Minimally Invasive Management of Ureteral Strictures: a 5-Year
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Jebmh.Com Original Research Article
Jebmh.com Original Research Article URETERIC STRICTURES AN ANALYTICAL STUDY OF AETIOLOGY, PATHOLOGY AND MANAGEMENT Saju P. R1, Rema Priyadarsini2, Vaibhav Vikas3, Praveen Gopi4, Rustum Singh Kaurav5 1Additional Professor, Department of Urology, Trivandrum Medical College, Trivandrum. 2Additional Professor, Department of Pathology, Alappuzha Medical College, Kerala. 3Senior Resident, Department of Urology, Trivandrum Medical College, Trivandrum. 4Senior Resident, Department of Urology, Trivandrum Medical College, Trivandrum. 5Senior Resident, Department of Urology, Trivandrum Medical College, Trivandrum. ABSTRACT BACKGROUND Ureteric strictures are common diseases of India due to tuberculosis, instrumentation, congenital and other reasons. In this study we found that tuberculosis (27%) and instrumentation (27%) were the leading causes of ureteric stricture. MATERIALS AND METHODS This is a prospective study conducted in the Department of Urology, Government Medical College, Thiruvananthapuram. Cases diagnosed as ureteric strictures by IVP and CT scan were taken up for this study. Their clinical features, investigations, treatment and surgical options were studied. RESULTS The total number of cases studied were 11 (5 males and 6 females). We found that three patients had tuberculous strictures and two patients had lower ureteric strictures with obstructive megaureter like presentation. Three cases had upper ureteric strictures with unknown aetiology. Three cases had iatrogenic ureteric strictures secondary to instrumentation. CONCLUSION We concluded from our study that Tuberculosis is a common cause of ureteric stricture. Prior history of instrumentation is the second most common cause of ureteric stricture. Lower ureteric stricture with obstructive megaureter like presentation was also not uncommon and an equally significant group of ureteric strictures had unknown aetiology. KEYWORDS Ureteric Stricture, Tuberculosis, Iatrogenic Stricture, Obstructive Megaureter, Instrumentation. -

Ureter an Innocent Bystander: Lower Ureteral Stricture Following
Arch Nephrol Urol 2019; 2 (2): 029-032 DOI: 10.26502/anu.2644-2833007 Case Report Ureter an Innocent Bystander: Lower Ureteral Stricture Following Angioembolisation of Uterine Artery Tushar Aditya Narain1, Manjeet Kumar2*, Shrawan Singh1, Gopal Sharma1, Shantanu Tyagi1 1Department of Urology, Postgraduate Institute of Medical Education and Research, Chandigarh, India 2Indira Gandhi Medical College and Hospital (IGMC), Shimla, Himachal Pradesh, India *Corresponding Author: Dr. Manjeet Kumar, Department of Urology, Indira Gandhi Medical College and Hospital (IGMC), Shimla, Himachal Pradesh, India, E-mail: [email protected] Received: 24 May 2019; Accepted: 31 May 2019; Published: 10 June 2019 Abstract Lower ureteric strictures are a common cause for unilateral hydroureteronephrosis, commonly resulting from previous surgeries, weather endoscopic, laproscopic or open. Devascularisation of the ureter resulting in fibrosis forms the underlying pathophysiology of stricture formation. We report a case of ureteral stricture resulting from angioembolization done for a bleeding arteriovenous malformation (AVM) of the uterus. Keywords: Angioembolisation; Stricture; Ureter 1. Introduction The main cause for ureteral stricture are surgical trauma, impacted ureteral stones, extrinsic compression from a tumor and congenital narrowing. Ureteral stricture is the most frequent complication observed in pelvic surgery. Ureteral strictures are typically due to ischemia, resulting in fibrosis. Wolf and colleagues defined a stricture as ischemic, when it follows open surgery or radiation therapy, whereas a stricture is considered nonischemic if it is caused by spontaneous stone passage or a congenital abnormality [1]. We report a case of ureteral stricture which developed after angioembolisation of bilateral uterine artery done for a bleeding arterio-venous malformation of the uterine cavity. -

Onlay Repair Technique for the Management of Ureteral Strictures: a Comprehensive Review
Hindawi BioMed Research International Volume 2020, Article ID 6178286, 11 pages https://doi.org/10.1155/2020/6178286 Review Article Onlay Repair Technique for the Management of Ureteral Strictures: A Comprehensive Review Shengwei Xiong ,1,2,3 Jie Wang,1,2,3 Weijie Zhu,1,2,3 Kunlin Yang,1,2,3 Guangpu Ding,1,2,3 Xuesong Li ,1,2,3 and Daniel D. Eun 4 1Department of Urology, Peking University First Hospital, No. 8 Xishiku St, Xicheng District, Beijing 100034, China 2Institute of Urology, Peking University, No. 8 Xishiku St, Xicheng District, Beijing 100034, China 3National Urological Cancer Center, No. 8 Xishiku St, Xicheng District, Beijing 100034, China 4Department of Urology, Temple University School of Medicine, 255S 17th Street, 7th Floor Medical Tower, Philadelphia, PA 19103, USA Correspondence should be addressed to Xuesong Li; [email protected] and Daniel D. Eun; [email protected] Received 5 March 2020; Revised 29 June 2020; Accepted 6 July 2020; Published 28 July 2020 Academic Editor: Achim Langenbucher Copyright © 2020 Shengwei Xiong et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Ureteroplasty using onlay grafts or flaps emerged as an innovative procedure for the management of proximal and midureteral strictures. Autologous grafts or flaps used commonly in ureteroplasty include the oral mucosae, bladder mucosae, ileal mucosae, and appendiceal mucosae. Oral mucosa grafts, especially buccal mucosa grafts (BMGs), have gained wide acceptance as a graft choice for ureteroplasty. -

Biodegradable Stent with Mtor Inhibitor-Eluting Reduces Progression of Ureteral Stricture
International Journal of Molecular Sciences Article Biodegradable Stent with mTOR Inhibitor-Eluting Reduces Progression of Ureteral Stricture Dong-Ru Ho 1,2,3 , Shih-Horng Su 4, Pey-Jium Chang 2, Wei-Yu Lin 1, Yun-Ching Huang 1, Jian-Hui Lin 1, Kuo-Tsai Huang 1, Wai-Nga Chan 1 and Chih-Shou Chen 1,* 1 Division of Urology, Department of Surgery, Chang Gung Memorial Hospital, Chiayi 613016, Taiwan; [email protected] (D.-R.H.); [email protected] (W.-Y.L.); [email protected] (Y.-C.H.); [email protected] (J.-H.L.); [email protected] (K.-T.H.); [email protected] (W.-N.C.) 2 Department of Medicine, College of Medicine, Chang Gung University, Taoyuan 333323, Taiwan; [email protected] 3 Department of Nursing, Chang Gung University of Science and Technology, Chiayi 613016, Taiwan 4 DuNing Incorperated, Tustin, CA 92780, USA; [email protected] * Correspondence: [email protected]; Tel.: +886-975-353-211 Abstract: In this study, we investigated the effect of mTOR inhibitor (mTORi) drug-eluting biodegrad- able stent (DE stent), a putative restenosis-inhibiting device for coronary artery, on thermal-injury- related ureteral stricture in rabbits. In vitro evaluation confirmed the dose-dependent effect of mTORi, i.e., rapamycin, on fibrotic markers in ureteral component cell lines. Upper ureteral fibro- sis was induced by ureteral thermal injury in open surgery, which was followed by insertion of biodegradable stents, with or without rapamycin drug-eluting. Immunohistochemistry and Western blotting were performed 4 weeks after the operation to determine gross anatomy changes, collagen deposition, expression of epithelial–mesenchymal transition markers, including Smad, α-SMA, and Citation: Ho, D.-R.; Su, S.-H.; Chang, SNAI 1. -

Clinical Study of Unilateral Or Bilateral Noncalculus Hydronephrosis and Or Hydroureter
International Journal of Recent Trends in Science And Technology, ISSN 2277-2812 E-ISSN 2249-8109, Volume 10, Issue 3, 2014 pp 438-446 Clinical Study of Unilateral or Bilateral Noncalculus Hydronephrosis and or Hydroureter 1 2 3* Kasabe P. , R. D. Jaykar , Rahul Wagh {1Assistant Professor,2 Associate Professor, 3 Resident} Department of General Surgery, Dr. V. M. Govt. Medical College, Solapur, Maharashtra, INDIA. *Corresponding Address: [email protected] Research Article Abstract: Background: Hydronephrosis is the dilation of the renal to the interruption of flow of urine, it is often due to an pelvis or calyces. Although patients usually presents with some obstructive process. Hydronephrosis is a very common signs and symptoms it can be clinically silent and is diagnosed as condition and it causes significant pain due to obstruction. an incidental finding during evaluation of an unrelated cause. Although calculus is the commonest cause of hydronephosis and Hydronephrosis can result from anatomic or functional hydroureter there are multiple noncalculus aetiology for the same process obstructing the flow of urine which can occur depending on the age and sex of the patient. This study is aimed anywhere from kidneys to the urethral meatus. Symptoms towards meticulous implementation of the accurate diagnostic tools depend on cause, location and duration of the obstruction. for early evaluation of noncalculus hydronephrosis and or Although patients usually presents with some signs and hydroureter and to assess the effectiveness of the early treatment symptoms it can be clinically silent and is diagnosed as towards the renal function sparing. Methods: In this prospective clinical study of 50 patients of hydronephrosis and or hydroureter an incidental finding during evaluation of an unrelated of all age groups and both the genders admitted in the department cause. -

Cystoscopy Insertion / Removal of Ureteric Stent
Tennyson Centre Darwin Private Hospital Suite 19 Suite 5 520 South Road Rocklands Drive Kurralta Park SA 5037 Tiwi NT 0810 P 08 8292 2399 P 08 8920 6212 F 08 8292 2388 F 08 8920 6213 [email protected] [email protected] www.urologicalsolutions.com.au www.urologicalsolutions.com.au CYSTOSCOPY INSERTION / REMOVAL OF URETERIC STENT Providing Specialist Care in South Australia & Northern Territory Associates: Dr Kym Horsell Dr Kim Pese Dr Michael Chong Dr Jason Lee Dr Alex Jay Dr Henry Duncan What is a Ureteric Stent? A ureteric stent is a specially designed hollow tube, made of a flexible plastic material that is placed in the ureter. The length of the stents used in adult patients varies between 22-30cm. 22-30cm long It is designed to stay in the urinary system by having both ends coiled; the top end coils in the kidney and the lower end coils inside the bladder to prevent its displacement. Stents are flexible enough to withstand various body movements. Stents are temporarily placed in the kidney to prevent or relieve obstruction. They allow urine to pass down the ureter, can help to relieve pain (e.g. from a stone/stone fragments), drain infection or help with kidney function if the kidney is obstructed. Having a stent in place will allow the ureter to heal. In the majority of patients, stents are required for only a short duration. This may be just a few days. However, a stent can stay in for up to three months without the need to replace it. -

EAU Guidelines on Urinary Incontinence 2016
EAU Guidelines on Urinary Incontinence in Adults F.C . Burkhard (Chair), M.G. Lucas, L.C. Berghmans, J.L.H.R. Bosch, F. Cruz, G.E. Lemack, A.K. Nambiar, C.G. Nilsson, R. Pickard, A. Tubaro Guidelines Associates: D. Bedretdinova, F. Farag, B.B. Rozenberg © European Association of Urology 2016 TABLE OF CONTENTS PAGE 1. INTRODUCTION 6 1.1 Aim and objectives 6 1.2 Panel composition 6 1.3 Available publications 6 1.4 Publication history 6 2. METHODS 7 2.1 Introduction 7 2.2 Review 7 2.3 Terminology 7 3. DIAGNOSTIC EVALUATION 8 3.1 History and physical examination 8 3.2 Patient questionnaires 8 3.2.1 Questions 8 3.2.2 Evidence 8 3.3 Voiding diaries 9 3.3.1 Questions 10 3.3.2 Evidence 10 3.4 Urinalysis and urinary tract infection 10 3.4.1 Questions 10 3.4.2 Evidence 10 3.5 Post-voiding residual volume 11 3.5.1 Question 11 3.5.2 Evidence 11 3.6 Urodynamics 11 3.6.1 Question 11 3.6.2 Evidence 11 3.6.2.1 Variability 11 3.6.2.2 Diagnostic accuracy 12 3.6.2.3 Does urodynamics influence the outcome of conservative therapy 12 3.6.2.4 Does urodynamics influence the outcome of surgery for urinary incontinence? 12 3.6.2.5 Does urodynamics help to predict complications of surgery for UI? 12 3.6.2.6 Does urodynamics influence the outcome of treatment for post- prostatectomy urinary incontinence in men? 13 3.6.3 Research priority 13 3.7 Pad testing 13 3.7.1 Question 13 3.7.2 Evidence 13 3.7.3 Research priority 14 3.8 Imaging 14 3.8.1 Questions 14 3.8.2 Evidence 14 3.8.3 Research priority 15 4. -

EAU Guidelines on Urinary Incontinence in Adults
EAU Guidelines on Urinary Incontinence in Adults F.C . Burkhard (Chair), J.L.H.R. Bosch, F. Cruz, G.E. Lemack, A.K. Nambiar, N. Thiruchelvam, A. Tubaro Guidelines Associates: D. Ambühl, D.A. Bedretdinova, F. Farag, R. Lombardo, M.P. Schneider © European Association of Urology 2018 TABLE OF CONTENTS PAGE 1. INTRODUCTION 8 1.1 Aim and objectives 8 1.1.1 The elderly 8 1.2 Panel composition 8 1.3 Available publications 8 1.4 Publication history 9 1.4.1 Summary of changes. 9 2. METHODS 11 2.1 Introduction 11 2.2 Review 11 2.3 Future goals 11 3. DIAGNOSTIC EVALUATION 11 3.1 History and physical examination 11 3.2 Patient questionnaires 12 3.2.1 Questions 12 3.2.2 Evidence 12 3.2.3 Summary of evidence and recommendations for patient questionnaires 13 3.3 Voiding diaries 14 3.3.1 Question 14 3.3.2 Evidence 14 3.3.3 Summary of evidence and recommendations for voiding diaries 14 3.4 Urinalysis and urinary tract infection 14 3.4.1 Question 14 3.4.2 Evidence 14 3.4.3 Summary of evidence and recommendations for urinalysis 15 3.5 Post-void residual volume 15 3.5.1 Question 15 3.5.2 Evidence 15 3.5.3 Summary of evidence and recommendations for post-void residual 15 3.6 Urodynamics 15 3.6.1 Question 16 3.6.2 Evidence 16 3.6.2.1 Variability 16 3.6.2.2 Diagnostic accuracy 16 3.6.2.3 Question 16 3.6.2.4 Evidence 16 3.6.2.5 Question 16 3.6.2.6 Evidence 16 3.6.2.7 Question 17 3.6.2.8 Evidence 17 3.6.2.9 Question 17 3.6.2.10 Evidence 17 3.6.3 Summary of evidence and recommendations for urodynamics 17 3.6.4 Research priority 18 3.7 Pad testing 18 3.7.1 Questions 18 3.7.2 Evidence 18 3.7.3 Summary of evidence and recommendations for pad testing 18 3.7.4 Research priority 18 3.8 Imaging 18 3.8.1 Questions 19 3.8.2 Evidence 19 3.8.3 Summary of evidence and recommendations for imaging 19 3.8.4 Research priority 19 2 URINARY INCONTINENCE IN ADULTS - LIMITED UPDATE MARCH 2018 4. -

Laparoscopic and Robotic Management of Ureteral Stricture In
in vivo 34 : 965-972 (2020) doi:10.21873/invivo.11864 Review Laparoscopic and Robotic Management of Ureteral Stricture in Adults FILIPPOS KAPOGIANNIS 1,2 , ELEFTHERIOS SPARTALIS 2,3 , KONSTANTINOS FASOULAKIS 1, GERASIMOS TSOUROUFLIS 2,3 , DIMITRIOS DIMITROULIS 2,3 and NIKOLAOS I. NIKITEAS 2,3 1Department of Urology, Hippokrateion Hospital, Athens, Greece; 2Hellenic Minimally Invasive and Robotic Surgery (MIRS) Study Group, Athens Medical School, National and Kapodistrian University of Athens, Athens, Greece; 3Second Department of Propaedeutic Surgery, Laiko Hospital, Athens Medical School, National and Kapodistrian University of Athens, Athens, Greece Abstract. Background/Aim: The aim of this review was to flow of urine. When this occurs, urine backs up into the provide an update on the status of minimal invasive treatment kidney and may cause pain, urinary tract infections, or of ureteral stricture either with a laparoscopic or robotic kidney failure. Management of strictures not amenable to surgery. Materials and Methods: Eligible studies, published endoscopic treatment involves ureteral reconstruction, which until November 2019 were retrieved through Medline, still remains a challenging therapy option. During the past Cochrane and Pubmed databases. Predetermined inclusion three decades, the field of minimally invasive surgery, and exclusion criteria were used as selection method for data especially in urology, has brought major changes in synthesis and acquisition. The study was performed in treatment strategies, firstly with laparoscopy, and more accordance with the PRISMA statement. Results: A total of 19 recently with robotic surgery. The aim of our study was to retrospective studies met the inclusion criteria. All of them provide an outline of the increased adoption of these demonstrated the safety, feasibility and success of both advancements which although not mature seem to provide laparoscopic and robotic ureteral reconstruction. -

Tubercular Stricture at Lower End of Ureter Causing Vesicoureteric Junction Obstruction: Our Experience in Rangpur Medical College A.H.M
............ TUBERCULAR STRICTURE AT LOWER END OF URETER CAUSING VESICOURETERIC JUNCTION OBSTRUCTION: OUR EXPERIENCE IN RANGPUR MEDICAL COLLEGE A.H.M. MANJURUL ISLAM1, M ZAHID HASSAIN2, MD ANOWAR HOSSAIN1, MD SHAHIDUL ISLAM1, TAPAS BOSE3 1Department of U3rology, Rangpur Medical College and Hospital, 2Department of Urology, United Hospital, 3Department of Respiratory Medicine, Rangpur Medical College and Hospital, Rangpur, Bangladesh. Abstract Objective: To determine the outcome of ureteroneocystostomy for vesicoureteric junction obstruction due to tubercular stricture. Patients and Method: Twelve patients age from 19 years to 47 years were underwant uretroneocystostomy with ifilateral D-J stanting for vecicoureteric junction obstruction (VUJO) with proximal hydroureteronephrosis tissue from the lower of the ureter shows granunation lesion complatable with tuberculosis. D-J stant were remove and patients were put into antitubercular chemotherapy . Results: Patients were symptom free and follow up IVU at six months interval shows free passage of contrast at 10 minutes film. Conclusion: Vesicoureteric junction obstruction (VUJO) due to lower ureteric stricture by tuberculus lesion, though rare, should be searched, because if not treated properly may lead to damage of ipsilateral renal unit. Bangladesh J. Urol. 2016; 19(1): 13-17 Introduction to cure disease and prevent the development of drug Ureteric stricture following TB is rare. The commonest resistant all led to modern-day control efforts[2]. Since site of tubercular stricture formation is close to 1994, the DOTS and Stop TB strategies have been ureterovesical junction[1]. Stricture formation is also successfully implemented in more than 180 of the 212 seen at the level of of ureteropelvic junction and less World Health Organization (WHO) member states. -
Stent Insertion Under General Anasthesia Patient Identifier/Label Statement of Patient
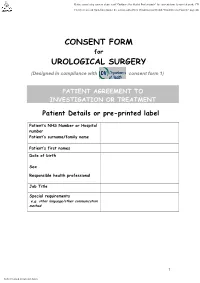
CONSENT FORM for UROLOGICAL SURGERY (Designed in compliance with consent form 1) PATIENT AGREEMENT TO INVESTIGATION OR TREATMENT Patient Details or pre-printed label Patient’s NHS Number or Hospital number Patient’s surname/family name Patient’s first names Date of birth Sex Responsible health professional Job Title Special requirements e.g. other language/other communication method 1 Patient identifier/label Name of proposed procedure ANAESTHETIC (Include brief explanation if medical term not clear) (Rigid ) CYSTOSCOPY AND STENT PROCEDURE SIDE……….. - GENERAL/REGIONAL THIS PROCEDURE INVOLVES TELESCOPIC INSPECTION OF BLADDER AND URETHRA AND - LOCAL INSERTING, REMOVING OR CHANGING A SOFT PLASTIC TUBE PLACED BETWEEN THE KIDNEY AND - SEDATION THE BLADDER. Statement of health professional (To be filled in by health professional with appropriate knowledge of proposed procedure, as specified in consent policy) I have explained the procedure to the patient. In particular, I have explained: The intended benefits TO DIAGNOSE AND TREAT ABNORMALITY OF THE URETERIC TUBE Serious or frequently occurring risks including any extra procedures, which may become necessary during the procedure. I have also discussed what the procedure is likely to involve, the benefits and risks of any available alternative treatments (including no treatment) and any particular concerns of this patient. Please tick the box once explained to patient COMMON MILD BURNING OR BLEEDING ON PASSING URINE FOR SHORT PERIOD AFTER OPERATION TEMPORARY INSERTION OF A CATHETER TEMPORARY -

Cystoscopy & Retrograde Pyelogram (&/-) Insertion Ureteric Stent
(Affix identification label here) 2018 URN: Cystoscopy & Retrograde Family name: Pyelogram +/- Insertion of Given name(s): Ureteric Stent Address: Date of birth: Sex: M F I Facility: A. Interpreter / cultural needs • Rarely damage to the urethra. A false passage may be produced causing leakage of urine or in the long term, a An Interpreter Service is required? Yes No narrowing that may affect flow of urine. If Yes, is a qualified Interpreter present? Yes No • Damage to the bladder by puncturing the bladder wall. This may need further surgery. A Cultural Support Person is required? Yes No © The State of Queensland (Queensland Health), Health), (Queensland Queensland of State The © • Swelling at the exit of the bladder which may stop If Yes, is a Cultural Support Person present? Yes No passage of urine. A tube (catheter) may need to be inserted to drain the urine until the swelling goes down. B. Condition and treatment • Bacteria may get into the blood stream with the The doctor has explained that you have the following development of septicaemia. Further treatment with condition: (Doctor to document in patient’s own words) antibiotics may be necessary. Permission to reproduce should be sought from [email protected] from sought be should reproduce to Permission • The tube may pass outside the ureter into the tissues. .......................................................................................................................................................................... This may need further surgery to remove and replace This condition requires the following procedure. (Doctor to the tube. document - include site and/or side where relevant to the • Bleeding which may stain the urine colour and procedure) sometimes cause blockage of urine flow.