Anaesthesia Handbook
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 7,074,961 B2 Wang Et Al
US007074961B2 (12) United States Patent (10) Patent No.: US 7,074,961 B2 Wang et al. (45) Date of Patent: Jul. 11, 2006 (54) ANTIDEPRESSANTS AND THEIR 6.211,171 B1 4/2001 Sawynok et al. ANALOGUES AS LONG-ACTING LOCAL 6,545,057 B1 4/2003 Wang et al. ANESTHETCS AND ANALGESCS 2001/0036943 A1 11/2001 Coe et al. (75) Inventors: Ging Kuo Wang, Westwood, MA (US); FOREIGN PATENT DOCUMENTS Peter Gerner, Weston, MA (US); Donald K. Verrecchia, Winchester, MA CH 534124 A 2, 1973 (US) WO WO95/17903 A1 7, 1995 WO WO95/1818.6 A1 7, 1995 (73) Assignee: The Brigham and Women's Hospital, WO WO 99.59.598 A1 11, 1999 Inc., Boston, MA (US) WO WO O2/060870 A2 8, 2002 (*) Notice: Subject to any disclaimer, the term of this OTHER PUBLICATIONS patent is extended or adjusted under 35 U.S.C. 154(b) by 451 days. Luo et al., Xenobiotica, vol. 25, No. 3, pp. 291-301, 1995.* (21) Appl. No.: 10/117,708 Ehlert et al., The Interaction of Amitriptyline, Doxepin, Imipramine and Their N-Methyl Quaternary Ammonium (22) Filed: Apr. 4, 2002 Derivatives with Subtypes of Muscarinic Receptors in Brain (65) Prior Publication Data and Heart, The Journal of Pharmacology and Experimental Therapeutics, Apr. 1990, vol. 253, No. 1, pp. 13–19. US 2003/00968.05 A1 May 22, 2003 Gerner, P., et al., Anesthesiology (2002) 96:1435–42. Related U.S. Application Dat e pplication Uata Khan, M.A., et al., Anesthesiology (2002) 96:109–16. (63) stripps'965,138, filed on Sep. -

The Femoral Nerve Block Characteristics Using Ropivacaine 0.2% Alone, with Epinephrine, Or with Lidocaine and Epinephrine
SCIENTIFIC ARTICLES THE FEMORAL NERVE BLOCK CHARACTERISTICS USING ROPIVACAINE 0.2% ALONE, WITH EPINEPHRINE, OR WITH LIDOCAINE AND EPINEPHRINE A.M. TAHA1,2 AND A.M. ABD-ELmaKSOUD31* Keywords: anesthetic techniques, regional, femoral; anaesthetics local, ropivacaine; equipment, ultrasound machines. Abstract Background: The objective of this study was to evaluate the femoral nerve block characteristics (onset, success rate and duration) using ropivacaine 0.2% alone; with epinephrine, or with lidocaine and epinephrine compared with that using ropivacaine 0.5%. Methods: Ninety six patients were included in this prospective controlled double blind study and were randomly allocated into four equal groups (n=24). All the patients received ultrasound guided femoral nerve block using 15 ml of either ropivacaine 0.5% (group 1), ropivacaine 0.2% (group 2), ropivacaine 0.2% with epinephrine (group 3) and ropivacaine 0.2% with lidocaine and epinephrine (group 4). The block onset, success rate and duration were recorded. Results: The motor onset was significantly delayed in group 2 (compared with the other three groups) and in group 3 (compared with group 4). However, the block success rate and duration were comparable in the four groups. Conclusion: In femoral nerve block, ropivacaine 0.2% may have a comparable success rate and duration to ropivacaine 0.5% but with a remarkably delayed motor onset that may be improved by adding epinephrine. Addition of lidocaine may further accelerate the motor onset. Introduction The femoral nerve block (FNB) is a commonly indicated block, and ropivacaine is a widely used long acting local anesthetic (LA)1,2. Peripheral nerve blocks can provide excellent anesthesia and postoperative analgesia 3,4. -

Components of Respiratory Depression After Narcotic Premedication in Adolescents
COMPONENTS OF RESPIRATORY DEPRESSION AFTER NARCOTIC PREMEDICATION IN ADOLESCENTS R. KNILL*, J.F. Coscnowr P. M. OLLEY,AND H. LEVISON N~d~COTIC ACENTS are potent depressants of ventilation. 1-5 Although this effect is generally assumed to result from decreased output of the central respiratory "'centres," some of the effect could be due to direct action on the ventilatory apparatus itself, by increasing respiratory impendance. For example, both morphine and meperidine can cause bronchoconstriction;" furthermore they can increase the tonic activity of abdominal and intercostal muscles, r-l~ The mechanical effects of this increase in abdominal wall tone have not been assessed after thera- peutic doses of these agents, but large doses of narcotics administered intravenously produce board-like rigidity of the abdominal wall r-lo and markedly decrease total respiratory compliance? As the magnitude of this effect appears to be dose related 1~ it may well be present to a lesser extent after therapeutic doses of these agents. The purpose of this work was to determine whether the ventilatory depression associated with morphine and a meperidine-phenothiazine mixture is solely the result of impairment of the neuromuscular or force-generating mechanisms, or is in part due to increased impedance of the ventilatory pump. Even small increases in ventilatory load with narcotics probably contribute to ventilatory depression, as load compensation is poor when central neural mechanisms are pharmacologi- cally imp aired. 11,1a The conventional technique for examining the effect of narcotics on ventilation is to apply rebreathing and steady-state.methods before and after medication, to measure changes in minute ventilation (V~) and tidal volume (VT).13,~4 However, these measurements depend on both central output and the properties of the ventilatory apparatus, ~,16 without distinction between them. -
Journal Watch 1805 TCCC.Pdf
TCCC Journal Watch May 2018 Abou El Fadl M, O’Phelan K: Management of traumatic brain injury: an update. Neurosurg Clin N Am 2018;29:213-221 Abraham P,Russell D, Huffman S, et al: Army combat medic resilience: the process of forging loyalty. Mil Med 2018;183:364-370 Adravanti P, Di Salvo E, Calafiore G, et al: A prospective, randomized, comparative study of intravenous alone and combine intravenous and intraarticular administration of tranexamic acid in primary total knee replacement. Arthoplast Today 2017;4:85-88 Aggarwal N, Brower R, Hager D, et al: Oxygen exposure resulting in arterial oxygen tensions above the protocol goal was associated with worse clinical outcomes in acute respiratory distress syndrome. Crit Care Med 2018;46:517-524 Agimi Y, Regasa L, Ivins B, et al: Role of Department of Defense policies in identifying traumatic brain injuries among deployed US Service members 2001- 2016. Aiolfi A, Benjamin E, Recinos G, et al: Air versus ground transportation in isolated severe head trauma: a national trauma bank study. J Emerg Med 2018;54:328- 334 Aji Y, Apriawan T, Bajamal A: Traumatic supra- and infra-tentorial extradural hematoma: case series and literature review. Asian J Neurosurg 2018;13:453- 457 Akbari E, Safari S, Hatamabadi H: The effect of fibrinogen concentrate and fresh frozen plasma on the outcome of patients with acute traumatic coagulopathy: a quasi-experimental study. Am J Emerg Med 2018;Epub ahead of print. Aries M, Donnelly J: Brain oxygenation optimization after severe traumatic brain injury: an ode to preventing brain hypoxia. Crit Care Med 2018;46:e350 Armstrong R: Visual problems associated with traumatic brain injury. -

Ultrasound Guided Femoral Nerve Block
Ultrasound Guided Femoral Nerve Block Michael Blaivas, MD, FACEP, FAIUM Clinical Professor of Medicine University of South Carolina School of Medicine AIUM, Third Vice President President, Society for Ultrasound Medical Education Past President, WINFOCUS Editor, Critical Ultrasound Journal Sub-specialty Editor, Journal of Ultrasound in Medicine Emergency Medicine Atlanta, Georgia [email protected] Disclosures • No relevant disclosures to lecture Objectives • Discuss anatomy of femoral nerve • Discuss uses of femoral nerve block classically and 3-in-1 variant • Discuss technique of femoral nerve blockade under ultrasound • Discuss pitfalls and potential errors Femoral Nerve Block Advantages • Many uses of regional nerve blocks • Avoid narcotics and their complications • Allow for longer term pain control • Can be used in patients unfit for sedation – Poor lung health – Hypotensive – Narcotic dependence or sensitivity Femoral Nerve Blocks • Wide variety of potential indications for a femoral nerve block – Hip fracture – Knee dislocation – Femoral fracture – Laceration repair – Burn – Etc. Nerve Blocks in Community vs. Academic Setting • Weekend stays • Night time admissions • Time to get consult and clear • Referral and admission patters • All of these factors can lead to patients spending considerable time prior to OR • Procedural sedation vs. block Femoral Nerve Blocks • Several basic principles with US also • Specialized needles +/- • No nerve stimulator • Can see nerve directly and inject directly around target nerve or nerves • Only -
Scope of Practice Statements
Scope of Practice Statements Emergency Medical Services Authority California Health and Human Services Agency EMSA # 300 November 2017 HOWARD BACKER, MD, MPH, FACEP DIRECTOR DANIEL R. SMILEY CHIEF DEPUTY DIRECTOR SEAN TRASK DIVISION CHIEF EMSA # 300 Released November 2017 EMSA #300 • Page 1 Table of Contents Introduction ........................................................................................................................................... 4 The EMS Authority ................................................................................................................................ 4 Local EMS Agencies ............................................................................................................................. 4 California EMS Personnel Levels .......................................................................................................... 4 Reading the Scope of Practice Pages .................................................................................................. 5 Airway and Breathing ............................................................................................................................ 6 Airway Suctioning .............................................................................................................................. 7 Automatic Transport Ventilator .......................................................................................................... 8 Bag Valve Mask – BVM .................................................................................................................... -

Frequently Asked Questions (Faqs)
Frequently Asked Questions (FAQs) What is hyperbaric oxygen therapy? Commonly referred to as HBOT, hyperbaric oxygen therapy enhances the body’s natural healing process by delivering oxygen under pressure, which increases the oxygen content in the blood, plasma, cerebral spinal fluid, and other body tissues. There are two basic types of HBOT—hard HBOT and mild HBOT. With hard HBOT, treatments are delivered in a hard-sided chamber typically at pressures greater than 1.5 ATA and using 100% oxygen. 100% oxygen is extremely flammable; therefore, hard HBOT involves managing the risk of explosion. Another concern with hard HBOT is oxygen toxicity. While hard HBOT with 100% oxygen results in greater oxygen saturation in the tissues, many conditions respond better to mild HBOT. In clinical trials to date, there has been virtually no difference in clinical outcome between mild HBOT and hard HBOT. Mild HBOT refers to hyperbaric oxygen therapy at lower pressures, typically 1.5 ATA or below, and the use of an oxygen concentrator delivering 90-95% oxygen inside a portable soft-sided chamber. Mild HBOT has no known safety risks with fire or toxicity, and it is substantially less expensive. Our facility provides concentrated oxygen (90-95%) at 1.3 ATA—(Mild HBOT)a highly effective combination clinically, and without the risk of oxygen toxicity or explosion, as 100% oxygen is avoided. How should I expect mild HBOT to feel? You will be seated or lying down inside the chamber, relaxing comfortably in your own clothing, as you breathe concentrated oxygen (90-95% O2) through a facemask. -
Stratus 5 Oxygen Concentrator User Manual
USER MANUAL OXYGEN CONCENTRATOR CE 0123 v2.1 STR1005 User Manual Symbol Key MARK DEFINITION II Power on Power off Follow Instruction for Use No smoking Caution, consult accompanying documents. Class Ⅱ (Double Insulated) Type BF Applied Part CE certification mark 0123 AC Power Stacking Limit by Number This Way Up Fragile, handle with care Keep dry Temperature limit No open flames IIPP2211 IP21 Drip Proof Equipment Consult instructions for use Stand-by Warning, electricity 2 v2.1 STR1005 User Manual 3 v2.1 STR1005 User Manual SPECIAL NOTES • Please read this manual carefully before using this product and save it for future reference. • If you need assistance with this manual, Please contact your local DME or home health provider • The Stratus 5 is a prescription device. Use only the liter setting prescribed for you. • It is always recommended for critically ill patients to have a backup oxygen source in case of malfunction. • If patient experiences an adverse reaction contact physician or call 911 immediately. • In case of machine malfunction, contact the home medical equipment provider; do not attempt to disassemble the Stratus 5. • The Stratus 5 is not intended as life support, it is for supplemental oxygen use only. Patients with special needs may be unable to understand the alarm features and should be well supervised while using an oxygen concentrator. • The Stratus 5 is for single patient use. • Do not adjust the flowmeter float beyond the red line position. Long-term use out of range will reduce the efficiency of the oxygen generator. SAFETY NOTICE Please read the following information carefully before Operating the oxygen concentrator Warning Special attention should be paid to reducing the risk of fire when using oxygen therapy. -
The Emergency Severity Index
The Emergency Severity Index Jassin M. Jouria, MD Dr. Jassin M. Jouria is a medical doctor, professor of academic medicine, and medical author. He graduated from Ross University School of Medicine and has completed his clinical clerkship training in various teaching hospitals throughout New York, including King’s County Hospital Center and Brookdale Medical Center, among others. Dr. Jouria has passed all USMLE medical board exams, and has served as a test prep tutor and instructor for Kaplan. He has developed several medical courses and curricula for a variety of educational institutions. Dr. Jouria has also served on multiple levels in the academic field including faculty member and Department Chair. Dr. Jouria continues to serve as a Subject Matter Expert for several continuing education organizations covering multiple basic medical sciences. He has also developed several continuing medical education courses covering various topics in clinical medicine. Recently, Dr. Jouria has been contracted by the University of Miami/Jackson Memorial Hospital’s Department of Surgery to develop an e- module training series for trauma patient management. Dr. Jouria is currently authoring an academic textbook on Human Anatomy & Physiology. Abstract One of the main challenges encountered by emergency departments is determining how to appropriately triage patients. Although some systems only take into account a single determining factor, the Agency for Healthcare Research and Quality promotes a system that considers both the acuity of patients’ health care problems as well as the number of resources needed to treat them. This system provides emergency departments with a unique tool to ensure that the most at-risk patients are being seen and treated in the most efficient manner. -

An Evidence-Based Guideline for the Pre-Operative Sedation of Children
Journal of Pediatrics and Neonatal Care An Evidence-Based Guideline for the Pre-Operative Sedation of Children Abstract Review Article There are numerous sedative pharmacological agents currently administered to Volume 2 Issue 6 - 2015 children as premedicants to facilitate the induction of anaesthesia. When pre- operative sedation is required, selection of the appropriate drug is imperative to Deborah M Fradkin*, Victoria L Scott- provide adequate anxiolysis whilst minimising unwanted side effects. We review Warren, Rita Vashisht and Sian E Rolfe the literature regarding the merits and limitations of the commonly used agents and suggest evidence based practical guidance. For the anxious but cooperative Department of Paediatric Anaesthesia, Royal Manchester Children’s Hospital, England child, oral midazolam is often adequate; however with more anxious younger and uncooperative children, combined oral midazolam and ketamine is more *Corresponding author: DM. Fradkin, Department of effective. Other oral benzodiazepines and oral clonidine all have their role when Paediatric Anaesthesia, Royal Manchester Children’s used in the appropriate circumstances. Intranasal clonidine is useful in the child Hospital, Oxford Road, Manchester, M13 9WL, England, Tel: refusing oral medication. Intramuscular ketamine should be reserved for extreme 0161 701 1264; Email: circumstances, administered only by anaesthetists experienced in its use, with full monitoring and resuscitative equipment immediately available. Received: August 15, 2015 | Published: September -
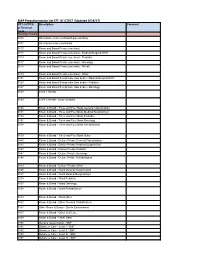
MAP Preauthorization List EFF: 8/1/2017 (Updated 8/24/17)
MAP Preauthorization List EFF: 8/1/2017 (Updated 8/24/17) CPT, HCPCS Description Comment or Revenue Code Revenue Codes 0100 All inclusive room and board plus ancillary 0101 All inclusive room and board 0110 Room and Board Private (one bed) 0111 Room and Board Private (one bed) - Medical/Surgical/GYN 0113 Room and Board Private (one bed) - Pediatric 0117 Room and Board Private (one bed) - Oncology 0118 Room and Board Private (one bed) - Rehab 0119 Room and Board Private (one bed) - Other 0121 Room and Board Semiprivate (two beds) - Medical/Surgical/GYN 0123 Room and Board Semiprivate (two beds) - Pediatric 0127 Room and Board Semiprivate (two beds) - Oncology 0128 Level 1 Rehab 0129 Level 2 Rehab - acute complex 0130 Room & Board - Three and Four Beds General Classification 0131 Room & Board - Three and Four Beds Medical/Surgical/Gyn 0133 Room & Board - Three and Four Beds Pediatric 0137 Room & Board - Three and Four Beds Oncology 0138 Room & Board - Three and Four Beds Rehabilitation 0139 Room & Board - Three and Four Beds Other 0140 Room & Board - Deluxe Private General Classification 0141 Room & Board - Deluxe Private Medical/Surgical/Gyn 0143 Room & Board - Deluxe Private Pediatric 0147 Room & Board - Deluxe Private Oncology 0148 Room & Board - Deluxe Private Rehabilitation 0149 Room & Board - Deluxe Private Other 0150 Room & Board - Ward General Classification 0151 Room & Board - Ward Medical/Surgical/Gyn 0153 Room & Board - Ward Pediatric 0157 Room & Board - Ward Oncology 0158 Room & Board - Ward Rehabilitation 0159 Room & Board - -
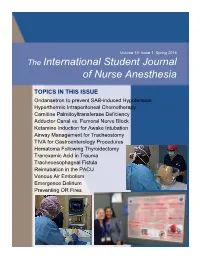
The International Student Journal of Nurse Anesthesia
Volume 15 Issue 1 Spring 2016 The International Student Journal of Nurse Anesthesia TOPICS IN THIS ISSUE Ondansetron to prevent SAB-induced Hypotension Hyperthermic Intraperitoneal Chemotherapy Carnitine Palmitoyltransferase Deficiency Adductor Canal vs. Femoral Nerve Block Ketamine Induction for Awake Intubation Airway Management for Tracheostomy TIVA for Gastroenterology Procedures Hematoma Following Thyroidectomy Tranexamic Acid in Trauma Tracheoesophageal Fistula Reintubation in the PACU Venous Air Embolism Emergence Delirium Preventing OR Fires INTERNATIONAL STUDENT JOURNAL OF NURSE ANESTHESIA Vol. 15 No. 1 Spring 2016 Editor Vicki C. Coopmans, CRNA, PhD Associate Editor Julie A. Pearson, CRNA, PhD Editorial Board Laura Ardizzone, CRNA, DNP Memorial Sloan Kettering Cancer Center; NY, NY MAJ Sarah Bellenger, CRNA, MSN, AN Darnall Army Medical Center; Fort Hood, TX Laura S. Bonanno, CRNA, DNP Louisiana State University Health Sciences Center Carrie C. Bowman Dalley, CRNA, MS Georgetown University Marianne Cosgrove, CRNA, DNAP Yale-New Haven Hospital School of Nurse Anesthesia LTC Denise Cotton, CRNA, DNAP, AN Winn Army Community Hospital; Fort Stewart, GA Janet A. Dewan, CRNA, PhD Northeastern University Kären K. Embrey CRNA, EdD University of Southern California Millikin University and Rhonda Gee, CRNA, DNSc Decatur Memorial Hospital Marjorie A. Geisz-Everson CRNA, PhD University of Southern Mississippi Johnnie Holmes, CRNA, PhD Naval Hospital Camp Lejeune Anne Marie Hranchook, CRNA, DNP Oakland University-Beaumont Donna Jasinski,