Understanding Acupuncture's Therapeutic Role in America
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How Is Physical Therapy Different from Chiropractic Or Massage?”
“How is physical therapy different from chiropractic or massage?” At Hulst Jepsen Physical Therapy we incorporate techniques similar to what chiropractors and massage therapists use with some key alterations and additions. MANUAL THERAPY Hulst Jepsen physical therapists are trained in joint mobility assessment and joint mobilization techniques of the spine and extremities. We utilize spinal mobilization techniques similar to those chiropractors use with the exception of limiting use of high velocity thrust. We have found high velocity thrust can produce injury and believe it should be used sparingly. Our belief is most neck and back injuries do not need to be “cracked” to get better. Hulst Jepsen physical therapists are also trained in a variety of soft tissue techniques similar to those a massage therapist might use. The difference here would be physical therapists have a significantly greater amount of education in the anatomy of soft tissues (muscles, tendons, ligaments) than massage therapists do. Every patient who comes to Hulst Jepsen Physical Therapy gets some form of “hands on” treatments, be it joint mobilization, soft tissue techniques, isolated muscle stretching or muscle energy (using muscle stretch and contraction to mobilize joints). These manual therapy techniques are important in expediting healing but we believe this is only one piece of treating injuries. MODALITIES Another component of physical therapy is therapeutic modalities. Physical therapists utilize hot packs/cold packs, ultrasound (deep heat utilizing sound waves), electrical stimulation (electrical current to relax muscles and decrease pain and swelling), and iontophresis (patches where medication is electrically pushed into a localized area). TRACTION Physical therapists utilize mechanical traction for neck and back problems. -

Spinal Manipulation — Not an 'Adjustment'
Spinal Manipulation — Not an ‘Adjustment’ How Does Manual Physical Therapy and Chiropractic Differ? By: Joe Waller MPT, Cert. SMT, CMTPT Spinal Manipulation, also known as ‘High-Velocity Low-Amplitude Thrust’ or ‘Spinal Manipulative Therapy’, is an ancient art and science tracing its origins to the earliest of medical practitioners. Practiced principally by physical therapists and chiropractors, it is also utilized to a lesser degree by medical and osteopathic physicians. Spinal manipulation is unique compared with other manual therapy techniques in that the clinician applies a rapid impulse, or thrust, in order to achieve a gapping and subsequent cavitation of the target joint. Joint cavitation is accompanied by an audible release recognized as a ‘popping’, or ‘cracking’, sound. Spinal manipulation is used by physical therapists to facilitate movement, relieve pain, increase circulation, relax muscles, and improve muscle function. A common misconception is that spinal manipulation by a physical therapist is synonymous with a chiropractic adjustment. So the question follows: what is the difference between the two? Between manual physical therapy and chiropractic? While technique application between the professions can be very similar, the two professions operate under divergent treatment models. A clearer understanding of the context and reasoning used to guide treatment will help differentiate between these two professions. The key phrases in the Wisconsin Definition of Chiropractic Practice Act are spinal column adjustment and spinal subluxations and associated nerve energy expression. Most chiropractors, to varying degrees, subscribe to the theory of the ‘spinal subluxation complex’, which asserts that the subluxation of a vertebra actively alters neurological function, which, if left untreated, will lead to disorders and disease of the various organ systems. -

FSBPT Resource Paper Regarding Dry Needling 7Th Edition
FSBPT Resource Paper Regarding Dry Needling 7th edition Federation of State Boards of Physical Therapy December 2017 Original publication: March 8, 2010 The FSBPT would encourage review of the information in this resource paper in order to determine whether dry needling is within the scope of practice for a physical therapist for the jurisdiction in question. The information presented in this paper will provide some background and evidence on which the state licensing authority may wish to base the decision regarding scope of practice. Preface .......................................................................................................................................................... 3 Introduction .................................................................................................................................................. 3 Dry Needling: Terms & Definitions .............................................................................................................. 4 Competencies Required of Physical Therapists to Perform Dry Needling .................................................... 7 Legislative and Regulatory Decisions ............................................................................................................ 7 Dry Needling in the USA (As Of 12/2017) ................................................................................................. 7 State Legislation ....................................................................................................................................... -

The Effect of Chiropractic Manual Therapy on the Spine, Hip and Knee Henry P
University of Wollongong Research Online University of Wollongong Thesis Collection University of Wollongong Thesis Collections 2000 The effect of chiropractic manual therapy on the spine, hip and knee Henry P. Pollard University of Wollongong Recommended Citation Pollard, Henry P., The effect of chiropractic manual therapy on the spine, hip and knee, Doctor of Philosophy thesis, Department of Biomedical Science, University of Wollongong, 2000. http://ro.uow.edu.au/theses/1097 Research Online is the open access institutional repository for the University of Wollongong. For further information contact Manager Repository Services: [email protected]. THE EFFECT OF CHIROPRACTIC MANUAL THERAPY ON THE SPINE, HIP AND KNEE. A thesis submitted in partial fulfillment of the requirements of the award of the degree Ph.D. from THE UNIVERSITY OF WOLLONGONG by HENRY P. POLLARD BSc, Grad Dip Chiropractic, Grad Dip App Sc, M Sport Sc DEPARTMENT OF BIOMEDICAL SCIENCE FACULTY OF HEALTH & BEHAVIOURAL SCIENCES 2000 1 Declaration The work presented in this thesis is the original work of the author except as acknowledged in the text. I, Henry Pollard hereby declare that I have not submitted any material as presented in this thesis either in whole or in part for a degree at this or any other institution. Signed: Date: ui OO 2 Dedication This thesis is dedicated to three very special people in my life. To my mother Rosetta who worked so very hard for so long to enable me the opportunity to seek an education. To my father Don for fostering an environment of encouragement and support. To my wife Grace for providing unconditional support so that I could satisfy my educational needs. -

The Manipulation Education Manual
Manipulation Education Manual For Physical Therapist Professional Degree Programs Manipulation Education Committee APTA Manipulation Task Force Jointly sponsored by: Education Section and Orthopaedic Section, American Physical Therapy Association American Physical Therapy Association American Academy of Orthopaedic Manual Physical Therapists 2004 April 2004 Dear Physical Therapist Educator, As you know, the practice of physical therapy has been under attack on many fronts recently; one of the most aggressive has been directed toward the physical therapist’s ability to provide manual therapy interventions including nonthrust and thrust mobilization/manipulations. APTA has been working with the American Academy of Orthopaedic Manual Physical Therapists (AAOMPT) and the Education and Orthopaedic Sections of APTA, to develop proactive initiatives to combat these attacks. In early 2003, strategies were developed to heighten awareness among academic and clinical faculty of legislative and regulatory threats to physical therapist use of manipulation in practice and in academic instruction. One of these strategies is to promote dialogue and resource sharing among physical therapy faculty regarding instruction, legislation, and regulation in the area of thrust manipulation. The Manipulation Education Manual (MEM) was developed to support the ongoing efforts in physical therapist education programs to provide appropriate, evidence-based instruction in thrust manipulation. Educational preparation of physical therapists for the practice of manipulative -

Can Chiropractors and Evidence-Based Manual Therapists Work Together? an Opinion from a Veteran Chiropractor
Can Chiropractors and Evidence-Based Manual Therapists Work Together? An Opinion From a Veteran Chiropractor Samuel Homola, DC Abstract: Use of manual therapy in the form of manipulation and massage is evident in the earliest recordings of history. Today, manual therapy is an evidence-based practice that can be used with predictable results in the treatment of a variety of neuromusculoskeletal problems. However, for some manual therapists, treatment is still based on a belief system that incorporates vitalism, energy healing, and other metaphysical concepts. Cooperation of practitioners in researching the effects of manual therapy would require uniformity based upon the guidelines of science, following rules for selection of an evidence-based therapy that produces predictable and replicable results. Such an approach would not allow contami- nation by dogma or by an agenda that is designed more to support a belief system than to find the truth. The chiropractic profession, which began with a founding father in 1895, is identified primarily by its use of manipulation. But chiropractic is based upon a vertebral subluxation theory that is generally categorized as supporting a belief system. The words “manipulation” and “subluxation” in a chiropractic context have meanings that are different from the meanings in evidence-based literature. An orthopedic subluxation, a partial disloca- tion or displacement of a joint, can sometimes benefit from manipulation or mobilization when there are joint-related symptoms. A chiropractic subluxation, however, is often an undetectable or asymptomatic “spinal lesion” that is alleged to be a cause of disease. Such a subluxation, which has never been proven to exist, is “adjusted” by chiropractors, who manipulate the spine to restore and maintain health. -

A History of Manipulative Therapy
A History of Manipulative Therapy Erland Pettman, PT, MCSP, MCPA, FCAMT, COMT Abstract: Manipulative therapy has known a parallel development throughout many parts of the world. The earliest historical reference to the practice of manipulative therapy in Europe dates back to 400 BCE. Over the centuries, manipulative interventions have fallen in and out of favor with the medical profession. Manipulative therapy also was initially the mainstay of the two leading alternative health care systems, osteopathy and chiropractic, both founded in the latter part of the 19th century in response to shortcomings in allopathic medicine. With medical and osteopathic physicians initially instrumen- tal in introducing manipulative therapy to the profession of physical therapy, physical therapists have since then provided strong contributions to the fi eld, thereby solidifying the profession’s claim to have manipulative therapy within in its legally regulated scope of practice. Key Words: Manipulative Therapy, Physical Therapy, Chiropractic, Osteopathy, Medicine, History istorically, manipulation can trace its origins from tail in which this is described suggests that the practice of parallel developments in many parts of the world manipulation was well established and predated the 400 BCE Hwhere it was used to treat a variety of musculoskele- reference11. tal conditions, including spinal disorders1. It is acknowl- In his books on joints, Hippocrates (460–385 BCE), who edged that spinal manipulation is and was widely practised in is often referred to as the father of medicine, was the fi rst many cultures and often in remote world communities such physician to describe spinal manipulative techniques using as by the Balinese2 of Indonesia, the Lomi-Lomi of Hawaii3-5, gravity, for the treatment of scoliosis. -

Applied Kinesiology Research and Literature Compendium
APPLIED KINESIOLOGY RESEARCH AND LITERATURE COMPENDIUM -- Edited by Scott Cuthbert, D.C. APPLIED KINESIOLOGY RESEARCH ARTICLES IN PEER REVIEWED JOURNALS Cuthbert SC, Barras M. J Manipulative Physiol Ther. 2009 Oct;32(8):660-9. Developmental delay syndromes: psychometric OBJECTIVE: This study presents a case series of 157 children with developmental delay testing before and after syndromes, including the conditions such as dyspraxia, dyslexia, attention-deficit hyperactivity disorder, and learning disabilities who received chiropractic care. CLINICAL FEATURES: A chiropractic treatment of 157 consecutive sample of 157 children aged 6 to 13 years (86 boys and 71 girls) with difficulties in children. reading, learning, social interaction, and school performance who met these inclusion criteria were included. INTERVENTION AND OUTCOMES: Each patient received a multimodal chiropractic treatment protocol, applied kinesiology chiropractic technique. The outcome measures were a series of 8 standardized psychometric tests given to the children by a certified speech therapist pre- and posttreatment, which evaluate 20 separate areas of cognitive function, including patient- or parent-reported improvements in school performance, social interaction, and sporting activities. Individual and group data showed that at the end of treatment, the 157 children showed improvements in the 8 psychometric tests and 20 areas of cognitive function compared with their values before treatment. Their ability to concentrate, maintain focus and attention, and control impulsivity and their performance at home and school improved. CONCLUSIONS: This report suggests that a multimodal chiropractic method that assesses and treats motor dysfunction reduced symptoms and enhanced the cognitive performance in this group of children. Developmental Delay J Ped Matern Fam Health. -

Orthopedic Manual Therapy for the Pediatric Patient
Orthopedic Manual Therapy for the Pediatric Patient Mitchell Selhorst, DPT, OCS Nationwide Children’s Hospital Sports and Orthopedic PT Columbus, Ohio ………………..…………………………………………………………………………………………………………………………………….. Learning Objectives The attendee will: • Understand the specific precautions and the relative risk of performing orthopedic manual therapy on pediatric patients. • Identify pediatric patients who are appropriate for orthopedic manual therapy. • Use orthopedic manual physical therapy to minimize pain and maximize function in pediatric orthopedic patients. ………………..…………………………………………………………………………………………………………………………………….. Pediatric Physical Therapy ………………..…………………………………………………………………………………………………………………………………….. This is the Pediatric I Mean Kids Need PT Too! Pediatric Pain is Not Benign • Injury in childhood may lead to increased risk of pain in adulthood.23 • Pain does not go away on its own – 2/3 of adolescents with low back pain will have chronic or recurrent symptoms 6 months later.38 Clinical Practice Guidelines Recommend use of Manual Therapy Alright, Let’s Do Manual Therapy! Wait… Growing Children ………………..…………………………………………………………………………………………………………………………………….. Contraindications and Precautions • Contraindication: A circumstance which absolutely rules out the use of a therapeutic method which would otherwise be indicated. • Precaution: The risks of a treatment have to be carefully assessed before treatment is initiated, and it can only be administered if its benefits to the patient are greater than its risks ………………..……………………………………………………………………………………………………………………………………. -

Karen Jean Bailey
Karen J. Bailey WORK EXPERIENCE: November 2002- Owner, Licensed Physical Therapist Present Optimal Performance Physical Therapy, LLC Scarborough, Maine 04074 Outpatient orthopedic and neurological clients, manual therapy, sports medicine, industrial rehab, and neuromuscular dysfunction May 1993 – Licensed Physical Therapist November 2002 Southern Maine Medical Center Biddeford, Maine 04005 Outpatient orthopedics (geriatrics/pediatrics), industrial rehab, sports medicine, manual therapy, neuromuscular dysfunction, acute care inpatient, aquatic therapy, and wound care. EDUCATION: April 2016 New England School of Homeopathy Training Program 2 year course completed November 2013 Approved Kinetic Chain Release (KCR) October 2011 Bachelor of Metaphysical Science, (B.Msc.) University of Sedona Sedona, AZ 86336 November 2007 Doctorate of Naturopathic Ministry (DNM) Trinity College of Natural Health Warsaw, Indiana 46580 May 1993 Bachelor of Science (BS) University of New England Biddeford, Maine 04005 Major: Physical Therapy - GPA: 3.4 PROFESSIONAL CERTIFICATIONS: April 2016 Certificate of Completion 2-year Homeopathy Training Program with Dr. Paul Herscu, ND,MPH, and Dr. Amy Rothenberg, ND of New School of Homeopathy October 2014 Approved Kinetic Chain Release Practitioner Hugh Gilbert, PT October 2011 Ordained Metaphysical Minister / Metaphysical Practitioner October 2008 Completion of 2-year Shamanic Healing Training Program with C. Allie Knowlton, MSW, LCSW, DCSW, Psychotherapist, Teacher of Shamanism and Shamanic Healer & Evelyn C. Rysdyk, -
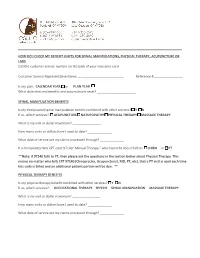
HOW DO I CHECK MY BENEFIT LIMITS for SPINAL MANIPULATIONS, PHYSICAL THERAPY, ACUPUNCTURE OR LABS Call the Customer Service Number on the Back of Your Insurance Card
HOW DO I CHECK MY BENEFIT LIMITS FOR SPINAL MANIPULATIONS, PHYSICAL THERAPY, ACUPUNCTURE OR LABS Call the customer service number on the back of your insurance card. Customer Service Representative Name: Reference #: Is my plan: CALENDAR YEAR or PLAN YEAR What date does my benefits and accumulators reset? SPINAL MANIPULATION BENEFITS Is my chiropractic/spinal manipulation benefit combined with other services? Y N If so, which services?: ACUPUNCTURE NATUROPATHY PHYSICAL THERAPY MASSAGE THERAPY What is my visit or dollar maximum? How many visits or dollars have I used to date? What date of service are my claims processed through? If a chiropractor bills CPT code 97140 “Manual Therapy,” which benefit does it fall to: CHIRO or PT **Note: If 97140 falls to PT, then please ask the questions in the section below about Physical Therapy. This means no matter who bills CPT 97140 (Chiropractor, Acupuncturist, MD, PT, etc), that a PT visit is used each time this code is billed and an additional patient portion will be due. ** PHYSICAL THERAPY BENEFITS Is my physical therapy benefit combined with other services? Y N If so, which services?: OCCUPATIONAL THERAPY SPEECH SPINAL MANIPUATION MASSAGE THERAPY What is my visit or dollar maximum? How many visits or dollars have I used to date? What date of service are my claims processed through? ACUPUNCTURE BENEFITS Is my Acupuncture benefit combined with other services? Y N If so, which services?: CHIROPRACTIC NATUROPATHY PHYSICAL THERAPY MASSAGE THERAPY What is my visit or dollar maximum? How many visits or dollars have I used to date? What date of service are my claims processed through? If an Acupuncturist bills CPT code 97140 “Manual Therapy,” which benefit does it fall to: ACU or PT **Note: If 97140 falls to PT, then please ask the questions in the section for Physical Therapy. -

Manipulative Therapy – Commercial Medical Policy
UnitedHealthcare® Commercial Medical Policy Manipulative Therapy Policy Number: 2021T0541N Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ........................................................................... 1 • Electrical Stimulation for the Treatment of Pain and Definitions ........................................................................................... 2 Muscle Rehabilitation Applicable Codes .............................................................................. 2 • Home Traction Therapy Description of Services ..................................................................... 2 • Manipulation Under Anesthesia Clinical Evidence ............................................................................... 3 • Motorized Spinal Traction U.S. Food and Drug Administration ..............................................17 • References .......................................................................................17 Neuropsychological Testing Under the Medical Policy History/Revision Information..............................................23 Benefit Instructions for Use .........................................................................23 • Spinal Ultrasonography • Temporomandibular Joint Disorders Community Plan Policy • Manipulative Therapy Medicare Advantage Coverage Summary • Chiropractic Services Coverage Rationale Manipulative therapy is proven and medically necessary for treating Musculoskeletal Disorders, except as