Concussion Management Protocol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clemson Area Chamber of Commerce
J ec W t s Creek e P C s R w St r ro d e M e C l o t B r Ln ri m CENTRAL r u i l s er d u S t a S g Willo P t m w Ct e C St College Ave u R H l e S eath t d d m Hill Dr C e S 00.25 0.5 1 Mile ataw R s r bah n R o P n d le R i by L S a a n i a s n R le D Dr n S e M e a d O g n t L g te in y o a Dr e Dr k n e a r e W Trl F t Br a D c or n a r y d Rd y g u D e o r t r Tw M D V 00.25 0.5 1 KM elve Mil S r H icke e rk te ea ry Dr Pa son s m a t Rd e E C h l d H SOUTH CAROLINA e C l R a M o r ra n pe D nt Dr n t D Ce S o T r ld O a r 93 O ld to n b C Ln n or e y C Legend ntr H i al am r WindsorCt Rd Dr ilto n W Fern Cir Kipp Ln es We Mountain t L llin y City Hall....................................... n gt a View on W Clemson University............... -

NC State Vs Clemson (10/26/1985)
Clemson University TigerPrints Football Programs Programs 1985 NC State vs Clemson (10/26/1985) Clemson University Follow this and additional works at: https://tigerprints.clemson.edu/fball_prgms Materials in this collection may be protected by copyright law (Title 17, U.S. code). Use of these materials beyond the exceptions provided for in the Fair Use and Educational Use clauses of the U.S. Copyright Law may violate federal law. For additional rights information, please contact Kirstin O'Keefe (kokeefe [at] clemson [dot] edu) For additional information about the collections, please contact the Special Collections and Archives by phone at 864.656.3031 or via email at cuscl [at] clemson [dot] edu Recommended Citation University, Clemson, "NC State vs Clemson (10/26/1985)" (1985). Football Programs. 178. https://tigerprints.clemson.edu/fball_prgms/178 This Book is brought to you for free and open access by the Programs at TigerPrints. It has been accepted for inclusion in Football Programs by an authorized administrator of TigerPrints. For more information, please contact [email protected]. FROM ONE CHAMPION TO ANOTHER . Louis P. Batson Company backs the Clemson Tigers. Louis P. Batson Company — International Champions in Textile, Plastics, Paper Mill and Industrial Machinery. #1 in quality tfr service dependability For your machinery, accessory, spare parts and service, call Batson first everytime. Company Home Office: Box 3978 • Greenville, S. C. 29608 Area 803 242-5262 I Table of Contents Clemson vs. N.C. State 73 Andy Newell October 26, 1985 Memorial Stadium Clemson's punter did not play any kind of football during 1982 and 1983 as he played The Textile Bowl baseball on the junior college level. -

Clemson Tigers 1 2020-21 WOMEN’S BASKETBALL
2020-21 WOMEN’S BASKETBALL WATCH / LISTEN GAME 19 | WAKE FOREST | 12:00 PM WATCH ACC Network Clemson Women’s Basketball Wake Forest Women’s Basketball Sam Ravech, Monica McNutt Head Coach: Amanda Butler Head Coach: Jen Hoover Career Record: 268-203 Career Record: 143-161 LISTEN Record at Clemson: 38-44 Record at Wake Forest: 124-148 Clemson Tigers Network (WCCP 105.5) Series History: Clemson leads, 51-25 William Qualkinbush, Sarah-Jo Lawrence Last Meeting: Clemson, 69-66 (@ Wake Forest; January 31, 2021) SCHEDULE OPENING TIP Overall: 10-8 • Home: 7-2 • Away 3-6 • Neu: 0-0 • Clemson returns to the floor on Sunday afternoon, after falling to #4 NC State, Date Opponent Time/Result 86-65, on Thursday afternoon in Raleigh, the Tigers’ final road game of the Nov. 25 FURMAN ..................................W, 83-43 2020-21 regular season. Nov. 27 PRESBYTERIAN........................W, 92-47 Nov. 30 @ Charlotte ...............................W, 80-73 • Delicia Washington led the Tigers with 24 points, 8 rebounds and 4 assists, Dec. 2 MERCER ..................................W, 67-54 her 11th-consecutive game in double figures since returning from an ankle in- Dec. 6 COLLEGE OF CHARLESTON .....W, 87-65 Dec. 10 *@ Virginia .................................W, 71-55 jury in mid-December. Dec. 13 *@ Pittsburgh .............................L, 71-80 • Amari Robinson finished one rebound shy of a double-double on Thursday Dec. 17 *FLORIDA STATE ......................W, 72-69 Dec. 20 *NOTRE DAME ..........................W, 78-55 night, with 11 points and 9 boards. Jan. 3 *@ Miami ....................................L, 71-80 • Sunday’s game is Clemson’s annual Play4Kay game. Both teams will wear Jan. -

Crystal Report
2014 ANNUAL UPDATE REPORT CLEMSON UNIVERSITY OFFICE OF RISK MANAGEMENT IS Local # Improvement Description Facility City Policy Number Survey Date Rep Cost I CABIN #1 82 CAMP LONG RD. CAMP LONG AIKEN F1200200-00007 1/24/2013 175,598 I CABIN #2 82 CAMP LONG RD. CAMP LONG AIKEN F1200200-00008 1/24/2013 121,398 I CABIN #3 82 CAMP LONG RD. CAMP LONG AIKEN F1200200-00009 1/24/2013 175,598 I CABIN #4 82 CAMP LONG RD. CAMP LONG AIKEN F1200200-00011 1/24/2013 112,601 I CABIN #5 82 CAMP LONG RD. CAMP LONG AIKEN F1200200-00012 1/24/2013 175,598 I CABIN #6 82 CAMP LONG RD. CAMP LONG AIKEN F1200200-00013 1/24/2013 175,598 I CABIN #7 82 CAMP LONG RD. CAMP LONG AIKEN F1200200-00014 1/24/2013 175,598 I 9606 - MORRIS LODGE-ASSEMBLY CAMP LONG AIKEN F1200200-00020 1/24/2013 455,805 - CAMP LONG I 9607- NOAH'S ARK - CAMP LONG CAMP LONG AIKEN F1200200-00030 1/24/2013 330,083 I 9609 - JONES JUNGLE- SLEEPING CAMP LONG AIKEN F1200200-00040 1/24/2013 86,848 CABIN-CAMP LONG I 9611-BAKER'S BARN-SLEEPING CAMP LONG AIKEN F1200200-00050 1/24/2013 196,848 CABIN-CAMP LONG I 9612-DINING HALL CAMP LONG AIKEN F1200200-00060 1/24/2013 1,050,152 KITCHEN&CRAFT SHOP-CAMP LONG I 9614-ROGER'S ROOST SLEEPING CAMP LONG AIKEN F1200200-00080 1/24/2013 179,370 CABIN-CAMP LONG I 9617 - BARN - CAMP LONG CAMP LONG AIKEN F1200200-00110 1/24/2013 133,802 I #9618 - CAMP LONG LIBRARY 82 CAMP LONG AIKEN F1200200-00121 1/24/2013 234,481 CAMP LONG RD. -

South Carolina Vs Clemson (11/20/1976)
Clemson University TigerPrints Football Programs Programs 1976 South Carolina vs Clemson (11/20/1976) Clemson University Follow this and additional works at: https://tigerprints.clemson.edu/fball_prgms Materials in this collection may be protected by copyright law (Title 17, U.S. code). Use of these materials beyond the exceptions provided for in the Fair Use and Educational Use clauses of the U.S. Copyright Law may violate federal law. For additional rights information, please contact Kirstin O'Keefe (kokeefe [at] clemson [dot] edu) For additional information about the collections, please contact the Special Collections and Archives by phone at 864.656.3031 or via email at cuscl [at] clemson [dot] edu Recommended Citation University, Clemson, "South Carolina vs Clemson (11/20/1976)" (1976). Football Programs. 125. https://tigerprints.clemson.edu/fball_prgms/125 This Book is brought to you for free and open access by the Programs at TigerPrints. It has been accepted for inclusion in Football Programs by an authorized administrator of TigerPrints. For more information, please contact [email protected]. LD- P/A^H I o Med, pi |^c> E^-Ll cki fJ FRIED CHICKEN Ideally situated to save you time and money. When Eastern meets your distribution needs, you have an experienced group working for you in two ideal locations: Greenville, South Carolina, and Jacksonville, Florida. The recent addition of two brand new distribution centers in Imeson Park at Jacksonville gives us total floor space of 1 ,1 67,000 sq. ft., with more projected. Our materials handling and warehouse maintenance equipment is the finest. Our personnel hand picked. -

Tales of Clemson, 1936-1940 Accreditation with ABET and CAC Arthur V
FEATURES The Winning SUMMER 2002 Ticket 12 VOL. 55, NO. 3 Meet a group of guys who define DEPARTMENTS “Clemson entrepreneurship.” PRESIDENT’S Perfect Balance 14 VIEW PAGE 2 See what makes these five alumni truly “distinguished.” WORLD VIEW PAGE 4 CALENDAR One World 18 PAGE 26 What’s this generation of Clemson students coming to? LIFELONG CONNECTIONS PAGE 28 STUDENT LIFE Growing Up with PAGE 30 Clemson 21 Find out how R.F. Poole CLASSMATES PAGE 32 established his place in the University’s history. NEWSMAKERS PAGE 44 COMMITMENT Just Look 22 PAGE 46 You don’t have to look far to find art on the TAPS PAGE 48 Clemson campus. DAVE LEWIS DAVE ‘Friday Flyer’ Cover and background photographs by Darryl Glubczynski President’s View Changing public service Why tamper with success? There’s a lot of conversation at Clemson about that ques- tion. Be certain of one thing: Clemson will question its success and make changes that will foster success in the future. Recently, success and change were the topics of a four-hour conversation at the Madren Center. More than 100 Clemson faculty members, staff and students attended a Public Service Activities summit on improving the University’s connection with South Carolina’s communities. In my opening comments at the summit, I said that I believe the land-grant univer- sity model may be the best idea America ever had. It has fundamentally changed our country in the most positive ways. Its success, however, may have hindered our ability to evolve. When you hit a home run, you’re not inclined to change anything. -

Virginia Vs Clemson (11/16/1974)
Clemson University TigerPrints Football Programs Programs 1974 Virginia vs Clemson (11/16/1974) Clemson University Follow this and additional works at: https://tigerprints.clemson.edu/fball_prgms Materials in this collection may be protected by copyright law (Title 17, U.S. code). Use of these materials beyond the exceptions provided for in the Fair Use and Educational Use clauses of the U.S. Copyright Law may violate federal law. For additional rights information, please contact Kirstin O'Keefe (kokeefe [at] clemson [dot] edu) For additional information about the collections, please contact the Special Collections and Archives by phone at 864.656.3031 or via email at cuscl [at] clemson [dot] edu Recommended Citation University, Clemson, "Virginia vs Clemson (11/16/1974)" (1974). Football Programs. 114. https://tigerprints.clemson.edu/fball_prgms/114 This Book is brought to you for free and open access by the Programs at TigerPrints. It has been accepted for inclusion in Football Programs by an authorized administrator of TigerPrints. For more information, please contact [email protected]. CLEMS&N TIGERS THE VIRGINIA GAMEtfrNOV. 16, 1974*1:00 P. M.ffrCLEMSON MEMORIAL STADIUM*$ 1 .00 Ideally situated to save you time and money. When Eastern meets your distribution needs, you have an experienced group working for you in two ideal locations: Greenville, South Carolina, and Jacksonville, Florida. The recent addition of two brand new distribution centers in Imeson Park at Jacksonville gives us total floor space of 1,167,000 sq.ft., with more projected. Ourmaterials handling and warehouse maintenance equipment is the finest. Our personnel hand picked. Our responsiveness to your instructions quick enough to move goods on a same-day basis. -

South Carolina Vs Clemson (11/25/1978)
Clemson University TigerPrints Football Programs Programs 1978 South Carolina vs Clemson (11/25/1978) Clemson University Follow this and additional works at: https://tigerprints.clemson.edu/fball_prgms Materials in this collection may be protected by copyright law (Title 17, U.S. code). Use of these materials beyond the exceptions provided for in the Fair Use and Educational Use clauses of the U.S. Copyright Law may violate federal law. For additional rights information, please contact Kirstin O'Keefe (kokeefe [at] clemson [dot] edu) For additional information about the collections, please contact the Special Collections and Archives by phone at 864.656.3031 or via email at cuscl [at] clemson [dot] edu Recommended Citation University, Clemson, "South Carolina vs Clemson (11/25/1978)" (1978). Football Programs. 136. https://tigerprints.clemson.edu/fball_prgms/136 This Book is brought to you for free and open access by the Programs at TigerPrints. It has been accepted for inclusion in Football Programs by an authorized administrator of TigerPrints. For more information, please contact [email protected]. FICIAL PROGRAM • MEMORIAL STADIUM • NOVEMBER 25, 1078 OUtH CAROLINA Eastern Distribution is people who Icnow how to handle things People who can get anything at all from one place to another on the right timetable, and in perfect condition. Murphy MacLean, Vice President/Flor ida, and Sherry Herren, Vice President/S. C. Eastern Distribution Office Manager Dianne Moore, Sales Representative Sherry Turner, and Controller Carrol Garrett Yes, the Eastern people on Harold Segars' Greenville, S. C, and Jacksonville, Fla., distribution team get things done, whether they're arranging the same-day movement of something you want out in a hurry, or consolidating loads to save you money through lower rates. -
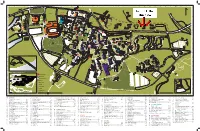
Campus Map 2018.Indd
ABCDEFGHIJKLMNOPQRSTUVWXY Z AA BB CC DD EE FF GG HH II nter 1 Ce 1 s y. 93 48 llnes d. S.C. Hw . We Cox Blv d Col . lv d er T To Downtown n l lt B a Wa M e ss g e al e tn i Fi n A n v e e . tdoor t . u n d O e C ily R INTRAMURAL 2 m 102 2 Fa FIELDS ow Ravenel Rd. n 89 n o S INTRAMURAL 114 Dan o s ie t FIELDS 85 l Dr. 27 m ia M l . 73 l t i H 99 S 57 eism n an a N W St. S 3 56 W rm 3 e . a h 3 C lt S . er H 72 132 w y T t . y i . 35 il C . c d 40 111 a R o M 7 F r M x 6 g e t 49 n B i e w 13 l 4 o 112 M 4 im 77 BOWMAN vd R 84 r 11 ’s e FIELD . P n e 122 S . om 91 C d. W H to 121 v 86 w l y . B 9 125 62 3 n 5 61 a 5 88 C m 60 26 alhoun D r 107 r. a d v 124 e 95 Bl 31 94 P 21 ial . 128 n 110 n N M e t s 32 n r. 20 e M a D C 6 l 6 n i u S 34 o 25 h l 83 C 55 Ca Walt S.C. -

South Carolina Vs Clemson (11/17/1990)
Clemson University TigerPrints Football Programs Programs 1990 South Carolina vs Clemson (11/17/1990) Clemson University Follow this and additional works at: https://tigerprints.clemson.edu/fball_prgms Materials in this collection may be protected by copyright law (Title 17, U.S. code). Use of these materials beyond the exceptions provided for in the Fair Use and Educational Use clauses of the U.S. Copyright Law may violate federal law. For additional rights information, please contact Kirstin O'Keefe (kokeefe [at] clemson [dot] edu) For additional information about the collections, please contact the Special Collections and Archives by phone at 864.656.3031 or via email at cuscl [at] clemson [dot] edu Recommended Citation University, Clemson, "South Carolina vs Clemson (11/17/1990)" (1990). Football Programs. 213. https://tigerprints.clemson.edu/fball_prgms/213 This Book is brought to you for free and open access by the Programs at TigerPrints. It has been accepted for inclusion in Football Programs by an authorized administrator of TigerPrints. For more information, please contact [email protected]. ^outnfCaKoJina Seniors^ ^cuncefiwMvmo^w ndJStacy \ meStwIiiaiiStaaiu^ ^November, PICTURES ARE WORTH A THOUSAND WORDS But at -"IpptT^jt we know your bottom line is what really counts. That's why we represent the world's leading textile machinery manufacturers and provide customers with the most high-tech equipment available to the market. We offer total support with complete service, technical assistance, and on-time spare parts. After all, you want that bottom line black- not red. Got the picture? DREF 3 FRICTION SPINNING MACHINE delivers yarn to 330 ypm. FEHRER K-21 RANDOM CARDING MACHINE has weight range 2 10-200 g/m , . -
South Carolina Vs Clemson (11/19/1988)
Clemson University TigerPrints Football Programs Programs 1988 South Carolina vs Clemson (11/19/1988) Clemson University Follow this and additional works at: https://tigerprints.clemson.edu/fball_prgms Materials in this collection may be protected by copyright law (Title 17, U.S. code). Use of these materials beyond the exceptions provided for in the Fair Use and Educational Use clauses of the U.S. Copyright Law may violate federal law. For additional rights information, please contact Kirstin O'Keefe (kokeefe [at] clemson [dot] edu) For additional information about the collections, please contact the Special Collections and Archives by phone at 864.656.3031 or via email at cuscl [at] clemson [dot] edu Recommended Citation University, Clemson, "South Carolina vs Clemson (11/19/1988)" (1988). Football Programs. 199. https://tigerprints.clemson.edu/fball_prgms/199 This Book is brought to you for free and open access by the Programs at TigerPrints. It has been accepted for inclusion in Football Programs by an authorized administrator of TigerPrints. For more information, please contact [email protected]. ^MGE YOU WORTHY OF THE BEST? Batson is the exclusive U.S. agent for textile equipment from the leading textile manufacturers worldwide. Experienced people back up our sales with complete service, spare parts, technical assistance, training and follow-up. KNOTEX WARP TYING AAACHINE has speeds up to 600 knots per minute. HACOBA WARPERS/BEAMERS guarantee high quality warps. Yam & Fabrics Machinery Home Office: BARCO INDUSTRIES, SYCOTEX: A complete integrated BOX 3978 • GREENVILLE, S.C. 29608 U.S.A. production management system for the textile industry. TEL. (803) 242-5262 - FAX (803) 271-4535 ' TELEX 216918 Table off Contents Clemson vs. -
COLLEGE ATHLETICS, COERCION, and the ESTABLISHMENT CLAUSE: the CASE of CLEMSON FOOTBALL Erin B. Edwards*
COPYRIGHT © 2020 VIRGINIA LAW REVIEW ASSOCIATION NOTE COLLEGE ATHLETICS, COERCION, AND THE ESTABLISHMENT CLAUSE: THE CASE OF CLEMSON FOOTBALL Erin B. Edwards* Once a person turns eighteen and goes to college, do they immediately become less susceptible to the influences of those in power and their peers? The Supreme Court tells us that they do. While consistently willing to find that prayers at middle school graduations and high school football games are violations of the Establishment Clause under the coercion test, the Court has stated that adults are more mature and “presumably” less susceptible to religious coercion. Scholars and the circuit courts of appeals have taken varying approaches and arrived at different outcomes when considering adult claimants. None, however, have articulated a uniform test for adults to establish coercion. Using indicative language from the Supreme Court, this Note argues for the first time that adult claimants must show that a State action has a “real and substantial likelihood” of coercion in order to bring a successful Establishment Clause challenge. It further proposes that a spectrum of susceptibility to coercion exists under the Establishment Clause based on certain populations’ ages and respective environments. After articulating the standard of coercion for adults and the spectrum of susceptibility to coercion, this Note applies both to a prominent example of overt incorporation of religion into a public university—the Clemson University football program. The Clemson football coaching staff unabashedly integrates religion into many aspects of the program, from Bible studies led and organized by staff to baptisms of players on the practice field. Using psychological and educational research about * J.D., University of Virginia School of Law, 2021; M.Ed., Clemson University, 2015.