Evaluation of Common Genetic Variants in 82 Candidate Genes As Risk Factors for Neural Tube Defects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PDF Document Created by Pdffiller
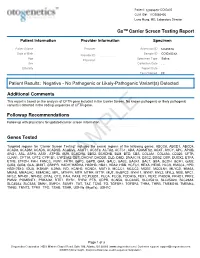
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

Neurodevelopmental Signatures of Narcotic and Neuropsychiatric Risk Factors in 3D Human-Derived Forebrain Organoids
Molecular Psychiatry www.nature.com/mp ARTICLE OPEN Neurodevelopmental signatures of narcotic and neuropsychiatric risk factors in 3D human-derived forebrain organoids 1 1 1 1 2 2 3 Michael Notaras , Aiman Lodhi , Estibaliz✉ Barrio-Alonso , Careen Foord , Tori Rodrick , Drew Jones , Haoyun Fang , David Greening 3,4 and Dilek Colak 1,5 © The Author(s) 2021 It is widely accepted that narcotic use during pregnancy and specific environmental factors (e.g., maternal immune activation and chronic stress) may increase risk of neuropsychiatric illness in offspring. However, little progress has been made in defining human- specific in utero neurodevelopmental pathology due to ethical and technical challenges associated with accessing human prenatal brain tissue. Here we utilized human induced pluripotent stem cells (hiPSCs) to generate reproducible organoids that recapitulate dorsal forebrain development including early corticogenesis. We systemically exposed organoid samples to chemically defined “enviromimetic” compounds to examine the developmental effects of various narcotic and neuropsychiatric-related risk factors within tissue of human origin. In tandem experiments conducted in parallel, we modeled exposure to opiates (μ-opioid agonist endomorphin), cannabinoids (WIN 55,212-2), alcohol (ethanol), smoking (nicotine), chronic stress (human cortisol), and maternal immune activation (human Interleukin-17a; IL17a). Human-derived dorsal forebrain organoids were consequently analyzed via an array of unbiased and high-throughput analytical approaches, including state-of-the-art TMT-16plex liquid chromatography/mass- spectrometry (LC/MS) proteomics, hybrid MS metabolomics, and flow cytometry panels to determine cell-cycle dynamics and rates of cell death. This pipeline subsequently revealed both common and unique proteome, reactome, and metabolome alterations as a consequence of enviromimetic modeling of narcotic use and neuropsychiatric-related risk factors in tissue of human origin. -

Abstracts from the 9Th Biennial Scientific Meeting of The
International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):15 DOI 10.1186/s13633-017-0054-x MEETING ABSTRACTS Open Access Abstracts from the 9th Biennial Scientific Meeting of the Asia Pacific Paediatric Endocrine Society (APPES) and the 50th Annual Meeting of the Japanese Society for Pediatric Endocrinology (JSPE) Tokyo, Japan. 17-20 November 2016 Published: 28 Dec 2017 PS1 Heritable forms of primary bone fragility in children typically lead to Fat fate and disease - from science to global policy a clinical diagnosis of either osteogenesis imperfecta (OI) or juvenile Peter Gluckman osteoporosis (JO). OI is usually caused by dominant mutations affect- Office of Chief Science Advsor to the Prime Minister ing one of the two genes that code for two collagen type I, but a re- International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):PS1 cessive form of OI is present in 5-10% of individuals with a clinical diagnosis of OI. Most of the involved genes code for proteins that Attempts to deal with the obesity epidemic based solely on adult be- play a role in the processing of collagen type I protein (BMP1, havioural change have been rather disappointing. Indeed the evidence CREB3L1, CRTAP, LEPRE1, P4HB, PPIB, FKBP10, PLOD2, SERPINF1, that biological, developmental and contextual factors are operating SERPINH1, SEC24D, SPARC, from the earliest stages in development and indeed across generations TMEM38B), or interfere with osteoblast function (SP7, WNT1). Specific is compelling. The marked individual differences in the sensitivity to the phenotypes are caused by mutations in SERPINF1 (recessive OI type obesogenic environment need to be understood at both the individual VI), P4HB (Cole-Carpenter syndrome) and SEC24D (‘Cole-Carpenter and population level. -

Anti-MMAB Antibody (ARG55862)
Product datasheet [email protected] ARG55862 Package: 100 μl anti-MMAB antibody Store at: -20°C Summary Product Description Rabbit Polyclonal antibody recognizes MMAB Tested Reactivity Hu Predict Reactivity Ms Tested Application WB Host Rabbit Clonality Polyclonal Isotype IgG Target Name MMAB Antigen Species Human Immunogen KLH-conjugated synthetic peptide corresponding to aa. 50-81 (Center) of Human MMAB. Conjugation Un-conjugated Alternate Names ATR; cob; cblB; CFAP23; Cob(I)yrinic acid a,c-diamide adenosyltransferase, mitochondrial; EC 2.5.1.17; Cob(I)alamin adenosyltransferase; Methylmalonic aciduria type B protein Application Instructions Application table Application Dilution WB 1:1000 Application Note * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Positive Control HepG2 Calculated Mw 27 kDa Properties Form Liquid Purification Purification with Protein A and immunogen peptide. Buffer PBS and 0.09% (W/V) Sodium azide Preservative 0.09% (W/V) Sodium azide Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C or below. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. Note For laboratory research only, not for drug, diagnostic or other use. www.arigobio.com 1/2 Bioinformation Database links GeneID: 326625 Human Swiss-port # Q96EY8 Human Gene Symbol MMAB Gene Full Name methylmalonic aciduria (cobalamin deficiency) cblB type Background This gene encodes a protein that catalyzes the final step in the conversion of vitamin B(12) into adenosylcobalamin (AdoCbl), a vitamin B12-containing coenzyme for methylmalonyl-CoA mutase. -

Oral Presentations
Journal of Inherited Metabolic Disease (2018) 41 (Suppl 1):S37–S219 https://doi.org/10.1007/s10545-018-0233-9 ABSTRACTS Oral Presentations PARALLEL SESSION 1A: Clycosylation and cardohydrate disorders O-002 Link between glycemia and hyperlipidemia in Glycogen Storage O-001 Disease type Ia Hoogerland J A1, Hijmans B S1, Peeks F1, Kooijman S3, 4, Bos T2, Fertility in classical galactosaemia, N-glycan, hormonal and inflam- Bleeker A1, Van Dijk T H2, Wolters H1, Havinga R1,PronkACM3, 4, matory gene expression interactions Rensen P C N3, 4,MithieuxG5, 6, Rajas F5, 6, Kuipers F1, 2,DerksTGJ1, Reijngoud D1,OosterveerMH1 Colhoun H O1,Rubio-GozalboME2,BoschAM3, Knerr I4,DawsonC5, Brady J J6,GalliganM8,StepienKM9, O'Flaherty R O7,MossC10, 1Dep Pediatrics, CLDM, Univ of Groningen, Groningen, Barker P11, Fitzgibbon M C6, Doran P8,TreacyEP1, 4, 9 Netherlands, 2Lab Med, CLDM, Univ of Groningen, Groningen, Netherlands, 3Dep of Med, Div of Endocrinology, LUMC, Leiden, 1Dept Paediatrics, Trinity College Dublin, Dublin, Ireland, 2Dept Paeds and Netherlands, 4Einthoven Lab Exp Vasc Med, LUMC, Leiden, Clin Genetics, UMC, Maastricht, Netherlands, 3Dept Paediatrics, AMC, Netherlands, 5Institut Nat Sante et Recherche Med, Lyon, Amsterdam, Netherlands, 4NCIMD, TSCUH, Dublin, Ireland, 5Dept France, 6Univ Lyon 1, Villeurbanne, France Endocrinology, NHS Foundation Trust, Birmingham, United Kingdom, 6Dept Clin Biochem, MMUH, Dublin, Ireland, 7NIBRT Glycoscience, Background: Glycogen Storage Disease type Ia (GSD Ia) is an NIBRT, Dublin, Ireland, 8UCDCRC,UCD,Dublin,Ireland,9NCIMD, inborn error of glucose metabolism characterized by fasting hypo- MMUH, Dublin, Ireland, 10Conway Institute, UCD, Dublin, Ireland, glycemia, hyperlipidemia and fatty liver disease. We have previ- 11CBAL, NHS Foundation, Cambridge, United Kingdom ously reported considerable heterogeneity in circulating triglycer- ide levels between individual GSD Ia patients, a phenomenon that Background: Classical Galactosaemia (CG) is caused by deficiency of is poorly understood. -

Case Report Methylmalonic Acidemia with Novel MUT Gene Mutations
Case Report Methylmalonic Acidemia with Novel MUT Gene Mutations Commented [A 1]: Important: 1.As per the journal, units of measurement should be Inusha Panigrahi, Savita Bhunwal, Harish Varma, and Simranjeet Singh presented simply and concisely using System International (SI) units; please ensure that units are Department of Pediatrics, Advanced Pediatric Centre, PGIMER, Chandigarh, India presented using the SI system at all instances. 2.References for some previously published data is Correspondence: Inusha Panigrahi; [email protected] missing. Please ensure that references are provided Methylmalonic acidemia (MMA) is a rare inherited metabolic disorder caused by deficiency wherever required. of the enzyme methylmalonyl-CoA mutase. The disease is presented in early infancy by 3.Informed consent from the patient is required and lethargy, vomiting, failure to thrive, encephalopathy and is deadly if left untreated. A 5-years should be mentioned in the manuscript. old boy presented with recurrent episodes of fever, feeding problems, lethargy, from the age of For more information, please refer to the guidelines at 11 months, and poor weight gain. He was admitted and evaluated for metabolic causes and https://www.hindawi.com/journals/crig/guidelines/. diagnosed as methylmalonic acidemia (MMA). He was treated with vit B12 and carnitine Commented [A 2]: As per the journal’s guidelines, supplements and has been on follow-up for the last 3 years. Mutation analysis by next please provide email addresses of all the authors. generation sequencing (NGS), supplemented with Sanger sequencing, revealed two novel Formatted: Right: 0 cm, Space Before: 0 pt, Line variants in the MUT gene responsible for MMA in exon 5 and exon 3. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

2021 Code Changes Reference Guide
Boston University Medical Group 2021 CPT Code Changes Reference Guide Page 1 of 51 Background Current Procedural Terminology (CPT) was created by the American Medical Association (AMA) in 1966. It is designed to be a means of effective and dependable communication among physicians, patients, and third-party payers. CPT provides a uniform coding scheme that accurately describes medical, surgical, and diagnostic services. CPT is used for public and private reimbursement systems; development of guidelines for medical care review; as a basis for local, regional, and national utilization comparisons; and medical education and research. CPT Category I codes describe procedures and services that are consistent with contemporary medical practice. Category I codes are five-digit numeric codes. CPT Category II codes facilitate data collection for certain services and test results that contribute to positive health outcomes and quality patient care. These codes are optional and used for performance management. They are alphanumeric five-digit codes with the alpha character F in the last position. CPT Category III codes represent emerging technologies. They are alphanumeric five-digit codes with the alpha character T in the last position. The CPT Editorial Panel, appointed by the AMA Board of Trustees, is responsible for maintaining and updating the CPT code set. Purpose The AMA makes annual updates to the CPT code set, effective January 1. These updates include deleted codes, revised codes, and new codes. It’s important for providers to understand the code changes and the impact those changes will have to systems, workflow, reimbursement, and RVUs. This document is meant to assist you with this by providing a summary of the changes; a detailed breakdown of this year’s CPT changes by specialty, and HCPCS Updates for your reference. -

Molecular Diagnostic Requisition
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 MOLECULAR DIAGNOSTIC REQUISITION PATIENT INFORMATION SAMPLE INFORMATION NAME: DATE OF COLLECTION: / / LAST NAME FIRST NAME MI MM DD YY HOSPITAL#: ACCESSION#: DATE OF BIRTH: / / GENDER (Please select one): FEMALE MALE MM DD YY SAMPLE TYPE (Please select one): ETHNIC BACKGROUND (Select all that apply): UNKNOWN BLOOD AFRICAN AMERICAN CORD BLOOD ASIAN SKELETAL MUSCLE ASHKENAZIC JEWISH MUSCLE EUROPEAN CAUCASIAN -OR- DNA (Specify Source): HISPANIC NATIVE AMERICAN INDIAN PLACE PATIENT STICKER HERE OTHER JEWISH OTHER (Specify): OTHER (Please specify): REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: INDICATION FOR STUDY SYMPTOMATIC (Summarize below.): *FAMILIAL MUTATION/VARIANT ANALYSIS: COMPLETE ALL FIELDS BELOW AND ATTACH THE PROBAND'S REPORT. GENE NAME: ASYMPTOMATIC/POSITIVE FAMILY HISTORY: (ATTACH FAMILY HISTORY) MUTATION/UNCLASSIFIED VARIANT: RELATIONSHIP TO PROBAND: THIS INDIVIDUAL IS CURRENTLY: SYMPTOMATIC ASYMPTOMATIC *If family mutation is known, complete the FAMILIAL MUTATION/ VARIANT ANALYSIS section. NAME OF PROBAND: ASYMPTOMATIC/POPULATION SCREENING RELATIONSHIP TO PROBAND: OTHER (Specify clinical findings below): BMGL LAB#: A COPY OF ORIGINAL RESULTS ATTACHED IF PROBAND TESTING WAS PERFORMED AT ANOTHER LAB, CALL TO DISCUSS PRIOR TO SENDING SAMPLE. A POSITIVE CONTROL MAY BE REQUIRED IN SOME CASES. REQUIRED: NEW YORK STATE PHYSICIAN SIGNATURE OF CONSENT I certify that the patient specified above and/or their legal guardian has been informed of the benefits, risks, and limitations of the laboratory test(s) requested. -

Mut , Mut , Cbla, Cblb
0031-3998/07/6202-0225 PEDIATRIC RESEARCH Vol. 62, No. 2, 2007 Copyright © 2007 International Pediatric Research Foundation, Inc. Printed in U.S.A. Long-Term Outcome in Methylmalonic Acidurias Is Influenced (by the Underlying Defect (mut0, mut؊, cblA, cblB FRIEDERIKE HO¨ RSTER, MATTHIAS R. BAUMGARTNER, CAROLINE VIARDOT, TERTTU SUORMALA, PETER BURGARD, BRIAN FOWLER, GEORG F. HOFFMANN, SVEN F. GARBADE, STEFAN KO¨ LKER, AND E. REGULA BAUMGARTNER Department of General Pediatrics [F.H., P.B., G.F.H., S.F.G., S.K.], Division of Inborn Metabolic Diseases, University Children’s Hospital, D-69120 Heidelberg, Germany; Metabolic Unit [C.V., T.S., B.F. E.R.B.], University Children’s Hospital Basel, CH-4005 Basel, Switzerland; Division of Metabolism and Molecular Pediatrics [M.R.B.], University Children’s Hospital Zu¨rich, CH-8032 Zu¨rich, Switzerland ABSTRACT: Isolated methylmalonic acidurias comprise a hetero- mut0 defect with complete loss of MCM activity (1). Both geneous group of inborn errors of metabolism caused by defects of defects are caused by mutations in the MUT gene and there- 0 – methylmalonyl-CoA mutase (MCM) (mut , mut ) or deficient syn- fore belong to the same complementation group (MIM thesis of its cofactor 5=-deoxyadenosylcobalamin (AdoCbl) (cblA, #251000). Using somatic complementation analysis, defects cblB). The aim of this study was to compare the long-term outcome of AdoCbl synthesis can be subdivided into several groups, in patients from these four enzymatic subgroups. Eighty-three pa- tients with isolated methylmalonic acidurias (age 7–33 y) born three of which cause isolated methylmalonic acidurias, i.e. between 1971 and 1997 were enzymatically characterized and pro- cblA, cblB, and, less frequently, cblD defects (2). -

New Tests 2 Test Updates 4 CPT Code Updates 11 Deleted Tests 11 Diagnostics Update Volume XXI, No
Volume XXI, No. 6 JUNE 2021 MONTHLY TEST UPDATES Diagnostics Update New Tests 2 Test Updates 4 CPT Code Updates 11 Deleted Tests 11 Diagnostics Update Volume XXI, No. 6 | JUNE 2021 New Tests Use Anti-DFS70 antibodies may help identify individuals who do not have an Anti-Carbamylated Protein (CarP) Antibody 520311 ANA-associated Autoimmune Rheumatic Disease (AARD) especially in the absence of significant clinical findings.1 Anti-DFS70 Ab, especially when positive CPT 83516 in isolation (i.e. in the absence of AARD-associated autoantibodies), may Synonyms Anti-CarP antigen antibody; RA marker prevent unnecessary referrals and examinations of ANA-positive individuals.2 Special Instructions This test has not been approved for NY state clients. Limitations This test should be used with clinical findings and other Specimen Serum autoimmune testing; it cannot be used alone to rule out autoimmune disease. Volume 1 mL This test was developed and its performance characteristics determined Minimum Volume 0.5 mL by Labcorp. It has not been cleared or approved by the Food and Drug Container Red-top tube; serum from red-top tube; serum from a gel tube; or Administration. serum gel tube Methodology Enzyme-linked immunosorbent assay (ELISA) Collection Separate serum from cells within one hour of collection. Transfer to a Additional Information Anti-DFS70 antibodies target the dense fine speckled plastic transport tube before shipping. protein of 70 kDa which is identical to Lens Epithelium-Derived Growth Factor Storage Instructions Refrigerate or freeze. or transcription co-activator p75 (LEDGFp75). They are detectable in 2% to 22% Stability of healthy individuals and in less than 1% of patients with AARD are of unknown Temperature Period clinical significance.