Intracranial Cerebrovascular Evaluations: Transcranial Doppler
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Introduction to Neuroimaging
Introduction to Neuroimaging Aaron S. Field, MD, PhD Assistant Professor of Radiology Neuroradiology Section University of Wisconsin–Madison Updated 7/17/07 Neuroimaging Modalities Radiography (X-Ray) Magnetic Resonance (MR) Fluoroscopy (guided procedures) • MR Angiography/Venography (MRA/MRV) • Angiography • Diffusion and Diffusion Tensor • Diagnostic MR • Interventional • Perfusion MR • Myelography • MR Spectroscopy (MRS) Ultrasound (US) • Functional MR (fMRI) • Gray-Scale Nuclear Medicine ―Duplex‖ • Color Doppler • Single Photon Emission Computed Tomography (SPECT) Computed Tomography (CT) • Positron Emission Tomography • CT Angiography (CTA) (PET) • Perfusion CT • CT Myelography Radiography (X-Ray) Radiography (X-Ray) Primarily used for spine: • Trauma • Degenerative Dz • Post-op Fluoroscopy (Real-Time X-Ray) Fluoro-guided procedures: • Angiography • Myelography Fluoroscopy (Real-Time X-Ray) Fluoroscopy (Real-Time X-Ray) Digital Subtraction Angiography Fluoroscopy (Real-Time X-Ray) Digital Subtraction Angiography Digital Subtraction Angiography Indications: • Aneurysms, vascular malformations and fistulae • Vessel stenosis, thrombosis, dissection, pseudoaneurysm • Stenting, embolization, thrombolysis (mechanical and pharmacologic) Advantages: • Ability to intervene • Time-resolved blood flow dynamics (arterial, capillary, venous phases) • High spatial and temporal resolution Disadvantages: • Invasive, risk of vascular injury and stroke • Iodinated contrast and ionizing radiation Fluoroscopy (Real-Time X-Ray) Myelography Lumbar or -

Neurological Critical Care: the Evolution of Cerebrovascular Critical Care Cherylee W
50TH ANNIVERSARY ARTICLE Neurological Critical Care: The Evolution of Cerebrovascular Critical Care Cherylee W. J. Chang, MD, FCCM, KEY WORDS: acute ischemic stroke; cerebrovascular disease; critical FACP, FNCS1 care medicine; history; intracerebral hemorrhage; neurocritical care; Jose Javier Provencio, MD, FCCM, subarachnoid hemorrhage FNCS2 Shreyansh Shah, MD1 n 1970, when 29 physicians first met in Los Angeles, California, to found the Society of Critical Care Medicine (SCCM), there was little to offer for the acute management of a patient suffering from an acute cerebrovascular Icondition except supportive care. Stroke patients were not often found in the ICU. Poliomyelitis, and its associated neuromuscular respiratory failure, cre- ated a natural intersection of neurology with critical care; such was not the case for stroke patients. Early textbooks describe that the primary decision in the emergency department was to ascertain whether a patient could swallow. If so, the patient was discharged with the advice that nothing could be done for the stroke. If unable to swallow, a nasogastric tube was inserted and then the patient was discharged with the same advice. In the 50 intervening years, many advances in stroke care have been made. Now, acute cerebrovascular patients are not infrequent admissions to an ICU for neurologic monitoring, observa- tion, and aggressive therapy (Fig. 1). HISTORY Over 50 years ago, stroke, previously called “apoplexy” which means “struck down with violence” or “to strike suddenly,” was a clinical diagnosis that was confirmed by autopsy as a disease of the CNS of vascular origin (1). In the 1960s, approximately 25% of stroke patients died within 24 hours and nearly half died within 2 to 3 weeks. -

2Nd Quarter 2001 Medicare Part a Bulletin
In This Issue... From the Intermediary Medical Director Medical Review Progressive Corrective Action ......................................................................... 3 General Information Medical Review Process Revision to Medical Record Requests ................................................ 5 General Coverage New CLIA Waived Tests ............................................................................................................. 8 Outpatient Hospital Services Correction to the Outpatient Services Fee Schedule ................................................................. 9 Skilled Nursing Facility Services Fee Schedule and Consolidated Billing for Skilled Nursing Facility (SNF) Services ............. 12 Fraud and Abuse Justice Recovers Record $1.5 Billion in Fraud Payments - Highest Ever for One Year Period ........................................................................................... 20 Bulletin Medical Policies Use of the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Codes on Contractors’ Web Sites ................................................................................. 21 Outpatient Prospective Payment System January 2001 Update: Coding Information for Hospital Outpatient Prospective Payment System (OPPS) ......................................................................................................................... 93 he Medicare A Bulletin Providers Will Be Asked to Register Tshould be shared with all to Receive Medicare Bulletins and health care -

June-July 2000 Part a Bulletin
In This Issue... Disclosure of Itemized Statement Providers Must Furnish an Itemmized Statement when Requested in Writing by the Beneficiary .................................................................................................... 6 Prospective Payment System The Outpatient Code Editor Software Has Been Modified in Preparation for the Implementation of Outpatient Prospective Payment System ........................... 8 Reclassification of Certain Urban Hospitals Certain Urban Hospitals in the State of Florida May Be Permitted to Be Reclassified as Rural Hospitals................................................................................ 13 ulletin Final Medical Review Policies 33216, 53850, 70541, 82108, 83735, 87621, 93303, 94010, 95004, A0320, J0207, J2430, J2792, J3240, J7190, and J9999 .......................................... 15 B Payment of Skilled Nursing Facility Claims Involving a Terminating Medicare+Choice Plan Payment of Skilled Nursing Facility Care for Beneficiaries Involuntarily Disenrolling from M+C plans Who Have Not Met the 3-Day Stay Requirement ........................................................................................... 67 Features From the Medical Director 3 Administrative 4 lease share the Medicare A roviders PBulletin with appropriate General Information 5 members of your organization. Outpatient Prospective Payment System 7 Routing Suggestions: General Coverage 12 o Medicare Manager Hospital Services 13 o Reimbursement Director Local and Focused Medical Policies 15 o Chief Financial -
Brain Spect with Tl-201 Ddc
BRAIN SPECT WITH TL-201 DDC INIS-mf —11361 BRAIN SPECT WITH TL-201 DDC BRAIN SPECT WITH TL-201 DDC ACADEMISCH PROEFSCHRIFT ter verkrijging van de graad van doctor aan de Universiteit van Amsterdam, op gezag van de Rector Magnificus Prof, dr S.K. Thoden van Velzen, in het openbaar te verdedigen in de Aula der Universiteit (Oude Lutherse Kerk, ingang Singel 411, hoek Spui), op donderdag 21 april 1988 te 13.30 uur door Johan Frederik de Brume geboren te 's Gravenhage AMSTERDAM 1988 Promotor : Prof, dr J.B. van der Schoot Copromotor : Dr E.A. van Royen To my parents Joey, Joost and Duco The publication of this thesis was financially supported by: The Netherlands Heart Foundation CIL, BV, Mallinckrodt General Electric Medical Systems Printed in the Netherlands Rodopi B.V., Amsterdam ISBN: 90-900-2127-2 Contents Chapter 1: Introduction 1 Chapter 2: Current methods in neuroimaging and cerebral blood flow measurements 5 2.1. Angiography and digital subtraction angiography 5 2.2. Duplex sonography 7 2.3. Technetium-99m pertechnetate brainscintigraphy 8 2.4. Regional cerebral blood flow measurements with Xenon-133 8 2.5. Computed tomography and Xenon-enhanced computed tomography 9 2.6. Nuclear magnetic resonance imaging 13 2.7. Positron emission tomography 15 2.8. Single-photon emission computed tomography 16 2.9. Regional cerebral blood flow imaging and blood- brain barrier 25 2.10. Cerebral blood flow tracers for SPECT 27 2.11. Possible applications of SPECT brain studies 32 Chapter 3: Functional brain imaging with 1-123 amphetamine First experience in the Netherlands 53 Chapter 4: Thallium-201 diethyldithiocarbamate 69 4.1. -

Cranial Or Head Ultrasound
Cranial Ultrasound/Head Ultrasound Ultrasound imaging of the head uses sound waves to produce pictures of the brain and cerebrospinal fluid. It is most commonly performed on infants, whose skulls have not completely formed. A transcranial Doppler ultrasound evaluates blood flow in the brain's major arteries. Ultrasound is safe, noninvasive, and does not use ionizing radiation. This procedure requires little to no special preparation. Your doctor will instruct you on how to prepare, including whether adults undergoing the exam should refrain from using nicotine-based products that may cause blood vessels to constrict. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. What is cranial ultrasound? Head and transcranial Doppler are two types of cranial ultrasound exams used to evaluate brain tissue and the flow of blood to the brain, respectively. Head Ultrasound A head ultrasound examination produces images of the brain and the cerebrospinal fluid that flows and is contained within its ventricles, the fluid filled cavities located in the deep portion of the brain. Since ultrasound waves do not pass through bone easily, this exam is most commonly performed on infants, whose skulls have not completely formed. The gaps between those skull bones provide a "window," allowing the ultrasound beam to freely pass into and back from the brain. The ultrasound probe and some gel are placed on the outside of the head in one of those regions without bone. Transcranial Doppler A transcranial Doppler (TCD) ultrasound evaluates both the direction and velocity of the blood flow in the major cerebral arteries of the brain. -

TCD CPT and ICD 10 Codes
TCD CPT Codes /ICD-10 Codes 2021 CPT Codes / ICD-10 Codes CPT codes covered if selection criteria are met: 93886 Transcranial Doppler study of the intracranial arteries; complete study 93888 limited study 93890 vasoreactivity study 93892 emboli detection without intravenous microbubble injection 93893 emboli detection with intravenous microbubble injection Other CPT codes related to the CPB: 61635 Transcatheter placement of intravascular stent(s), intracranial (eg, atherosclerotic stenosis), including balloon angioplasty, if performed REIMBURSEMENT INFORMATION: A complete transcranial Doppler evaluation includes ultrasound examination of the right and left anterior circulation and the posterior circulation, including the vertebral arteries and basilar artery. A limited transcranial Doppler evaluation includes two or less of the below mentioned areas. Excludes hand-held Dopplers that do not provide a hard copy or vascular flow bidirectional analysis. Includes complete transcranial Doppler (TCD) study. Includes patient care required to perform/supervise studies and interpret results. Includes ultrasound evaluation of right/left anterior circulation territories and posterior circulation territory. DWL USA, Inc. 30320 Rancho Viejo Road, Suite 105 San Juan Capistrano, CA 92675 www.dwl.us TCD CPT Codes /ICD-10 Codes 2021 ICD-10 Diagnosis Codes That Support Medical Necessity: D57.00 – D57.02 Hb-SS disease with crisis D57.1 Sickle-cell disease without crisis D57.20 Sickle-cell/Hb-C disease without crisis D57.211 – D57.219 Sickle-cell/Hb-C disease -

A Comparison of Transcranial Doppler and Magnetic Resonance Imaging
Clinical Neurology and Neurosurgery 182 (2019) 37–42 Contents lists available at ScienceDirect Clinical Neurology and Neurosurgery journal homepage: www.elsevier.com/locate/clineuro A comparison of transcranial Doppler and magnetic resonance imaging for T long term changes in middle cerebral artery stenosis ⁎ Chan-Hyuk Leea, Dallah Yoob,c, Hyung-Min Kwonb, Yong-Seok Leeb, a Department of Neurology, Chonbuk National University Hospital, Jeonju, South Korea b Department of Neurology, Seoul Metropolitan Government–Seoul National University Boramae Medical Center, Seoul, South Korea c Department of Neurology Seoul National University Hospital, Seoul, South Korea ARTICLE INFO ABSTRACT Keywords: Objectives: Intracranial arterial stenosis may progress or regress, of which the diagnosis is important to predict Transcranial Doppler the risk of stroke or to evaluate the response of treatment. Transcranial Doppler (TCD) seems to be useful for this Middle cerebral artery purpose, however, optimal diagnostic criteria have not been validated yet. Our study was designed to compare Blood flow velocity TCD changes with magnetic resonance angiography (MRA) to validate optimal TCD criteria for progression or Arterial stenosis regression of middle cerebral artery (MCA). Magnetic resonance imaging Patients and methods: We prospectively enrolled patients who visited our neurology department due to MCA Progression stenosis on TCD examination. Brain MRA was used to identify patients with stenosis of the same site of MCA. Progression or regression was defined by change of MRA grading (normal, mild, moderate, severe or occlusion). Various criteria of mean flow velocity (MFV) difference and percent change were assessed. To register more patients for reliable analysis, additional patients with the same inclusion criteria were recruited retrospectively. -

GUIDELINE for DIAGNOSIS and MANAGEMENT of POST DURAL PUNCTURE HEADACHE in OBSTETRICS Background Symptoms of PDPH
GUIDELINE FOR DIAGNOSIS AND MANAGEMENT OF POST DURAL PUNCTURE HEADACHE IN OBSTETRICS Background CSF acts as a cushion supporting and protecting the brain. Leakage of CSF from the subarachnoid space through a dural breach, can lead to loss of this support. The resulting traction on the innervated tissues around the brain can be responsible for the headache that follows.This headache, called post-dural puncture (PDPH), or low-pressure headache (LPH), is postural and usually self limiting, appearing on the first or second day after dural puncture and lasting less than seven days. However, in cases where the headache is severe enough that the mother is unable to cope with her normal daily tasks and look after her newborn baby, conservative management becomes unsustainable. Epidural blood patch (EBP), if not contraindicated, is the treatment of choice in these cases, especially if symptoms suggestive of cranial nerve involvement are present. The incidence and severity of headache is directly related to the size and the design of the needle used. The majority of parturients suffering inadvertent dural puncture with a Tuohy needle will develop a PDPH, severe enough to require EBP, while the introduction of small-gauge needles with pencil points has greatly reduced the incidence of headaches after spinal anaesthesia. Although the headache is self limiting, the possibility, however remote, of a serious complication such as a subdural haematoma to occur if the hole in the dura is not sealed, has to be kept in mind. Symptoms of PDPH PDPH is classically fronto-occipital and is often associated with neck stiffness. -

Neurosonology: Transcranial Doppler
1 Neurosonology: Transcranial Doppler Mark N. Rubin, M.D. Vascular & Hospital Neurology, Neurosonology Assistant Professor of Neurology Email: [email protected] Google Scholar _______________________________ Northwest Neurology https://www.northwestneuro.com/ 2 Contents Transcranial Doppler (TCD) Services and Indications ........................................................................ 3 What is TCD? ............................................................................................................................... 3 What can be accomplished with TCD? .......................................................................................... 3 When is TCD useful? .................................................................................................................... 3 Overview of TCD Ultrasonography ................................................................................................... 4 General Principles of TCD ............................................................................................................. 4 TCD Technique ............................................................................................................................. 7 Patient Safety .............................................................................................................................. 7 Evidence Compendium by Indication ............................................................................................... 8 Cerebrovascular Disease ............................................................................................................. -

Transcranial Doppler Screening
Oxford Children’s Hospital Transcranial Doppler Screening Information for parents and carers As part of the care provided for your child at the Sickle Cell and Thalassaemia Clinic, we offer transcranial Doppler scans as a regular screening test. This scan provides unique information about the flow of blood in the arteries supplying blood to the brain. page 2 What is a Transcranial Doppler scan (TCD)? A transcranial Doppler machine uses an ultrasound probe to detect the rate (speed) of blood flow in vessels. The probe is rolled over the skin of the head and neck and creates an image of blood vessels (arteries) on a screen. It allows the speed of blood flow to the brain to be measured. Why should children with sickle cell disorders have the scan? In some children, an abnormally fast blood flow in the arteries of the brain may mean that they are narrowed. This may reduce the blood flow to part of the brain. If the blood flow is very reduced, it may increase the risk of your child having a stroke in the future. Research has shown that by carrying out this scan, we can find those children with this problem before a stroke develops. Will it hurt? No, it is painless. The ultrasound probe is just gently rolled over the head and neck. We will use ultrasound jelly to help the probe to slide over your child’s skin and hair, to improve the images on the screen. Who should have the scan? All children between the ages of 2 and 16 who have sickle cell anaemia or sickle beta thalassaemia will be offered a scan. -
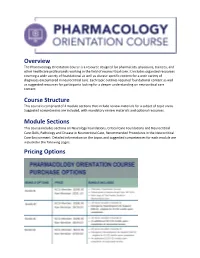
Overview Course Structure Module Sections Pricing Options
Overview The Pharmacology Orientation Course is a resource designed for pharmacists, physicians, trainees, and other healthcare professionals working in the field of neurocritical care. It includes organized resources covering a wide variety of foundational as well as disease-specific content for a wide variety of diagnoses encountered in neurocritical care. Each topic outlines required foundational content as well as suggested resources for participants looking for a deeper understanding on neurocritical care content. Course Structure This course is comprised of 4 module sections that include review materials for a subset of topic areas. Suggested competencies are included, with mandatory review materials and optional resources. Module Sections This course includes sections on Neurology Foundations, Critical Care Foundations and Neurocritical Care Skills, Pathology and Disease in Neurocritical Care, Recommended Procedures in the Neurocritical Care Environment. Detailed information on the topics and suggested competencies for each module are included in the following pages. Pricing Options Module 1: Neurology Foundations Topics: • Neuroanatomy • Neuroradiology (CT/MRI/TCD Interpretation) • ICU Neuro Exam and Localization Suggested Competencies Describe the anatomy of the brain and spinal cord, identifying major external and internal structures, coverings, and fluid-filled spaces. Describe the anatomy of the brainstem, demonstrating knowledge of specific functions. Identify and describe the function of the cranial nerves. Illustrate