Simultaneous dobutamine stress echocardiog radionuclide ventriculography. Cardiovasc Radial 1979;2:161-173. raphy and technetium-99m SPECT in patients with suspected coronary artery disease. 30. Hurwitz RA, TrêvesS, Kuroc A. Right ventricular and left ventricular ejection fraction J Am Coll Cardiol I993;21:1591-I596. in pediatrie patients with normal hearts: first pass radionuclide angiography. Am 35. Marwick TH, D'Hondt AM, Mairesse GH, Baudhuin T, Wijins W, Detry JM, Meiin Heart J 1984;107:726-732. 31. Freeman ML, Palac R, Mason J, et al. A comparison of dobutamine infusion and JA. Comparative ability of dobutamine and exercise stress in inducing myocardial ischemia in active patients. Br Heart J 1994:72:31-38. supine bicycle exercise for radionuclide cardiac stress testing. Clin NucÃMed 1984:9:251-255. 36. Senior R, Sridhara BS, Anagnostou E, Handler C, Raftery EB, Lahiri A. Synergistic 32. Cohen JL, Greene TO, Ottenweller J, Binebaum SZ, Wilchfort SD, Kim CS. value of simultaneous stress dobutamine sestamibi single-photon-emission computer Dobutamine digital echocardiography for detecting coronary artery disease. Am J ized tomography and echocardiography in the detection of coronary artery disease. -

Spontaneous Pneumothorax in COVID-19 Patients Treated with High-Flow Nasal Cannula Outside the ICU: a Case Series
International Journal of Environmental Research and Public Health Case Report Spontaneous Pneumothorax in COVID-19 Patients Treated with High-Flow Nasal Cannula outside the ICU: A Case Series Magdalena Nalewajska 1, Wiktoria Feret 1 , Łukasz Wojczy ´nski 1, Wojciech Witkiewicz 2 , Magda Wi´sniewska 1 and Katarzyna Kotfis 3,* 1 Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70–111 Szczecin, Poland; [email protected] (M.N.); [email protected] (W.F.); [email protected] (Ł.W.); [email protected] (M.W.) 2 Department of Cardiology, Pomeranian Medical University, 70–111 Szczecin, Poland; [email protected] 3 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70–111 Szczecin, Poland * Correspondence: katarzyna.kotfi[email protected] Abstract: The coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become a global pandemic and a burden to global health at the turn of 2019 and 2020. No targeted treatment for COVID-19 infection has been identified so far, thus supportive treatment, invasive and non-invasive oxygen support, and corticosteroids remain a common therapy. High-flow nasal cannula (HFNC), a non-invasive oxygen support method, has become a prominent treatment option for respiratory failure during the SARS-CoV-2 pandemic. Citation: Nalewajska, M.; Feret, W.; HFNC reduces the anatomic dead space and increases positive end-expiratory pressure (PEEP), Wojczy´nski,Ł.; Witkiewicz, W.; allowing higher concentrations and higher flow of oxygen. Some studies suggest positive effects of Wi´sniewska,M.; Kotfis, K. HFNC on mortality and avoidance of intubation. -

The Child with Altered Respiratory Status
Path: K:/LWW-BOWDEN-09-0101/Application/LWW-BOWDEN-09-0101-016.3d Date: 3rd July 2009 Time: 16:31 User ID: muralir 1BlackLining Disabled CHAPTER 16 The Child With Altered Respiratory Status Do you remember the Diaz fam- Case History leave Lela, the baby sister, ily from Chapter 9, in which with Claudia’s mother, Selma, Jose has trouble taking his asthma medication, and head to the hospital. and in Chapter 4, in which Jose’s little sister, At the hospital the emergency department Lela, expresses her personality even as a new- nurse observes Jose sitting cross-legged and born? Jose is 4 years old and was diagnosed leaning forward on his hands. His mouth is with asthma this past fall, about 6 months ago. open and he is breathing hard with an easily Since that time Claudia, his mother, has audible inspiratory wheeze. He is using his noticed several factors that trigger his asthma subclavicular accessory muscles with each including getting sick, pollen, and cold air. breath. His respiratory rate is 32 breaths per One evening following a warm early-spring minute, his pulse is 112 beats per minutes, day, Jose is outside playing as the sun sets and and he is afebrile. Claudia explains that he the air cools. When he comes inside he was fine; he was outside running and playing, begins to cough. Claudia sets up his nebulizer and then came in and began coughing and and gives him a treatment of albuterol, which wheezing, and she gave him an albuterol lessens his coughing. Within an hour, Jose is treatment. -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -

Bronchiolitis After Lung Transplantation Lymphoid Tissue In
The Role of Intrapulmonary De Novo Lymphoid Tissue in Obliterative Bronchiolitis after Lung Transplantation This information is current as Masaaki Sato, Shin Hirayama, David M. Hwang, Humberto of September 25, 2021. Lara-Guerra, Dirk Wagnetz, Thomas K. Waddell, Mingyao Liu and Shaf Keshavjee J Immunol 2009; 182:7307-7316; ; doi: 10.4049/jimmunol.0803606 http://www.jimmunol.org/content/182/11/7307 Downloaded from References This article cites 46 articles, 4 of which you can access for free at: http://www.jimmunol.org/content/182/11/7307.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 25, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2009 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology The Role of Intrapulmonary De Novo Lymphoid Tissue in Obliterative Bronchiolitis after Lung Transplantation1 Masaaki Sato,* Shin Hirayama,* David M. Hwang,*† Humberto Lara-Guerra,* Dirk Wagnetz,* Thomas K. Waddell,* Mingyao Liu,* and Shaf Keshavjee2* Chronic rejection after lung transplantation is manifested as obliterative bronchiolitis (OB). -
An Interesting Case of Undiagnosed Pleural Effusion Case Report
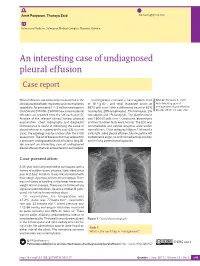
Amit Panjwani, Thuraya Zaid [email protected] Pulmonary Medicine, Salmaniya Medical Complex, Manama, Bahrain. An interesting case of undiagnosed pleural effusion Case report Pleural effusions are commonly encountered in the Investigations revealed a haemoglobin level Cite as: Panjwani A, Zaid T. clinical practise of both respiratory and nonrespiratory of 16.4 g⋅dL−1, and total leukocyte count of An interesting case of specialists. An estimated 1–1.5 million new cases in 8870 cells⋅mm−3 with a differential count of 62% undiagnosed pleural effusion. the USA and 200 000–250 000 new cases of pleural neutrophils, 28% lymphocytes, 7% monocytes, 2% Breathe 2017; 13: e46–e52. effusions are reported from the UK each year [1]. eosinophils and 1% basophils. The platelet count Analysis of the relevant clinical history, physical was 160 000 cells⋅mm−3. Creatinine, electrolytes examination, chest radiography and diagnostic and liver function tests were normal. The ECG was thoracentesis is useful in identifying the cause of unremarkable and cardiac enzymes were within pleural effusion in majority of the cases [2]. In a few normal limits. Chest radiograph (figure 1) showed a cases, the aetiology may be unclear after the initial mild, right-sided pleural effusion, blunting of the left assessment. The list of diseases that may account for costophrenic angle, no shift of mediastinal position a persistent undiagnosed pleural effusion is long [3]. and no lung parenchymal opacities. We present an interesting case of undiagnosed pleural effusion that was encountered in our hospital. R Case presentation A 33-year-old male presented to our hospital with a history of sudden-onset, pleuritic, right-sided chest pain of 2 days’ duration. -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -
Information About Lung Nodules
Information about lung nodules Introduction/procedure You have been informed that you have a nodule (or nodules) in your lung. This is a very common finding and is usually nothing to worry about. Lung nodules are often very small (too small to investigate further) and cause no symptoms. They are often found incidentally whilst having a chest x-ray or CT scan for another condition and do not affect the function of the lungs or interfere with breathing. Once discovered, it’s important to observe the appearance of the nodule(s) over time. This is done by repeating an x-ray or CT scan of your chest at certain intervals. Some nodules can be seen on chest x-ray whilst others require a CT scan to be seen clearly. The interval between the scans or x-rays is usually 3 or 6 months and is determined by your age, whether you smoke and the original size of the nodule(s). It is not the same for everyone, but we follow nationally agreed guidelines. After each scan, the images will be reviewed by the specialist chest team and the nodules measured. You will be informed of the result of the review by telephone 2-3 weeks after the scan. Most lung nodules stay exactly the same size, get smaller or even disappear over time. If a nodule has not increased in size over a series of scans or x-rays, you will be informed that no more follow up is required. Rarely a lung nodule may increase in size. If so, it’s important to determine the nature of the nodule and further investigation will be necessary. -

Editorial Note on Pulmonary Fibrosis Sindhu Sri M*
Editorial Note iMedPub Journals Archives of Medicine 2020 www.imedpub.com Vol.12 No. ISSN 1989-5216 4:e-105 DOI: 10.36648/1989-5216.12.4.e-105 Editorial Note on Pulmonary Fibrosis Sindhu Sri M* Department of Pharmaceutical Analytical Chemistry, Jawaharlal Nehru Technological University, Hyderabad, India *Corresponding author: Sindhu Sri M, Department of Pharmaceutical Analytical Chemistry, Jawaharlal Nehru Technological University, Hyderabad, India, E-mail: [email protected] Received date: July 20, 2020; Accepted date: July 26, 2020; Published date: July 31, 2020 Citation: Sindhu Sri M (2020) Editorial Note on Pulmonary Fibrosis. Arch Med Vol. 12 Iss.4: e105 Copyright: ©2020 Sindhu Sri M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Editorial Note • Lung fibrosis or pulmonary fibrosis. • Liver fibrosis. Pulmonary Fibrosis (PF) is a lung disease that happens when • Heart fibrosis. lung tissue gets harmed and scarred. Pulmonary meaning lung, • Mediastinal fibrosis. and fibrosis significance scar tissue. In the medical terminology • Retroperitoneal cavity fibrosis used to depict this scar tissue is fibrosis. The alveoli and the • Bone marrow fibrosis veins inside the lungs are responsible for conveying oxygen to • Skin fibrosis the body, including the brain, heart, and different organs. The • Scleroderma or systemic sclerosis PF group of lung diseases falls into a considerably large Hypoxia caused by pulmonary fibrosis can lead to gathering of ailments called the interstitial lung infections. At pulmonary hypertension, which, in turn, can lead to heart the point when an interstitial lung ailment incorporates scar failure of the right ventricle. -

Clarifying the Diagnosis of Post-Inflammatory Pulmonary Fibrosis: a Population-Based Study
AGORA | RESEARCH LETTER Clarifying the diagnosis of post- inflammatory pulmonary fibrosis: a population-based study To the Editor: Epidemiological studies are important in defining the distribution and burden of diseases in a population. A common method of studying interstitial lung disease (ILD) epidemiology has been the analysis of insurance and billing claims databases, such as the Commercial Claims and Encounters Database and the Medicare Supplemental and Coordination of Benefits Database. These studies rely on the accuracy of International Statistical Classification of Diseases (ICD) codes to identify a patient population of interest. Several studies have described the incidence and prevalence of ILD by methodically searching ICD codes related to ILD or by using code-based algorithms [1–6]. Post-inflammatory pulmonary fibrosis (PPF) (ICD-9-CM 515) has been categorised as a general diagnostic code used by providers for IPF, an ILD characterised by progressive parenchymal fibrosis [1, 7]. Cases of PPF have been variably included in studies of IPF epidemiology. The prevalence of PPF may be comparable or higher to that of IPF. For example, COULTAS et al. [2] reported PPF to represent 16.7% of prevalent cases of ILDs while IPF comprised 22.5% in a population-based registry. RAGHU et al.[8] analysed a large healthcare claims database spanning the period 1996–2000 and found the prevalence of PFF to be nearly 11-fold higher than that of IPF identified by “broad case definition”. To our knowledge, however, cases designated as PPF have never been fully characterised. In particular, it is unknown to what extent PPF (ICD-9-CM 515) overlaps with the diagnosis of IPF. -

Cigna Medical Coverage Policies – Radiology Chest Imaging Effective November 15, 2018
Cigna Medical Coverage Policies – Radiology Chest Imaging Effective November 15, 2018 ______________________________________________________________________________________ Instructions for use The following coverage policy applies to health benefit plans administered by Cigna. Coverage policies are intended to provide guidance in interpreting certain standard Cigna benefit plans and are used by medical directors and other health care professionals in making medical necessity and other coverage determinations. Please note the terms of a customer’s particular benefit plan document may differ significantly from the standard benefit plans upon which these coverage policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a coverage policy. In the event of a conflict, a customer’s benefit plan document always supersedes the information in the coverage policy. In the absence of federal or state coverage mandates, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage determinations in each specific instance require consideration of: 1. The terms of the applicable benefit plan document in effect on the date of service 2. Any applicable laws and regulations 3. Any relevant collateral source materials including coverage policies 4. The specific facts of the particular situation Coverage policies relate exclusively to the administration of health benefit plans. Coverage policies are not recommendations for treatment and should never be used as treatment guidelines. This evidence-based medical coverage policy has been developed by eviCore, Inc. Some information in this coverage policy may not apply to all benefit plans administered by Cigna. These guidelines include procedures eviCore does not review for Cigna.