Reducing the Risks from Radon: Information and Interventions a Guide for Health Care Providers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Is Radon?
Biology Unit Radon Alert INVESTIGATION 3 WHAT IS RADON? INTRODUCTION Radon is a naturally occurring radioactive gas. It is formed by the radioactive breakdown of radium, and is found in soils just about everywhere. You cannot see it, taste it, or smell it. It is continuously formed in rocks and soils and escapes into the atmosphere. In some cases, it makes its way into homes, builds up to high concentrations in indoor air, and can become a health hazard. Although there are several different isotopes of radon, the one that is of greatest concern as a potential Radioactivity - the spontaneous human health threat is called radon-222. Radon-222 is emission of energy by certain (radio- formed naturally during a chain of radioactive disintegra- active) atoms, resulting in a change tion reactions (decay series). The decay series begins from one element to another or one when uranium-238 decays. Uranium is widely distrib- isotope to another. The energy can uted in rocks and soils throughout the earth’s crust. It has be in the form of alpha or beta par- a half-life of 4.5 billion years, which means a very slow ticles and gamma rays. breakdown. The decay series is shown schematically in Figure 1. There are eight different elements and 15 different isotopes in the series, beginning with uranium- 238 and ending with lead-206. New elements formed by radioactive disintegration reactions are called decay products. Thus, radium-226 is one of the decay products of uranium-238. Polonium-218 and lead-214 are decay products of radon-222. -

Vapor Intrusion? Can You Get Sick from Vapor Vapor Intrusion Refers to the Vapors Produced by a Chemical Intrusion? Spill/Leak That Make Their Way Into Indoor Air
Bureau of Environmental Health Health Assessment Section VVaappoorr IInnttrruussiioonn “To protect and improve the health of all Ohioans” Answers to Frequently Asked Health Questions What is vapor intrusion? Can you get sick from vapor Vapor intrusion refers to the vapors produced by a chemical intrusion? spill/leak that make their way into indoor air. When intrusion? You can get sick from breathing harmful chemical chemicals are spilled on the ground or leak from an vapors. But getting sick will depend on: underground storage tank, they will seep into the soils and How much you were exposed to (dose). will sometimes make their way into the groundwater How long you were exposed (duration). (underground drinking water). There are a group of How often you were exposed (frequency). chemicals called volatile organic compounds (VOCs) that How toxic the spill/leak chemicals are. easily produce vapors. These vapors can travel through General Health, age, lifestyle: Young children, the soils, especially if the soils are sandy and loose or have a lot elderly and people with chronic (on-going) health of cracks (fissures). These vapors can then enter a home problems are more at risk to chemical exposures. through cracks in the foundation or into a basement with a dirt floor or concrete slab. VOC vapors at high levels can cause a strong petroleum or solvent odor and some persons may VOCs and vapors: experience eye and respiratory irritation, headache VOCs can be found in petroleum products such as gasoline and/or nausea (upset stomach). These symptoms or diesel fuels, in solvents used for industrial cleaning and are usually temporary and go away when the person are also used in dry cleaning. -
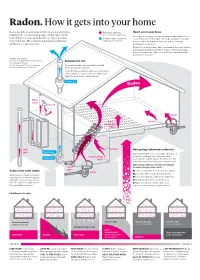
Radon. How It Gets Into Your Home
Radon. How it gets into your home Radon gas kills an estimated 21,000 Americans every year, Radon gas entering How it gets in your home making it the second-leading cause of lung cancer in the home from below ground Loose pipes, unsealed cracks and sump crocks (a basin in the United States. You are most likely to be exposed to it in Common ways to remove concrete basement oor that collects groundwater seepage) your own home. Here’s how radon gets into your home radon gas from home can be points of entry for radon as it seeps up through and how you can get rid of it. permeable rock and soil. Regardless of your home's base, any break in the seal between ground and foundation can allow radon to enter and escape into your living areas. Higher oors will see less radon as the particulates dissipate. Advance Local graphic. Sources: U.S. Department of the Interior Reducing the risk U.S. Geological Survey U.S. Environmental Protection Agency Once radon levels are conrmed to be high, Minnesota Department of Health there are ways to remove it. Leaks that allow radon to enter are sealed and a radon mitigation system, left, is installed that vents the particulates safely outside. Radon fan Water pipes Faucet Drain Gaps in Cracks suspended oors Well Cracks How geology determines radon risk pipe Radon pipe Highly permeable soil or rock types oer less of Construction a barrier to radon present below ground. Suction pit joints Generally, the harder packed the ground is, the lower the chance of having radon in your home. -

Of the Periodic Table
of the Periodic Table teacher notes Give your students a visual introduction to the families of the periodic table! This product includes eight mini- posters, one for each of the element families on the main group of the periodic table: Alkali Metals, Alkaline Earth Metals, Boron/Aluminum Group (Icosagens), Carbon Group (Crystallogens), Nitrogen Group (Pnictogens), Oxygen Group (Chalcogens), Halogens, and Noble Gases. The mini-posters give overview information about the family as well as a visual of where on the periodic table the family is located and a diagram of an atom of that family highlighting the number of valence electrons. Also included is the student packet, which is broken into the eight families and asks for specific information that students will find on the mini-posters. The students are also directed to color each family with a specific color on the blank graphic organizer at the end of their packet and they go to the fantastic interactive table at www.periodictable.com to learn even more about the elements in each family. Furthermore, there is a section for students to conduct their own research on the element of hydrogen, which does not belong to a family. When I use this activity, I print two of each mini-poster in color (pages 8 through 15 of this file), laminate them, and lay them on a big table. I have students work in partners to read about each family, one at a time, and complete that section of the student packet (pages 16 through 21 of this file). When they finish, they bring the mini-poster back to the table for another group to use. -

Basic Radon Facts
Connecticut Department of Public Health Environmental Health Section Radon Program 410 Capitol Avenue, MS# 21 RAD PO Box 340308 Hartford, CT 06134-0308 June 2016 Basic Radon Facts Radon is a cancer causing, radioactive gas Radon is a naturally occurring, radioactive gas released in rock, soil, and water formed from the breakdown of uranium. Levels in outdoor air pose a low threat to human health. However, radon can enter homes from surrounding soil and become a health hazard inside buildings. Radon does not cause symptoms. You can’t see it or smell it, but an elevated radon level in your home may be affecting the health of your family. Breathing radon over prolonged periods may damage lung tissue. Exposure to radon is the leading cause of lung cancer in nonsmokers in the United States. The U.S. Environmental Protection Agency (EPA) estimates that radon causes more than 20,000 lung cancer deaths in the country each year. Only smoking causes more lung cancer deaths. If you smoke and your home has radon, your risk of developing lung cancer can be much higher. Radon is found all over the United States Radon has been found in elevated levels in homes in every state. High radon concentrations can occur sporadically in all parts of Connecticut. Two homes right next to each other can have different radon levels. Just because your neighbor’s house doesn’t have an elevated level of radon does not mean that your house will also have a low radon level. The only way to know if you have an elevated radon level above the EPA action level of 4 pCi/L is to test your home’s indoor air. -

Keeping Your Home Safe from RADON
Keeping Your Home Safe From RADON 800-662-9278 | Michigan.gov/radon 08/2019 What is Radon? Radon is a colorless and odorless gas that comes from the soil. The gas can accumulate in our home and in the air we breathe. Radon gas decays into fine particles that are radioactive. When inhaled, these fine particles can damage the lung. Exposure to radon over a long period of time can lead to lung cancer. It is estimated that 21,000 people die each year in the United States from lung cancer due to radon exposure. A radon test is the only way to know how much radon is in your home. Radon can be reduced with a mitigation system. The Michigan Department of Environment, Great Lakes, and Energy (EGLE) has created this guide to explain: • How radon accumulates in homes • The health risks of radon exposure • How to test your home for radon • What to do if your home has high radon • Radon policies C Keeping Your Home Safe From Radon Table of Contents Where Does Radon Come From? ............................................. 1 Radon in Michigan ....................................................................... 1 Percentage of Elevated Radon Test Results by County ......... 2 Is There a Safe Level of Radon? ............................................... 3 Radon Health Risks ..................................................................... 4 How Radon Enters the Home ..................................................... 6 Radon Pathways ........................................................................... 7 Radon Testing ............................................................................ -

Radionuclides (Including Radon, Radium and Uranium)
Radionuclides (including Radon, Radium and Uranium) Hazard Summary Uranium, radium, and radon are naturally occurring radionuclides found in the environment. No information is available on the acute (short-term) noncancer effects of the radionuclides in humans. Animal studies have reported inflammatory reactions in the nasal passages and kidney damage from acute inhalation exposure to uranium. Chronic (long-term) inhalation exposure to uranium and radon in humans has been linked to respiratory effects, such as chronic lung disease, while radium exposure has resulted in acute leukopenia, anemia, necrosis of the jaw, and other effects. Cancer is the major effect of concern from the radionuclides. Radium, via oral exposure, is known to cause bone, head, and nasal passage tumors in humans, and radon, via inhalation exposure, causes lung cancer in humans. Uranium may cause lung cancer and tumors of the lymphatic and hematopoietic tissues. EPA has not classified uranium, radon or radium for carcinogenicity. Please Note: The main sources of information for this fact sheet are EPA's Integrated Risk Information System (IRIS) (5), which contains information on oral chronic toxicity and the RfD for uranium, and the Agency for Toxic Substances and Disease Registry's (ATSDR's) Toxicological Profiles for Uranium, Radium, and Radon. (1) Uses Uranium is used in nuclear power plants and nuclear weapons. Very small amounts are used in photography for toning, in the leather and wood industries for stains and dyes, and in the silk and wood industries. (2) Radium is used as a radiation source for treating neoplastic diseases, as a radon source, in radiography of metals, and as a neutron source for research. -
Recalling Radon's Recognition
in your element Recalling radon’s recognition Brett F. Thornton and Shawn C. Burdette look back at the discovery — and the many different names — of element 86. n 1899, Pierre and Marie Curie noted an Thoron, unlike radon, requires no such “induced radioactivity” — left behind by clarification, and 220Rn is routinely called Iradium, distinct from its own radioactivity. thoron today. Thoron is far easier to say Ernest Rutherford and Robert B. Owens also than ‘radon-two-twenty’, perhaps explaining reported that year on a radioactive substance why the annual count of scientific papers 220 ( Rn, t1/2 = 55.6 s) emitted by thorium, which mentioning thoron has increased over twenty- they called emanation. In 1900, Friedrich fold since thoron was ‘disallowed’ in 1957. Dorn realized that the Curies had observed a Distinguishing between 222Rn (the 222 220 unique substance ( Rn, t1/2 = 3.8 d), similar isotope called ‘radon’) and Rn (thoron) is to emanation. In 1904, André-Louis Debierne not of idle linguistic and historic interest. 222 found a third radioactive particle; this one © SUPERSTOCK/ALAMY Rn can persist indoors, whereas the short- 219 produced from actinium ( Rn, t1/2 = 4 s). lived thoron cannot. Not all home radon These were at first regarded as elements and actinon (An) for the three isotopes; detectors (pictured) are sensitive to thoron, and became colloquially known as thorium names suggested by Elliott Q. Adams. and thoron-sensitive detectors must be emanation, radium emanation and actinium An official statement on a name for all placed with care because thoron does not emanation, but today we recognize them three isotopes — that is, a name for the travel far from its source. -
Radon Products
Protect Your Home and Family From Radon Radon is a radioactive emission of uranium with high concentrations found in many areas. Radon rises from the soil and into the home where this radioactive carcinogen may be inhaled by occupants. The EPA estimates that over 20,000 deaths each year are radon related making it the second leading cause of lung cancer deaths. The most common solution to reduce radon exposure is through fan-powered mitigation systems. Side Wall Radon Mitigation System RADON VAC™ Studies Show Side Wall Venting is Safe, Simple and Saves!* Tjernlund is the originator and leading manufacturer of Side Wall Vent systems for gas and oil heaters. Now, Tjernlund has developed the first engineered solu- tion for Side Wall Venting radon gas. System includes: Sealed blower with 3" PVC connectors and a patent pending high velocity discharge hood. Avoid the Costs and Hassles of Running PVC Through the Roof Compare the Total Installed Cost! Avoid Ugly, Intrusive Pipe Runs With Radon VAC:You Save Avoid these hassles: No Electrician $ 125 No Routing PVC Through Living Spaces No Roof Terminus $ 25 No Ladder/Roof Climbing No Couplings $ 20 No Ugly PVC or Fan on Home Exterior No Condensate Drain $ 25 No Rain/Condensation in PVC No Extra PVC $ 50 No Fan Orientation Restrictions No Extra Hardware $ 40 No Extra PVC Routing No Extra Labor $200 No Guessing on Fan Size/Model $485 Patent Pending Variable Easy Installation Sealed Housing for Safety Aspiration Control Both fan and hood directly connect Custom fitted gaskets through- Easily adjust the discharge hood to 3” PVC. -

The Noble Gases
INTERCHAPTER K The Noble Gases When an electric discharge is passed through a noble gas, light is emitted as electronically excited noble-gas atoms decay to lower energy levels. The tubes contain helium, neon, argon, krypton, and xenon. University Science Books, ©2011. All rights reserved. www.uscibooks.com Title General Chemistry - 4th ed Author McQuarrie/Gallogy Artist George Kelvin Figure # fig. K2 (965) Date 09/02/09 Check if revision Approved K. THE NOBLE GASES K1 2 0 Nitrogen and He Air P Mg(ClO ) NaOH 4 4 2 noble gases 4.002602 1s2 O removal H O removal CO removal 10 0 2 2 2 Ne Figure K.1 A schematic illustration of the removal of O2(g), H2O(g), and CO2(g) from air. First the oxygen is removed by allowing the air to pass over phosphorus, P (s) + 5 O (g) → P O (s). 20.1797 4 2 4 10 2s22p6 The residual air is passed through anhydrous magnesium perchlorate to remove the water vapor, Mg(ClO ) (s) + 6 H O(g) → Mg(ClO ) ∙6 H O(s), and then through sodium hydroxide to remove 18 0 4 2 2 4 2 2 the carbon dioxide, NaOH(s) + CO2(g) → NaHCO3(s). The gas that remains is primarily nitrogen Ar with about 1% noble gases. 39.948 3s23p6 36 0 The Group 18 elements—helium, K-1. The Noble Gases Were Kr neon, argon, krypton, xenon, and Not Discovered until 1893 83.798 radon—are called the noble gases 2 6 4s 4p and are noteworthy for their rela- In 1893, the English physicist Lord Rayleigh noticed 54 0 tive lack of chemical reactivity. -

Indoor Air Quality in Tighter Homes
Building Science Bootcamp Indoor Air-Quality (IAQ) Effective and Efficient IAQ Strategies in Residential Buildings This presentation is the intellectual property of Carbon Neutral Group Consulting LLC, and duplication or distribution without licensing or without written legal consent is prohibited and protected by intellectual property law. Building Science Bootcamp Indoor Air-Quality (IAQ) Table of Contents: 1. Radon Sources and Risk, 2. Soil-Gas Mitigation & Moisture Management Strategies, 3. Radon System Performance, 4. Exhaust-Only Ventilation, 5. Balanced Ventilation, A Building Science Bootcamp Indoor Air-Quality - Radon Radon Measurement Questions… • Is radon testing mandatory in new construction after occupancy*? • Do tighter homes need passive or active radon systems? • Residential re-sale test required, however... • Short-term test results vary widely by testing conditions. * The answer is no, new homes are not required to test for radon after construction. Building Science Bootcamp Indoor Air Quality in Tighter Homes • Tighter homes more readily depressurize when exhaust equipment is operated, making combustion appliances more prone to backdraft or spillage, • Tighter buildings are also associated with elevated indoor radon concentrations, in addition to moisture problems, • The US Environmental Protection Agency developed a protocol for guiding professional home energy upgrades while maintaining healthy IEQ for the occupants, • However, the variability remains wide in the quality of energy-retrofitting services provided by weatherization contractors, which in turn affects indoor air quality in the retrofitted homes. Building Science Bootcamp Indoor Air-Quality - Radon What is Radon? A radioactive isotope given off by decomposing trace-uranium, that when inhaled, has been shown in scientific studies to cause lung cancer. -

Radon in the Helium-Bearing Natural Gas of the Texas Panhandle
ej f Radon in the Helium-Bearing Natural Gas of the Texas Panhandle Trace Elements Memorandum Report 239 IN REPLY REFER TO: UNITED STATES DEPARTMENT OF THE INTERIOR GEOLOGICAL SURVEY WASHINGTON 25, D. C. AEC-4-98/1 Dr0 Phillip L 0 Merritt, Assistant Manager Raw Materials Operations U0 So Atomic Energy Commission Po 00 Box 30? Ansonia Station New York 23, New York Dear Phils Transmitted herewith for your information and distribution are 8 copies of Trace Elements Memorandum Report 239 9 "Radon in the helium=>bearing natural gas of the Texas Panhandle," by H0 Faul, Go Eo Mangerj and A0 Y0 Sakakura 0 Our measurements of the radon content of natural gas samples from 84 producing wells in the Texas Panhandle gas field show signifi- cant differences5 furthermore 9 the wells with the highest radon content occur in clusters suggesting a marked variation in the distribution of the parent elements of radon, namely radium and uranium., within or near the gas reservoir., Analysis of the radon data in relation to possible source distribution suggests that rocks containing average concentrations of uranium could not supply the amount of radon observed in most of the gas wellso Further research on the emanating power of granite and dolo mite is required to determine whether the radon observed is attributable to radioactive elements in the reservoir rock or to radioactive elements outside the reservoir volume proper0 The Oak Ridge National Laboratory k©s already initiated preliminary studies of the emanating power of the selected dolomite samples 0 Additional radon measurements, are needed to establish the limits of the abnormal radon concentration and further delineate the possible distribution of the parent !.element 0 Sincerely yours., '^SvwA^ W0 H Bradley I Chief Geologist fITED STATES DEPARTMENT OF THE INTERIOR GEOLOGICAL SURVEY RADON IN THE HELIUM-BEARING NATURAL GAS OF THE TEXAS PANHANDLE H.