Effect of Mirabegron on Cognitive Function in Elderly
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Long Term Follow up of Mirabegron - a Real Life- Pragmatic Experience
Central Journal of Urology and Research Bringing Excellence in Open Access Research Article *Corresponding author Haitham Abdelmoteleb, Bristol Urological Institute, Southmead Hospital, Bristol, BS10 5NB, UK, Tel: 440-7884- Long Term Follow Up of 827995; Email: Submitted: 04 June 2016 Mirabegron - A Real Life- Accepted: 22 August 2016 Published: 24 August 2016 ISSN: 2379-951X Pragmatic Experience Copyright Haitham Abdelmoteleb*, Musaab Yassin, and Hashim Hashim © 2016 Abdelmoteleb et al. Bristol Urological Institute, South mead Hospital, UK OPEN ACCESS Abstract Keywords • Mirabegron Objectives: To evaluate the efficacy and tolerability of Mirabegron for the • Beta-3 agonist treatment of overactive bladder symptoms in a real life, long term follow up study • Overactive bladder syndrome conducted in a tertiary referral centre. • Long term Methods: A structured telephone questionnaire of patients was conducted in order to evaluate the efficacy and tolerability of Mirabegron. Patients who were initially prescribed and responded to Mirabegron 50mg once daily between 6/2013 and 9/2013, were interviewed to see if they were compliant with treatment, continue to respond to treatment and if they discontinued treatment. Results: Follow-up was for a mean of 11.7 months. At short-term follow-up, 20/39 patients responded to treatment. In the long term follow-up, 18/20 patients were still using Mirabegron. 2/20 patients discontinued because of lack of efficacy. Overall, the main reasons for discontinuation of Mirabegron after trying it for a mean of 5.3 months, was lack of efficacy and adverse events. The majority of AEs were mild in severity and few were serious. Other reasons include the lack of further prescription from general practitioners. -

Betmiga, INN-Mirabegron
EMA/591015/2015 EMEA/H/C/002388 EPAR summary for the public Betmiga mirabegron This is a summary of the European public assessment report (EPAR) for Betmiga. It explains how the Committee for Medicinal Products for Human Use (CHMP) assessed the medicine to reach its opinion in favour of granting a marketing authorisation and its recommendations on the conditions of use for Betmiga. What is Betmiga? Betmiga is a medicine containing the active substance mirabegron. It is available as prolonged-release tablets (25 mg, 50 mg). ‘Prolonged-release’ means that mirabegron is released slowly from the tablet over a few hours. What is Betmiga used for? Betmiga is used in adults with overactive bladder syndrome. It is used to treat certain symptoms of the condition: urgency (sudden urge to urinate), increased urinary frequency (the need to urinate frequently) and urge incontinence (involuntary leakage of urine from the bladder when a sudden strong need to urinate is felt). The medicine can only be obtained with a prescription. How is Betmiga used? The recommended dose of Betmiga is 50 mg once a day. In patients who have reduced kidney or liver function the doctor may need to prescribe a lower dose or avoid the use of Betmiga, especially in patients taking certain other medicines. For full details, see the package leaflet (also part of the EPAR). 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2015. -

Frailty & Cognihon: Management of OAB in Elderly & Frail Pahents
Frailty & Cogni.on: Management of OAB in Elderly & Frail Pa.ents MR. RAHUL MISTRY CONSULTANT UROLOGICAL SURGEON POGP CONFERENCE NOVEMBER 2016 Topics • What are LUTS? • Symptom definiDons • The impact of OAB on paents • Management of OAB • The challenge of treang OAB • The Ancholinergic burden • Novel treatment of OAB Change of Terminology • LUTS = Lower urinary tract symptoms • LUTS instead of “prostasm” • Storage instead of “irritave” • Voiding instead of “obstrucDve” What are LUTS Post-micturion Storage symptoms Voiding symptoms symptoms DayDme frequency Slow stream Post-micturiDon Nocturia Spraying dribbling Incomplete Urgency IntermiUency emptying Urinary Hesitancy inconnence Straining Terminal dribbling Definions • Urgency - sudden compelling desire to pass urine which is difficult to defer • Urinary inconnence • any involuntary leakage of urine (urge / stress) • may need to be disDnguished from sweang or vaginal discharge • Increased dayme frequency - the complaint by the paent who considers that he/she voids too o]en by day • Nocturia - individual has to wake at night one or more Dmes to void • ICS DefiniDons, Abrams P et al. Neurourol Urodyn; 21:167-178 (2002) Defini.on of Overac.ve Bladder (OAB) (Internaonal Connence Society) 1. Abrams P et al. Neurourol Urodyn 2002;21:167-178 Mrs W. E. Terrible, your classic pa.ent? Age: 64 year old woman Occupaon: Recently reDred from an office job Symptoms: • Urinary frequency (14−15 Dmes a day) • Urge inconDnence (daily) • Nocturia (3 Dmes a night) THe impact of OAB on pa.ents How do OAB symptoms affect pa.ents? haven’t slept depressing like a baby negave lose control locked in embarrassing exhausted no control terrible so red I keep it xxx secret Quotes from a video of real-life OAB paents talking about how OAB has affected their lives. -
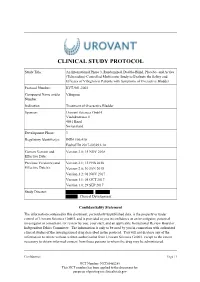
Study Protocol
CLINICAL STUDY PROTOCOL Study Title: An International Phase 3, Randomized, Double-Blind, Placebo- and Active (Tolterodine)-Controlled Multicenter Study to Evaluate the Safety and Efficacy of Vibegron in Patients with Symptoms of Overactive Bladder Protocol Number: RVT-901-3003 Compound Name and/or Vibegron Number: Indication Treatment of Overactive Bladder Sponsor: Urovant Sciences GmbH Viaduktstrasse 8 4051 Basel Switzerland Development Phase: 3 Regulatory Identifier(s): IND# 106,410 EudraCT# 2017-003293-14 Current Version and Version 3.0; 15 NOV 2018 Effective Date: Previous Version(s) and Version 2.1; 12 FEB 2018 Effective Date(s): Version 2.0; 30 JAN 2018 Version 1.2; 01 NOV 2017 Version 1.1; 05 OCT 2017 Version 1.0; 29 SEP 2017 Study Director: , , Clinical Development Confidentiality Statement The information contained in this document, particularly unpublished data, is the property or under control of Urovant Sciences GmbH, and is provided to you in confidence as an investigator, potential investigator or consultant, for review by you, your staff, and an applicable Institutional Review Board or Independent Ethics Committee. The information is only to be used by you in connection with authorized clinical studies of the investigational drug described in the protocol. You will not disclose any of the information to others without written authorization from Urovant Sciences GmbH. except to the extent necessary to obtain informed consent from those persons to whom the drug may be administered. Confidential Page | 1 NCT Number: NCT03492281 This NCT number has been applied to the document for purposes of posting on clinicaltrials.gov Clinical Study Protocol RVT-901-3003 Urovant Sciences GmbH Effective: 15 NOV 2018 SUMMARY OF CHANGES Version Location Description of Change 3.0 Global Minor typographical/formatting errors were corrected. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Understanding Drug-Drug Interactions Due to Mechanism-Based Inhibition in Clinical Practice
pharmaceutics Review Mechanisms of CYP450 Inhibition: Understanding Drug-Drug Interactions Due to Mechanism-Based Inhibition in Clinical Practice Malavika Deodhar 1, Sweilem B Al Rihani 1 , Meghan J. Arwood 1, Lucy Darakjian 1, Pamela Dow 1 , Jacques Turgeon 1,2 and Veronique Michaud 1,2,* 1 Tabula Rasa HealthCare Precision Pharmacotherapy Research and Development Institute, Orlando, FL 32827, USA; [email protected] (M.D.); [email protected] (S.B.A.R.); [email protected] (M.J.A.); [email protected] (L.D.); [email protected] (P.D.); [email protected] (J.T.) 2 Faculty of Pharmacy, Université de Montréal, Montreal, QC H3C 3J7, Canada * Correspondence: [email protected]; Tel.: +1-856-938-8697 Received: 5 August 2020; Accepted: 31 August 2020; Published: 4 September 2020 Abstract: In an ageing society, polypharmacy has become a major public health and economic issue. Overuse of medications, especially in patients with chronic diseases, carries major health risks. One common consequence of polypharmacy is the increased emergence of adverse drug events, mainly from drug–drug interactions. The majority of currently available drugs are metabolized by CYP450 enzymes. Interactions due to shared CYP450-mediated metabolic pathways for two or more drugs are frequent, especially through reversible or irreversible CYP450 inhibition. The magnitude of these interactions depends on several factors, including varying affinity and concentration of substrates, time delay between the administration of the drugs, and mechanisms of CYP450 inhibition. Various types of CYP450 inhibition (competitive, non-competitive, mechanism-based) have been observed clinically, and interactions of these types require a distinct clinical management strategy. This review focuses on mechanism-based inhibition, which occurs when a substrate forms a reactive intermediate, creating a stable enzyme–intermediate complex that irreversibly reduces enzyme activity. -

170 Limited Use of Anticholinergic Drugs For
170 Penning-van Beest F1, Sukel M1, Reilly K2, Kopp Z2, Erkens J1, Herings R1 1. PHARMO Institute, 2. Pfizer Inc LIMITED USE OF ANTICHOLINERGIC DRUGS FOR OVERACTIVE BLADDER: A PHARMO STUDY Hypothesis / aims of study The aim of the study was to determine the prevalence of use of anticholinergic drugs for overactive bladder (OAB) in men and women in the Netherlands in the period 1998-2003. Study design, materials and methods Data were obtained from the PHARMO Record Linkage System, which includes patient centric data of drug-dispensing records and hospital records of more than one million patients in the Netherlands. Currently four anticholinergic drugs are available on the Dutch market for the treatment of OAB: tolterodine immediate release (IR), since 1998, tolterodine extended release (ER), since 2001, oxybutynin, since 1986, and flavoxate, since 1979. All patients who were ever prescribed these OAB drugs in the period January 1998 until December 2003 were included in the study cohort. The prevalence of use of tolterodine ER, tolterodine IR, oxybutynin and flavoxate was determined per calendar year, stratified by gender, by counting the number of patients having a dispensing with a duration of use including a single fixed day a year. Results The number of OAB drug users included in the study cohort increased from about 3,800 in 1998 to 5,000 in 2003. About 60% of the OAB drug users in the study cohort were women and about 42% of the OAB drug users were 70 years or older. The use of OAB drugs increased from 100 users per 100,000 men in 1998 to 140 users per 100,000 men in 2003 (table). -

The Pharmacology of Paediatric Incontinence
BJU International (2000), 86, 581±589 The pharmacology of paediatric incontinence P.B. HOEBEKE* and J. VANDE WALLE² *Departments of Paediatric Urology and ²Paediatric Nephrology, Ghant University Hospital, Belgium Introduction ' the accommodation of increasing volumes of urine The clinical uropharmacology of the lower urinary tract at a low intravesical pressure and with appropriate is based on an appreciation of the innervation and sensation receptor content of the bladder and its related anatomical ' a bladder outlet that is closed and remains so during structures. The anatomy, neuroanatomy and neuro- increases in intra-abdominal pressures physiology of the bladder is reviewed. Classes of drugs are ' and absence of involuntary bladder contractions [2]. discussed in relation to the possible functional targets of pharmacological intervention and ®nally some speci®c In children the development of continence and applications in paediatric voiding dysfunction are voluntary voiding involves maturation of the nervous discussed. system and behavioural learning. Toilet training mainly depends on the cognitive perception of the maturing urinary tract. This implies a high sensibility for the Pharmacological interactions development of dysfunctions [3]. The storage and A short review of anatomy, neuroanatomy and neuro- evacuation of urine are controlled by two functional physiology is essential to understand pharmacological units in the lower urinary tract, i.e. the reservoir (the interactions. These interactions with effects on bladder bladder) and an outlet (consisting of the bladder neck, function can occur on different levels, i.e. on bladder urethra and striated muscles of the pelvic ¯oor). In the mucosa, bladder smooth muscle or bladder outlet striated bladder, two regions (Fig. -

Anticholinergics for Overactive Bladder Evidence, Clinical Issues and Comparisons
Anticholinergics for Overactive Bladder Evidence, Clinical Issues and Comparisons RxFiles Academic Detailing Program March 2008 Saskatoon City Hospital 701 Queen Street, Saskatoon, SK S7K 0M7 www.RxFiles.ca Recent Guidelines: Overactive Bladder – Background • Special caution should be used for the elderly who Canadian Urological1: • Overactive bladder (OAB) is also known as urge are especially sensitive to side effects from ACs. Can J Urol. 2006;13(3):3127-38 incontinence and occurs when there is an inability Some with dementia or cognitive impairment may 2 not tolerate ACs at all. If using an AC in the NICE (UK) 2006 : to delay voiding when an urge is perceived. elderly, start at the lowest dose, titrate up and www.nice.org.uk/nicemedia/pdf/CG • OAB is differentiated from stress urinary 40fullguideline.pdf reassess for effectiveness and adverse effects. incontinence (SUI) which is associated with a loss of Remember that many drugs contribute to the total urine secondary to intra-abdominal pressure such as anticholinergic load (e.g. antidepressants, antipsychotics).14 Systematic Reviews: occurs with coughing, sneezing and exercise.9 Cochrane: Hay-Smith J et al. • ACs should not be used with acetylcholinesterase • Anticholinergics (ACs) are useful drugs for Which anticholinergics drug for inhibitors (e.g. ARICEPT, REMINYL, EXELON) given treating OAB, however their use is limited by the overactive bladder symptoms in their opposing mechanisms.23 adults. Cochrane Systematic side effects of dry mouth and constipation. 3 Reviews 2005, Issue 3. 4 Oregon 2005 : Are non-drug treatment options effective? Oxybutynin (Oxy) vs Tolterodine (Tol) • A Cochrane systematic review found 3: www.ohsu.edu/drugeffectiveness/rep • Bladder training (a gradual time lengthening orts/documents/OAB%20Final%20 no statistically significant differences for Report%20Update%203.pdf between voids) or urge suppression may be useful 10 patient perceived improvement, leakage Canada in OAB, especially in addition to ACs. -

Oxybutynin: Dry Days for Patients with Hyperhidrosis
r E v i E w oxybutynin: dry days for patients with hyperhidrosis G.S. Mijnhout1*, H. Kloosterman2, S. Simsek1, R.J.M. Strack van Schijndel3, J.C. Netelenbos1 Departments of 1Endocrinology and 3Internal Medicine, VU University Medical Centre, Amsterdam, the Netherlands, 2General Practitioner, Den Helder, the Netherlands, *corresponding author: tel.: +31 (0)20-444 41 01, fax: +31 (0)20-444 05 02, e-mail: [email protected] A b s T r act we report the case of a 56-year-old postmenopausal woman Table 1. Causes of hyperhidrosis who was referred to our Endocrinology outpatient Clinic generalised because of severe hyperhidrosis. she had a four-year history Menopausal of excessive sweating of her face and upper body. on Endocrine diseases: hyperthyroidism, carcinoid syndrome, presentation no sweating could be documented. physical pheochromocytoma, mastocytosis, diabetes mellitus, hypoglycaemia, acromegaly examination was also unremarkable. it appeared that Serotonin syndrome five days earlier her general practitioner had prescribed Chronic infections: e.g. endocarditis, tuberculosis, HIV oxybutynin for urge incontinence and this accidentally infection cured her hyperhidrosis. she was diagnosed with idiopathic Malignancy: lymphoma, bronchial carcinoma with compression of the sympathetic chain hyperhidrosis. we advised her to continue the oxybutynin Neurological: brain damage, spinal cord injuries, autonomic and six months later, she was still symptom-free. oral dysreflexia, Parkinson’s disease, Shapiro’s syndrome anticholinergic drugs are known to be effective for Drug-induced: antidepressants, antipyretics, antimigraine drugs, hyperhidrosis, but only anecdotal reports on oxybutynin cholinergic agonists, GnRH agonists, sympathomimetic agents, b-blockers, cyclosporine and many others can be found in the literature. -

Download SPC Oxybutynin 2.5Mg
SUMMARY OF PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT Oxybutynin hydrochloride 2.5 mg tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each 2.5 mg tablet contains 2.5mg Oxybutynin hydrochloride Excipient(s) with known effect: Contains 53.25 mg Lactose monohydrate per tablet. For the full list of excipient, see section 6.1. 3 PHARMACEUTICAL FORM Tablets White to off white, odourless, 5mm round biconvex, uncoated tablets with inscription “BS” on one side and plain on the other side. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Adults Treatment of frequency, urgency or urge incontinence as may occur in bladder overactivity whether due to neurogenic bladder disorders (detrusor hyperreflexia) or idiopathic detrusor overactivity. Paediatric population Oxybutynin hydrochloride is indicated for children over 5 years for: - Urinary incontinence, urgency and frequency in overactive bladder conditions caused by idiopathic overactive bladder or neurogenic bladder dysfunction (detrusor over activity). - Nocturnal enuresis associated with detrusor over activity, in conjunction with non-drug therapy, when other treatment not been successful. 4.2 Posology and method of administration Dosage and administration: Adults: The dosage should be determined individually, with an initial dose of 2.5 mg three times daily. Thereafter, the lowest effective dose should be selected. The daily dose may vary between 10 and 15 mg per day (maximum dose is 20 mg per day) divided into 2-3 (max. 4) doses. Elderly: The elimination half-life is increased in the elderly. Therefore, a dose of 2.5mg twice a day, particularly if the patient is frail, is likely to be adequate. This dose may be titrated upwards to 5mg two times a day to obtain a clinical response provided the side effects are well tolerated. -

[Product Monograph Template
PRODUCT MONOGRAPH Pr ® MYRBETRIQ mirabegron extended-release tablets 25 mg and 50 mg Selective beta 3-adrenoceptor agonist Astellas Pharma Canada, Inc. Date of Revision: Markham, ON L3R 0B8 June 02, 2016 Submission Control No: 192447 16A007-MIR-CAN MYRBETRIQ® is a registered trademark of Astellas Pharma Inc. MYRBETRIQ® Product Monograph Page 1 of 40 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE ..............................................................................3 CONTRAINDICATIONS ...................................................................................................3 WARNINGS AND PRECAUTIONS ..................................................................................4 ADVERSE REACTIONS ....................................................................................................7 DRUG INTERACTIONS ..................................................................................................11 DOSAGE AND ADMINISTRATION ..............................................................................17 OVERDOSAGE ................................................................................................................18 ACTION AND CLINICAL PHARMACOLOGY ............................................................18 STORAGE AND STABILITY ..........................................................................................22