The Effectiveness of Levocetirizine in Comparison with Loratadine In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

XYZAL (Levocetirizine Dihydrochloride)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Patients with end-stage renal impairment at less than 10 mL/min These highlights do not include all the information needed to use XYZAL creatinine clearance or patients undergoing hemodialysis (2.3, 4) safely and effectively. See full prescribing information for XYZAL. • Children 6 to 11 years of age with renal impairment (2.3, 4) ® XYZAL (levocetirizine dihydrochloride) ------------------------WARNINGS AND PRECAUTIONS----------------------- 5 mg tablets 2.5 mg/5 mL (0.5 mg/mL) oral solution • Avoid engaging in hazardous occupations requiring complete mental Initial U.S. Approval: 1995 alertness such as driving or operating machinery when taking XYZAL (5.1). ---------------------------RECENT MAJOR CHANGES--------------------------- • Avoid concurrent use of alcohol or other central nervous system Dosage and Administration (2) 01/2008 depressants with XYZAL (5.1). Dosage and Administration, Adults & Children 12 Years & Older (2.1) 01/2008 ------------------------------ADVERSE REACTIONS------------------------------ Dosage and Administration, Children 6 to 11 Years (2.2) 01/2008 The most common adverse reactions (rate ≥2% and > placebo) were ---------------------------INDICATIONS AND USAGE---------------------------- somnolence, nasopharyngitis, fatigue, dry mouth, and pharyngitis in subjects XYZAL is a histamine H1-receptor antagonist indicated for: 12 years of age and older, and pyrexia, somnolence, cough, and epistaxis in • The relief of symptoms associated with seasonal and perennial allergic -

New York State Medicaid Drug Utilization Review Board Meeting Agenda
New York State Medicaid Drug Utilization Review Board Meeting Agenda The Drug Utilization Review (DUR) Board will meet on April 27, 2016, from 9:00 a.m. to 4:00 p.m., Meeting Room 6, Concourse, Empire State Plaza, Albany, New York Agenda Items A. Preferred Drug Program (PDP) The DUR Board will review therapeutic classes listed below, as they pertain to the PDP. The DUR Board will review clinical and financial information, to recommend preferred and non-preferred drugs. For therapeutic classes currently subject to the PDP^, the DUR Board will only consider clinical information which is new since the previous review of the therapeutic class and then consider financial information. New clinical information may include a new drug or drug product information, new indications, new safety information or new published clinical trials (comparative evidence is preferred, or placebo controlled when no head-to-head trials are available). Information in abstract form alone, posters, or unpublished data are poor quality evidence for the purpose of re-review and submission is discouraged. Those wishing to submit new clinical information must do so in an electronic format by April 12, 2016 or the Board may not have ample time to review the information. ^ The current preferred and non-preferred status of drugs subject to the Preferred Drug List (PDL) may be viewed at https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf 1. Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) – Prescription (Previous review date: April 22, 2015) Anaprox DS (naproxen -

MEDICATIONS to AVOID PRIOR to ALLERGY SKIN TESTING Allergy
MEDICATIONS TO AVOID PRIOR TO ALLERGY SKIN TESTING Allergy testing requires the ‘histamine response’ in order to be accurate and reliable. There are many types of antihistamines. Antihistamines are found in many different medicines, either as a single drug or mixed with a combination of chemicals. Please review all medicines you take (including Over-The-Counter) in order to make your allergy testing appointment most efficient and accurate. Generic names are in all lower case, trade names Capitalized. Oral antihistamines to be stopped 3 (THREE) days prior to your appointment: - brompheniramine (Actifed, Atrohist, Dimetapp, Drixoral) - cetirizine (Zyrtec, Zyrtec D) - chlopheniramine (Chlortrimeton, Deconamine, Kronofed A, Novafed A, Rynatan, Tussinex) - clemastine (Tavist, Antihist) - cyproheptadine (Periactin) - diphenhydramine (Benadryl, Allernix, Nytol) - doxylamine (Bendectin, Nyquil) - hydroxyzine (Atarax, Marax, Vistaril) - levocetirizine (Xyzal) - promethazine (Phenergan) Oral antihistamines to be stopped 7 (SEVEN) days prior to your appointment: - desloratadine (Clarinex) - fexofenadine (Allegra, Allegra D) - loratadine (Claritin, Claritin D, Alavert) Nose spray and eye drop antihistamines to stop 5 (FIVE) days prior to your appointment: - azelastine (Astelin, Astepro, Dymista, Optivar) - bepotastine (Bepreve) - ketotifen (Zaditor, Alaway) - olapatadine (Pataday, Patanase) - pheniramine (Visine A, Naphcon A) – OK to stop for 2 days Antacid medications (different type of antihistamine) to stop 3 (THREE) days prior to your appointment: - cimetidine (Tagamet) - famotidine (Pepcid) - ranitidine (Zantac) Note: Antihistamines are found in many over the counter medications, including Tylenol Allergy, Actifed Cold and Allergy, Alka-Seltzer Plus Cold with Cough Formula, and many others. Make sure you read and check the ingredients carefully and stop those containing antihistamines at least 3 (THREE) days prior to the appointment. -

Antihistamines in the Treatment of Chronic Urticaria I Jáuregui,1 M Ferrer,2 J Montoro,3 I Dávila,4 J Bartra,5 a Del Cuvillo,6 J Mullol,7 J Sastre,8 a Valero5
Antihistamines in the treatment of chronic urticaria I Jáuregui,1 M Ferrer,2 J Montoro,3 I Dávila,4 J Bartra,5 A del Cuvillo,6 J Mullol,7 J Sastre,8 A Valero5 1 Service of Allergy, Hospital de Basurto, Bilbao, Spain 2 Department of Allergology, Clínica Universitaria de Navarra, Pamplona, Spain 3 Allergy Unit, Hospital La Plana, Villarreal (Castellón), Spain 4 Service of Immunoallergy, Hospital Clínico, Salamanca, Spain 5 Allergy Unit, Service of Pneumology and Respiratory Allergy, Hospital Clínic (ICT), Barcelona, Spain 6 Clínica Dr. Lobatón, Cádiz, Spain 7 Rhinology Unit, ENT Service (ICEMEQ), Hospital Clínic, Barcelona, Spain 8 Service of Allergy, Fundación Jiménez Díaz, Madrid, Spain ■ Summary Chronic urticaria is highly prevalent in the general population, and while there are multiple treatments for the disorder, the results obtained are not completely satisfactory. The second-generation H1 antihistamines remain the symptomatic treatment option of choice. Depending on the different pharmacokinetics and H1 receptor affi nity of each drug substance, different concentrations in skin can be expected, together with different effi cacy in relation to the histamine-induced wheal inhibition test - though this does not necessarily have repercussions upon clinical response. The antiinfl ammatory properties of the H1 antihistamines could be of relevance in chronic urticaria, though it is not clear to what degree they infl uence the fi nal therapeutic result. Before moving on to another therapeutic level, the advisability of antihistamine dose escalation should be considered, involving increments even above those approved in the Summary of Product Characteristics. Physical urticaria, when manifesting isolatedly, tends to respond well to H1 antihistamines, with the exception of genuine solar urticaria and delayed pressure urticaria. -

Ethylenediamine Dihydrochloride
ETHYLENEDIAMINE DIHYDROCHLORIDE Your patch test result indicates that you have a contact allergy to ethylenediamine dihydrochloride. This contact allergy may cause your skin to react when it is exposed to this substance although it may take several days for the symptoms to appear. Typical symptoms include redness, swelling, itching and fluid-filled blisters. Where is ethylenediamine dihydrochloride found? Ethylenediamine dihydrochloride is a substance that is used to manufacture various drugs and industrial compounds. The most common source of allergic reaction to ethylenediamine dihydrochloride is contact with topical antifungal, antibacterial, and cortisone skin cream mixtures, especially those containing nystatin. It is rarely found in cosmetics and toiletries. Ethylenediamines are one structural class of antihistamines and was used previously as a stabilizing component in topical medicaments such as Mycolog Cream. It is not used as frequently in topical skin care products today and is not found in Mycolog II Cream although it may still be found in some generic nystatin/triamcinolone creams. Because you are allergic to ethylenediamine dihydrochloride, you may have a general skin reaction to antihis- tamine drugs used in the treatment of asthma, hay fever, motion sickness, and hives. A variety of industrial products such as epoxy resins, coolant oils, fungicides, dyes, insecticides, and synthetic waxes also may contain this chemical. How can you avoid contact with ethylenediamine dihydrochloride? Avoid products that list any of the -

Thermodynamic Investigation of Promethazine, Loratadine, Cetirizine and Buclizine As Antihistamine Drugs; Monte Carlo and Semi-Empirical Studies
ISSN-E 1995-9516 Universidad Nacional de Ingeniería COPYRIGHT © (UNI). TODOS LOS DERECHOS RESERVADOS http://revistas.uni.edu.ni/index.php/Nexo https://doi.org/10.5377/nexo.v33i01.10050 Vol. 33, No. 01, pp. 94-108/Junio 2020 THERMODYNAMIC INVESTIGATION OF PROMETHAZINE, LORATADINE, CETIRIZINE AND BUCLIZINE AS ANTIHISTAMINE DRUGS; MONTE CARLO AND SEMI-EMPIRICAL STUDIES INVESTIGACIÓN TERMODINÁMICA DE PROMETAZINA, LORATADINA, CETIRIZINA Y BUCLIZINA COMO MEDICAMENTOS ANTIHISTAMÍNICOS; MONTE CARLO Y ESTUDIOS SEMI-EMPÍRICOS Mina Zakeri1, Majid Monajjemi2*, Ali Ebrahimi3 1Department of Chemistry, Science and Research Branch, Islamic Azad University, Tehran, Iran 2Department of Chemical Engineering, Central Tehran branch, Islamic Azad University Tehran, Iran 3Department of chemistry, Computational Quantum Chemistry Laboratory, University of Sistan and Baluchestan, Iran *[email protected] (recibido/received: 14-diciembre-2019; aceptado/accepted: 21-febrero-2020) ABSTRACT In this article, we discussed about four antihistamine drug called promethazine, loratadine, cetirizine and buclizine. Promethazine in this list is the only one in first generation antihistamine classification with CNS sedation effect and the other three belongs to second generation antihistamine group which are non- sedation and used to treat in many different anti-allergenic fields. In the following we optimized potential, kinetic and total energy of these molecules at body temperature (310 k˚) and environment temperature (298 k ˚) using Mont Carlo method in Amber force field in 500 ns. The quantum mechanics calculations and molecular structure of these molecules investigated using B3LYP level of theory with 6-31 G (d) as a basis set. Theoretical computations were performed to study thermodynamic parameters and frequency analysis. Electronic, thermal, zero point and gibs free energy and enthalpy were estimated in frequency analysis. -

Medications & Allergy Tests
Otolaryngology - Head & Neck Surgery Fairbanks Hearing and Balance Center Richard P. Raugust, M.D. 1919 Lathrop Street, Suite 104 Thomas H. Hammond, M.D. Fairbanks Alaska 99701 Sam Kim, M.D. Phone: (907) 456-7768 Fax: (907) 456-4045 MEDICATIONS & ALLERGY TESTS Medications which Interfere with Allergy Skin Tests Certain over-the-counter and prescriptions medications contain ingredients which affect allergy skin tests. Check labels of all medications you are using (including eye drops and nasal sprays) to determine whether your medication contains any ingredient listed below. For questions regarding ingredients, contact your pharmacist. The medications listed must be held for at least the amount of time indicated prior to allergy skin tests. MINIMUM TIME HELD PRIOR TO EYE DROPS APPOINTMENT Pataday, Patanol, Optivar, Zaditor, Alaway, Elestat, olopatadine, 7 days azelastine, ketotifen, epinastine Pheniramine (e.g. Visine Allergy Eye drops) 48 hours NASAL SPRAYS Pataday, Patanol, Optivar, Zaditor, Alaway, Elestat, Astelin, Astepro, 7 days azelastine, Patanase, olopatidine ORAL MEDICATIONS Benadryl, diphenhydramine (allergy medications and sleep aids) 48 hours doxylamine, pyrilamine, pheniramine (in allergy, cold, and sinus meds) 48 hours Phenergan, promethazine (in prescription cough syrups and anti-nausea) 48 hours Periactin, cyproheptadine (appetite stimulant and other uses) 48 hours meclizine, dimenhydrinate, Antivery, Bonine, Dramamine (motion sickness) 48 hours ranitidine, famotidine, nizatidine (indigestion, heartburn medications) 48 -

Preferred Drug List
October 2021 Preferred Drug List The Preferred Drug List, administered by CVS Caremark® on behalf of Siemens, is a guide within select therapeutic categories for clients, plan members and health care providers. Generics should be considered the first line of prescribing. If there is no generic available, there may be more than one brand-name medicine to treat a condition. These preferred brand-name medicines are listed to help identify products that are clinically appropriate and cost-effective. Generics listed in therapeutic categories are for representational purposes only. This is not an all-inclusive list. This list represents brand products in CAPS, branded generics in upper- and lowercase Italics, and generic products in lowercase italics. PLAN MEMBER HEALTH CARE PROVIDER Your benefit plan provides you with a prescription benefit program Your patient is covered under a prescription benefit plan administered administered by CVS Caremark. Ask your doctor to consider by CVS Caremark. As a way to help manage health care costs, prescribing, when medically appropriate, a preferred medicine from authorize generic substitution whenever possible. If you believe a this list. Take this list along when you or a covered family member brand-name product is necessary, consider prescribing a brand name sees a doctor. on this list. Please note: Please note: • Your specific prescription benefit plan design may not cover • Generics should be considered the first line of prescribing. certain products or categories, regardless of their appearance in • This drug list represents a summary of prescription coverage. It is this document. Products recently approved by the U.S. Food and not all-inclusive and does not guarantee coverage. -

Please Eat Before You Come
List Usual Medications (including Vitamins and Herbal) Richmond Name, Dosage, and Frequency Allergy and PLEASE EAT Asthma 1. Specialists, P.C. BEFORE YOU 2. 3. Name COME IN. 4. Appt. Date: 5. 6. 7. Important Information The following medications 8. Regarding your may be continued: 9. Antibiotics 10. Current Medications Birth Control Pills 11. Cardiac (Heart) Medications and your Appointment Diabetic Medications 12. Hormones 13. Prescription Sedatives Seizure Medications 14. Some medications may interfere Thyroid Medications 15. with allergy testing. Review the Blood Pressure Medications 16. medications inside at least 17. ONE WEEK BEFORE your visit. 18. Call if you have any questions about your 19. medications. RAAS-108 (Rev 08.10.2020) 20. Discontinue 3-5 days before appointment or Do not use the day of the appointment **Check with your prescribing physician before as soon as possible if less than 5 days: stopping any medications. ASTHMA MEDICATIONS: **Read package ingredients of any over the BENADRYL / DIPHENHYDRAMINE (Inhaled Steroids) counter cold/ flu/ sinus and sleep medications. (Stomach Medications) Advair Asmanex Pulmicort Cimetidine Pepcid Breo Dulera Symbicort Famotidine Ranitidine Alvesco Flovent QVAR Discontinue one week before appointment or Metoclopramide Zantac as soon as possible if less than 1 week: Nizatidine (Inhaled Bronchodilators) Acrivastine Dymista Do not use the day of the appointment Albuterol ProAir Advil PM Elavil (Anti-Inflammatory/Pain Medication) Atrovent Proventil Alavert & Alavert D Excedrin PM Combivent -

209089Orig1s000 209090Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209089Orig1s000 209090Orig1s000 CLINICAL REVIEW(S) CLINICAL REVIEW Application Type NDA (Rx to OTC switch) Application Number(s) 209-089 Xyzal Allergy 24 HR tablets 209-090 Xyzal Allergy 24 HR solution Priority or Standard Standard Submit Date(s) March 18, 2016 Received Date(s) March 31, 2016 PDUFA Goal Date January 31, 2017 Division / Office DPARP/ODE 2/OND Reviewer Name(s) Xu Wang, M.D., Ph.D. Review Completion Date December 9, 2016 Established Name Levocetirizine dihydrochloride Rx Trade Name Xyzal tablets/solution OTC Trade Name Xyzal Allergy 24HR tablets/solution Therapeutic Class Antihistamine Applicant UCB Inc. Formulation(s) tablets/solution Dosing Regimen ≥12 years: One tablet (5 mg) daily/10 mL solution (5 mg) daily; 1 6 – 11 years: /2 tablet (2.5 mg) daily/5 mL solution (2.5 mg) daily; 2 – 5 years: 2.5 mL solution (1.25 mg) daily Indication(s) Temporarily relieve these symptoms due to hay fever or other upper respiratory allergies: • running nose, • sneezing, • itchy, watering eyes, • itching of nose or throat Intended Population(s) Tablets: ≥6 years of age Solution: ≥2 years of age Template Version: March 6, 2009 Reference ID: 4025819 Clinical Review Xu Wang, M.D., Ph.D. NDA 209-089/NDA 209-090 Rx to OTC switch Xyzal Allergy 24HR (levocetirizine dihydrochloride) tablets/solution Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT .........................................4 1.1 Recommendation on Regulatory Action ............................................................. 4 1.2 Risk Benefit Assessment .................................................................................... 4 2 INTRODUCTION AND REGULATORY BACKGROUND ........................................ 4 2.1 Product Information ............................................................................................ 4 2.2 Currently Available Treatments for Proposed Indications.................................. -
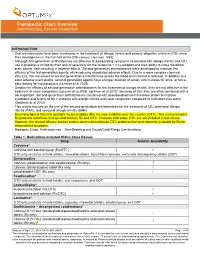
Therapeutic Class Overview Antihistamines, Second Generation
Therapeutic Class Overview Antihistamines, Second Generation INTRODUCTION Oral antihistamines have been a mainstay in the treatment of allergic rhinitis and chronic idiopathic urticaria (CIU) since their development in the first half of the 20th century (Janssen 1993). Although first-generation antihistamines are effective at ameliorating symptoms associated with allergic rhinitis and CIU, use in practice is limited by their lack of selectivity for the histamine 1 (H1)-receptor and their ability to cross the blood- brain barrier, both resulting in adverse effects. Second-generation antihistamines were developed to maintain the efficacy of the first-generation agents, while reducing associated adverse effects. Due to a more complex chemical structure, the movement of second-generation antihistamines across the blood-brain barrier is reduced. In addition to a safer adverse event profile, second-generation agents have a longer duration of action, which allows for once- or twice- daily dosing for most products (Lehman et al 2006). Despite the efficacy of second-generation antihistamines for the treatment of allergic rhinitis, they are not effective in the treatment of nasal congestion (Lehman et al 2006, Seidman et al 2015). Because of this, they are often combined with a decongestant. Second-generation antihistamines combined with pseudoephedrine have been shown to improve symptoms and quality of life in patients with allergic rhinitis and nasal congestion compared to antihistamines alone (Seidman et al 2015). This review focuses on the use of the second-generation antihistamines for the treatment of CIU, perennial allergic rhinitis (PAR), and seasonal allergic rhinitis (SAR). Several products formerly available by prescription (Rx) are now available over-the-counter (OTC). -

High-Risk Medication Pocket Guide
High-Risk Medication Pocket Guide Therapeutic Class High-Risk Medication Potential Risks Alternative Medication Option Antihistamines Brompheniramine, Carbinoxamine, Highly anticholinergic (can cause dry mouth, flushing, dry Allergies: Cetirizine, Fexofenadine, Loratadine, Chlorpheniramine, Clemastine, skin, confusion, or difficulty urinating); Sedation. Levocetirizine (as a single agent or as Cyproheptadine, Dexbrompheniramine, Anxiety: Buspirone, SSRIs (Fluoxetine, Paroxetine), part of a combination Dexchlorpheniramine, Diphenhydramine SNRIs (Venlafaxine, Cymbalta) product) - excludes (oral), Doxylamine, Hydroxyzine, OTC products Promethazine, Triprolidine Insomnia: Melatonin, low-dose Trazodone Anti-Infectives Nitrofurantoin (when cumulative day supply Potential for pulmonary toxicity or peripheral neuropathy Infection: Ciprofloxacin, Trimethoprim/ is >90 days during plan year) (numbness, tingling, or pain in the hands, feet, or toes. Sulfamethoxazole, Amoxicillin/Clavulanate, Muscle weakness. Cephalexin Difficulty walking and/or problems with balance or coordination). Antiparkinson Agents Benztropine (oral), Trihexyphenidyl Highly anticholinergic (can cause dry mouth, flushing, Parkinson Disease: Selegiline, dry skin, confusion, or difficulty urinating); Carbidopa/Levodopa, Ropinirole, Pramipexole, Not recommended for prevention of extrapyramidal Entacapone symptoms with antipsychotics due to potential Antipsychotic induced Extrapyramidal Symptoms: hallucinations. Quetiapine, Clozapine Antipsychotics Thioridazine Highly anticholinergic