Thesis-Steven Wilson
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Summary Benchmarks for Preferred Practice Pattern® Guidelines
SUMMARY BENCHMARKS FOR PREFERRED PRACTICE PATTERN® GUIDELINES TABLE OF CONTENTS Summary Benchmarks for Preferred Practice Pattern Guidelines Introduction . 1 Glaucoma Primary Open-Angle Glaucoma (Initial Evaluation) . 3 Primary Open-Angle Glaucoma (Follow-up Evaluation) . 5 Primary Open-Angle Glaucoma Suspect (Initial and Follow-up Evaluation) . 6 Primary Angle-Closure Disease (Initial Evaluation and Therapy) . 8 Retina Age-Related Macular Degeneration (Initial and Follow-up Evaluation) . 10 Age-Related Macular Degeneration (Management Recommendations) . 11 Diabetic Retinopathy (Initial and Follow-up Evaluation) . 12 Diabetic Retinopathy (Management Recommendations) . 13 Idiopathic Epiretinal Membrane and Vitreomacular Traction (Initial Evaluation and Therapy) . 14 Idiopathic Macular Hole (Initial Evaluation and Therapy) . 15 Posterior Vitreous Detachment, Retinal Breaks, and Lattice Degeneration (Initial and Follow-up Evaluation) . 17 Retinal and Ophthalmic Artery Occlusions (Initial Evaluation and Therapy) . 18 Retinal Vein Occlusions (Initial Evaluation and Therapy) . 19 Cataract/Anterior Segment Cataract (Initial and Follow-up Evaluation) . 20 Cornea/External Disease Bacterial Keratitis (Initial Evaluation) . 22 Bacterial Keratitis (Management Recommendations) . 23 Blepharitis (Initial and Follow-up Evaluation) . 24 Conjunctivitis (Initial Evaluation) . 25 Conjunctivitis (Management Recommendations) . 26 Corneal Ectasia (Initial Evaluation and Follow-up) . 27 Corneal Edema and Opacification (Initial Evaluation) . 28 Corneal Edema -

Description of Alternative Approaches to Measure and Place a Value on Hospital Products in Seven Oecd Countries
OECD Health Working Papers No. 56 Description of Alternative Approaches to Measure Luca Lorenzoni, and Place a Value Mark Pearson on Hospital Products in Seven OECD Countries https://dx.doi.org/10.1787/5kgdt91bpq24-en Unclassified DELSA/HEA/WD/HWP(2011)2 Organisation de Coopération et de Développement Économiques Organisation for Economic Co-operation and Development 14-Apr-2011 ___________________________________________________________________________________________ _____________ English text only DIRECTORATE FOR EMPLOYMENT, LABOUR AND SOCIAL AFFAIRS HEALTH COMMITTEE Unclassified DELSA/HEA/WD/HWP(2011)2 Health Working Papers OECD HEALTH WORKING PAPERS NO. 56 DESCRIPTION OF ALTERNATIVE APPROACHES TO MEASURE AND PLACE A VALUE ON HOSPITAL PRODUCTS IN SEVEN OECD COUNTRIES Luca Lorenzoni and Mark Pearson JEL Classification: H51, I12, and I19 English text only JT03300281 Document complet disponible sur OLIS dans son format d'origine Complete document available on OLIS in its original format DELSA/HEA/WD/HWP(2011)2 DIRECTORATE FOR EMPLOYMENT, LABOUR AND SOCIAL AFFAIRS www.oecd.org/els OECD HEALTH WORKING PAPERS http://www.oecd.org/els/health/workingpapers This series is designed to make available to a wider readership health studies prepared for use within the OECD. Authorship is usually collective, but principal writers are named. The papers are generally available only in their original language – English or French – with a summary in the other. Comment on the series is welcome, and should be sent to the Directorate for Employment, Labour and Social Affairs, 2, rue André-Pascal, 75775 PARIS CEDEX 16, France. The opinions expressed and arguments employed here are the responsibility of the author(s) and do not necessarily reflect those of the OECD. -
National Correct Coding Initiative's (Ncci) General
NATIONAL CORRECT CODING INITIATIVE’S (NCCI) GENERAL CORRESPONDENCE LANGUAGE AND SECTION-SPECIFIC EXAMPLES (FOR NCCI PROCEDURE TO PROCEDURE (PTP) EDITS AND MEDICALLY UNLIKELY EDITS (MUE)) EFFECTIVE: April 1, 2017* *INCLUDES 2017 HCPCS/CPT CODES Current Procedural Terminology (CPT) codes, descriptions and other data only are copyright 2016 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein. TABLE OF CONTENTS Section Page Introduction 5 General Correspondence Language for NCCI PTP Edits and Medically Unlikely Edits (MUEs) Standard preparation/monitoring services for anesthesia 8 HCPCS/CPT procedure code definition 8 CPT Manual or CMS manual coding instruction 8 Mutually exclusive procedures 9 Sequential procedure 9 CPT “Separate procedure” definition 9 More extensive procedure 9 Gender-specific procedures 10 Standards of medical/surgical practice 10 Anesthesia service included in surgical procedure 10 Laboratory panel 10 Deleted/modified edits for NCCI 11 Misuse of column two code with column one code 11 Medically Unlikely Edits (MUE) (Units of Service) 11 Deleted/modified edits -

Retinal Pigment Epithelial Tear Resembling Retinal Tear
Correspondence 333 References 5University of Washington/Fred Hutchinson 1 Dean WH, Banda L, Kambewa ES, Sherwin JC. Increased Cancer Research Center, Seattle, WA, USA intraocular pressure on the first post-operative day 6Department of Ophthalmology and Visual following sutureless extracapsular cataract surgery in Sciences, The University of Texas Medical Branch, Africa. Eye 2012; 26: 332. Galveston, TX, USA 2 Kim JY, Jo MW, Brauner SC, Ferrufino-Ponce Z, Ali R, 7Ophthalmic Consultants of Boston, Harvard Cremers SL et al. Increased intraocular pressure on the first Medical School, Boston, MA, USA postoperative day following resident-performed cataract E-mail: [email protected] surgery. Eye (Lond) 2011; 25: 929–936. Eye (2012) 26, 332–333; doi:10.1038/eye.2011.274; JY Kim1,2,3, M-W Jo4, SC Brauner3, Z Ferrufino-Ponce5, published online 11 November 2011 R Ali6, SL Cremers3 and BA Henderson7 1Department of Ophthalmology, University of Sir, Ulsan College of Medicine, Asan Medical Center, Retinal pigment epithelial tear resembling retinal Seoul, Republic of Korea tear 2Research Institute for Biomacromolecules, University of Ulsan College of Medicine, Case report Asan Medical Center, Seoul, Republic of Korea A 74-year-old Caucasian female with history of advanced 3Massachusetts Eye and Ear Infirmary, Harvard age-related macular degeneration presented with Medical School, Boston, MA, USA decreased vision in the right eye. The patient was 4Department of Preventive Medicine, University of treated with two ranibizumab injections for choroidal Ulsan College of Medicine, Seoul, Republic of Korea neovascularization 5 months prior without Figure 1 (a) SD-OCT showing RPE defect with overlying intact retina. -
Anterior Segment Surgery and Complications CATARACT EXTRACTION and INTRAOCULAR LENS IMPLANTATION
10 Anterior Segment Surgery and Complications CATARACT EXTRACTION AND INTRAOCULAR LENS IMPLANTATION Complications PENETRATING KERATOPLASTY Complications Correction of Astigmatism in a Corneal Graft LAMELLAR KERATOPLASTY SUPERFICIAL KERATECTOMY EXCIMER LASER PHOTOTHERAPEUTIC KERATECTOMY CONJUNCTIVAL FLAP LIMBAL STEM CELL TRANSPLANTATION PTERYGIUM EXCISION AND CONJUNCTIVAL AUTOGRAFT CONJUNCTIVAL AND CORNEAL TUMOR EXCISION CORNEAL PERFORATION SURGERY PERMANENT KERATOPROSTHESIS REFRACTIVE SURGERY Radial Keratotomy Excimer Laser Photorefractive Keratectomy Laser In Situ Keratomileusis CONCLUSION Anterior segment surgery ranges from routine cataract extraction and lens implantation, one of the most common surgical operations in the United States, to rarely performed surgery such as permanent keratoprosthesis. It also encompasses surgery first performed centuries ago, such as rudimentary pterygium excision, to the latest in keratorefractive surgery. CATARACT EXTRACTION AND INTRAOCULAR LENS IMPLANTATION The many reasons for the development of cataracts are discussed in detail in Chapter 8. Most cataracts are acquired, but they can also be congenital. This section focuses primarily on the treatment of acquired cataracts in adults. Cataracts in adults are generally age related, but some lens opacities may result from other causes such as trauma, inflammation, systemic illness such as diabetes, or medications such as corticosteroids. Cataracts generally advance slowly over years but can advance rapidly over months, or even faster in some patients. The primary indication for cataract extraction is diminished vision caused by the cataract, significantly affecting the patient's lifestyle. The exact point at which this hardship occurs depends on the patient. Certain patients require little visual function and may delay cataract surgery for years or indefinitely. Other patients with high visual needs seek cataract surgery with much smaller degrees of visual loss. -
Role of Temporary Tarsorrhaphy Using Super Glue in the Management of Corneal Disorders
Original Article Role of Temporary Tarsorrhaphy Using Super Glue in the Management of Corneal Disorders Muhammad Moin, Irfan Qayyum, Anwar Ul-Haq Ahmad, Mumtaz Hussain Pak J Ophthalmol 2009, Vol. 25 No. 3 . .. .. See end of article for Purpose: To evaluate the safety and efficacy of temporary tarsorrhaphy using authors affiliations super glue in the management of corneal disorders. … ……………………… Material and Methods: A retrospective chart review of 46 consecutive patients who underwent superglue tarsorrhaphy from June 1997 to June 1998 was Correspondence to: performed. All patients were managed at the Institute of Ophthalmology, Mayo Mohammad Moin hospital, Lahore. This study included patients with painful non healing corneal Department of Ophthalmology ulcers, exposure keratopathy (secondary to moderate proptosis), dry eyes (to Mayo Hospital reduce surface area of evaporation) and post-operative patients with conjunctival Lahore flaps ± scleral grafts (to help take up of the graft). Patients with corneal perforations, endopthalmitis or panophthalmitis were excluded from the study. Temporary tarsorrhaphy was done using super glue technique in which the upper eyelashes were glued to the lower lid skin. The degree of lid closure was calculated according to the pre-existing corneal pathology. Patients were followed up on a weekly basis for one month to check for reduction of pain, improvement of corneal pathology and duration of tarsorrhaphy. Results: There were 50 eyes of 46 patients included in the study who underwent super glue tarsorrhaphy for various corneal pathologies. There were 36 males and 10 female patients with an average age of 40 years (range 10-60 yrs). Thirty two eyes had keratitis (fungal, bacterial, disciform, dendritic), 5 had a persistent epithelial defect, 4 had exposure keratopathy secondary to moderate proptosis, 5 had conjunctival flap alone or combined with a scleral graft and 4 had dry eyes. -
Refractive Management/Intervention 2017-2019
Academy MOC Essentials® Practicing Ophthalmologists Curriculum 2017–2019 Refractive Management/Intervention *** Refractive Management/Intervention 2 © AAO 2017-2019 Practicing Ophthalmologists Curriculum Disclaimer and Limitation of Liability As a service to its members and American Board of Ophthalmology (ABO) diplomates, the American Academy of Ophthalmology has developed the Practicing Ophthalmologists Curriculum (POC) as a tool for members to prepare for the Maintenance of Certification (MOC) -related examinations. The Academy provides this material for educational purposes only. The POC should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed at obtaining the best results. The physician must make the ultimate judgment about the propriety of the care of a particular patient in light of all the circumstances presented by that patient. The Academy specifically disclaims any and all liability for injury or other damages of any kind, from negligence or otherwise, for any and all claims that may arise out of the use of any information contained herein. References to certain drugs, instruments, and other products in the POC are made for illustrative purposes only and are not intended to constitute an endorsement of such. Such material may include information on applications that are not considered community standard, that reflect indications not included in approved FDA labeling, or that are approved for use only in restricted research settings. The FDA has stated that it is the responsibility of the physician to determine the FDA status of each drug or device he or she wishes to use, and to use them with appropriate patient consent in compliance with applicable law. -

Accreditation Council for Graduate Medical Education
Accreditation Council for Graduate Medical Education Ophthalmology Case Logs National Data Report Prepared by: Department of Applications and Data Analysis I. National Resident Statistics Main Table A. This main table provides a national picture of educational experiences. The report is ideal for establishing and assessing national policy related to resident practical experiences. Data is broken out by resident role. B. Descriptive statistics have been carefully chosen to provide the most useful information for judging performance at that national level. i. "Natl Res AVE" - The national average describes the mean number of procedures performed per resident in the nation. ii. "Natl Res STD" - The standard deviation indicates how tightly the scores are clustered around the mean in the set of data. iii. "Natl Res MIN" - The minimum value among procedure counts in the nation. iv. "Natl Res MED" - The median value among procedure counts in the nation. v. "Natl Res MAX" - The maximum value seen among procedure counts in the nation. II. National Benchmark Table for Resident Statistics The table displays selected percentile benchmarks of program averages. For example, a score at the 10th percentile indicates that 10% of residents achieved less than the value while the remaining 90% achieved more than the value. © 2015 Accreditation Council for Graduate Medical Education (ACGME) OPHTHALMOLOGY: NATIONAL RESIDENT REPORT (Main Table) Reporting Period: Total Experience of Residents Completing Programs in 2014-2015 Residency Review Committee for Ophthalmology -

Surgery Prioritization Strategy: Codes for Typical Ophthalmic Procedures
Surgery Prioritization Strategy: Codes for Typical Ophthalmic Procedures Emergent Condition/Service CPT code(s) Endophthalmitis 67015 Aspiration or release of vitreous, subretinal or choroidal fluid, pars plana approach (posterior sclerotomy) 65800 Paracentesis of anterior chamber of eye (separate procedure); with removal of aqueous 67028 Intravitreal injection of a pharmacologic agent (separate procedure) Note: 67028 is bundled with both 67015 and 65800 Open globe, disruption of operative 65275 Repair of laceration; cornea, nonperforating, with or without removal foreign body incision 65280 Repair of laceration; cornea and/or sclera, perforating, not involving uveal tissue 65285 Repair of laceration; cornea and/or sclera, perforating, with reposition or resection of uveal tissue 65286 Repair of laceration; application of tissue glue, wounds of cornea and/or sclera 66250 Revision or repair of operative wound of anterior segment, any type, early or late, major or minor procedure Cantholysis/canthotomy 67715 Canthotomy (separate procedure) Intraocular foreign body 65235 Removal of foreign body, intraocular; from anterior chamber of eye or lens 65260 Removal of foreign body, intraocular; from posterior segment, magnetic extraction, anterior or posterior route 65265 Removal of foreign body, intraocular; from posterior segment, nonmagnetic extraction 67413 Orbitotomy without bone flap (frontal or transconjunctival approach); with removal of foreign body Canalicular lacerations 68700 Plastic repair of canaliculi 67950 Canthoplasty (reconstruction -
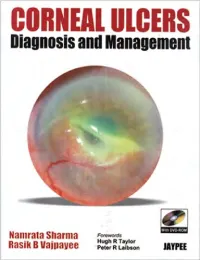
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

Ocular Surgery in Ophthalmic Zoster
Eye (1989) 3, 313-317 Ocular Surgery in Ophthalmic Zoster R. J. MARSH and M. COOPER London Summary Surgical outcome after ophthalmic zoster was analysed with respect to cataract, glaucoma, corneal ulceration and scarring. We used data from the Zoster Clinic and Hospital Activity Analysis (HAA) at Moorfields Eye Hospital and a lipid keratopathy database at the Western Ophthalmic Hospital. Conventional surgery for cataract, glaucoma and corneal scarring gave good results which were probably no different from experience with routine cases, although there was a tendency for prolonged post-operative inflammation. Lateral and central tarsorrhaphy for neuroparalytic ulceration almost invariably led to rapid healing. Many ophthalmologists are apprehensive glaucoma.6 Corneal scarring follows a small about operating on eyes that have been number of nummular, disciform and scle affected by herpes zoster ophthalmicus rokeratitis, sometimes forming a vascularised because they fear peroperative and post lipid keratopathy6 but otherwise complicates operative complications associated with neuroparalytic and exposure keratitis. Whilst inflammation. Therefore elective intraocular ulceration or glaucoma may need surgery surgery tends to be avoided. A survey of the whatever the underlying causes, cataract or literature is disappointing with only small corneal grafts tend to be avoided because the numbers of cases reported. 1,2,7 The com contralateral eye is usually normal. Our data monest complications requiring surgery are intended to help in evaluating the risks associ neuroparalytic ulcers, cataracts, glaucoma ated with such surgery. and corneal scars.1,2 Ulceration occurs in In view of the large number of cases of 6-8% of patients with neuroparalytic keratitis ophthalmic zoster seen at Moorfields Eye and in less than 3% with the chronic exposure Hospital we felt we had a unique opportunity type of keratitis. -

Surgical Case Discussions from Thought Leaders
Supplement to September 2017 CLINICAL CASE COMPENDIUM Surgical Case Discussions From Thought Leaders Editorially independent supported by advertising from Alcon and Topcon. See The Future, Right Now. See where smaller can take you Innovative harness technology allows experienced cavers to e ectively explore even smaller crevices and discover hidden potential. Introducing greater access to the TM YOU’ VE NEVER SEEN smallest of spaces with the new ULTRAVIT® 27+® portfolio. TM TM TM YOUR PROCEDURES QUITE LIKE THIS. The latest innovation from the leader in Micro-Incision Vitrectomy Surgery, the comprehensive MIVS ULTRAVIT ® 27+® portfolio is the smartest way to go smaller. Now you can reduce your incision size with more con dence than ever: TM TM TM • Exceptional access to small tissue planes • Multifunctional tool e ciency with the 7500 cpm ULTRAVIT® 27+® dual pneumatic probe ® 1,2 • Sti ness experience similar to 25+ instrumentation TM TM TM • A complete line of 27+® solutions, including GRIESHABER® instrumentation, laser probe and accessories Featuring next-generation visualization technologies and an intelligent ocular-free design, the NGENUITY® 3D Visualization System establishes TM TM a powerful platform for Digitally Assisted Vitreoretinal Surgery (DAVS). TM © 2014 Novartis 8/14 GAU14020JAD IMPORTANT PRODUCT INFORMATION 1. Data on File: DHF 430 Veri cation Report 2,080.8 Revision 02. CAUTION: Federal (USA) law restricts this device to sale by, or on the order of, a physician. INDICATION: The NGENUITY® 3D Visualization System consists of a 3D stereoscopic, 2. Avery R. Single surgeon experience with an enhanced 25+ vitrectomy probe/entry system. ASRS Poster, 2009. AlconRetina.com high-defi nition digital video camera and workstation to provide magnifi ed stereoscopic images of objects during micro-surgery.