Spot Reduction”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Myths & Misconceptions
Lesson Myths & Misconceptions By Carone Fitness Myths & Misconceptions Common Myths This section will provide you with examples of common myths, how to recognize a fad, and aids that you can use to dispel misconceptions. 1 Myths & Misconceptions Fat into Muscle Myth: Exercising turns fat into muscle. Fact: Exercising causes you to lose fat and gain muscle, but fat cells never become muscle cells. Myths & Misconceptions Weight Loss Myth: If you have increased your physical activity level and reduced your caloric intake by 500 calories, but you are not losing a pound a week, you are doing something wrong. Fact: When you begin an exercise program, you may not lose 1 pound every week. 2 Myths & Misconceptions Pounds Myth: One pound of muscle weighs more than one pound of fat. Fact: A pound is a pound. For example, one ton of bricks weighs the same as one ton of feathers. The difference is that a pound of fat has a greater surface area, so it looks bigger than a pound of muscle. Myths & Misconceptions Spot Reduction Myth: If you want to lose fat off your abdominals, you need to do a lot of sit-ups. Fact: This myth is known as spot reduction, which is the belief that you lose fat mass in a specific body part by concentrating exercise in that area. 3 Myths & Misconceptions Spot Reduction Spot reduction does not work because the body gains and loses fat in a genetically predetermined way. Cardiovascular exercise will help you lose body fat generally, and strength training will help a certain area look and feel more toned. -
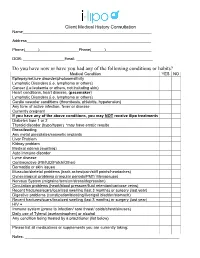
Do You Have Now Or Have You Had Any of the Following Conditions Or Habits?
Client Medical History Consultation Name___________________________________________________________ Address_________________________________________________________ Phone(______)__________________Phone(______)_____________________ DOB: ___________________Email: ___________________________________ Do you have now or have you had any of the following conditions or habits? Medical Condition YES NO Epilepsy/seizure disorder/photosensitivity Lymphatic Disorders (i.e. lymphoma or others) Cancer (i.e.leukemia or others, not including skin) Heart conditions, heart disease, (pacemaker) Lymphatic Disorders (i.e. lymphoma or others) Cardio vascular conditions (thrombosis, phlebitis, hypotension) Any form of active infection, fever or disease Currently pregnant If you have any of the above conditions, you may NOT receive ilipo treatments Diabetes type 1 or 2 Thyroid disorder (hypo/hyper) *may have erratic results Breastfeeding Any metal pins/plates/cosmetic implants Liver Problem Kidney problem Medical edema (swelling) Auto immune disorder Lyme disease Contraceptive (Pill/IUD/Patch/Other) Dermatitis or skin issues Muscular/skeletal problems (back aches/pain/stiff points/headaches) Gynecological problems (irregular periods/PMT/ Menopause) Nervous System (migraine/tension/stress/depression) Circulation problems (heart/blood pressure/fluid retention/varicose veins) Recent fractures/scars/localized swelling (last 3 months) or surgery (last year) Digestive problems (constipation/bloating/liver/gall bladder/stomach) Recent fractures/scars/localized swelling -

Ning, High-Intensity Interval Circuit Training and Steady-State Run- Ning on Body Composition and Glucose Tolerance in Recrea- Tionally Active Adults
COMPARISON OF THE EFFECTS OF HIGH-INTENSITY INTERVAL RUNNING, HIGH-INTENSITY INTERVAL CIRCUIT TRAINING AND STEADY-STATE RUN- NING ON BODY COMPOSITION AND GLUCOSE TOLERANCE IN RECREA- TIONALLY ACTIVE ADULTS Aino Kari Master’s Thesis Exercise Physiology Spring 2015 Department of Biology of Physical Activity University of Jyväskylä ABSTRACT Aino, Kari (2015). Comparison of the effects of high-intensity interval running, high-intensity interval circuit training and steady-state running on body composition and glucose tolerance in recreationally active adults. Department of Biology of Physical Activity, University of Jyväskylä. Master’s thesis. 69 p.. 3 appendixes. Introduction. The measurement of body composition is important for several reasons, but nowadays when obe- sity and overweight are common problems all over the world even more attention should be given to body com- position. Excess amount of fat is itself a risk for health, but it also predisposes to many diseases, one of which is diabetes. It has been shown that with regular physical activity and exercise the body composition and body’s glucose regulation can be improved. In common activity guidelines the amount of traditional endurance and resistance training takes hours per week to perform to fill the recommendations. However, since it has been shown that one of the most common reasons for not participating in exercise is lack of time, therefore high- intensity interval training (HIIT) might be one option. HIIT takes less time to perform, since it consists of short, high-intensity work periods separated often by even shorter, lower intensity recovery periods. Altogether one HIIT session takes in average 30 minutes. -

How to Lose Body Fat?
TRAINER TIPS | IS SPOT REDUCTION A THING? WILL DOING CRUNCHES GIVE ME SIX PACK ABS? SPOT REDUCTION DOESN’T WORK FAT DISTRIBUTION VARIES AMONG INDIVIDUALS The human body does not pull fat from specific areas of the body ANDROID | APPLE-SHAPED BODY GYNOID | PEAR-SHAPED BODY when exercising musculature of that specific area. For example, doing 1,000 crunches won’t shrink your stomach. HOW TO LOSE BODY FAT? CREATE A CALORIC DEFICIT THROUGH COMBINATION OF: Resistance training using compound Diet Cardiovascular exercise exercises (such as squats rather than leg extensions) FITNESS GOAL: TRAINER NAME: PHONE: www.NSCA.com EMAIL: TRAINER TIPS | IS SPOT REDUCTION A THING? WHAT IS SPOT REDUCTION? appears beneficial to emphasize total body, compound exercises (e.g., ontrary to popular belief, the human body does not pull fat from squats) over isolated exercises (e.g., leg extension) for clients seeking specific areas of the body when exercising the musculature of to improve their body composition. Cthat specific area. Marketing and misinformation about “spot reduction” can be misleading. Clients looking for fat loss should The health-related benefits associated with aerobic exercise include focus on compound movements that involve high levels of muscle enhanced insulin sensitivity, reduced body fat, increased bone recruitment, which increases energy expenditure to a greater extent. mineral density, as well as improved cardiovascular and respiratory function (McCarthy, et al., 2012). Moderate-intensity steady state DISPELLING THE MYTH aerobic exercise utilizes a greater percentage of fat oxidation to fuel While exercises that target specific areas of the body (such as performance compared to high-intensity interval training (HIIT). -

Electrical Muscle Stimulation 1 Electrical Muscle Stimulation
Electrical muscle stimulation 1 Electrical muscle stimulation Electrical muscle stimulation (EMS), also known as neuromuscular electrical stimulation (NMES) or electromyostimulation, is the elicitation of muscle contraction using electric impulses. The impulses are generated by a device and delivered through electrodes on the skin in direct proximity to the muscles to be stimulated. The impulses mimic the action potential coming from the central nervous system, causing the muscles to contract. The electrodes are generally pads that adhere to the skin. EMS is both a form of electrotherapy and of muscle training. It is cited by important authors[1] as complementary technique for sport training, and there is published research[2] on the results obtained. In the United States, EMS devices are regulated by the U.S. Food and Drug Administration (FDA).[3] History Luigi Galvani (1791) provided the first scientific evidence that current can activate muscle. During the 19th and 20th century researchers studied and documented the exact electrical properties that generate muscle movement.[4] [5] It was discovered that the body functions induced by electrical stimulation caused long-term changes in the muscles.[6] [7] In the '60s Soviet sport scientists applied EMS in the training of elite athletes, claiming 40% force gains.[8] In the '70s these studies were shared during conferences with the Western sport establishments. However, results were conflicting, perhaps because the mechanisms in which EMS acted was poorly understood.[9] Recent medical physiology research[10] [11] [12] pinpointed the mechanisms by which electrical stimulation causes adaptation of cells of muscles, blood vessels[13] [14] [15] and nerves. -

Contour Light Body Makeover 3 Weeks to a New You! Lose Fat at the Speed of Light!
Contour Light Body Makeover 3 Weeks To A New You! Lose Fat At The Speed Of Light! Safe Treatments For Fat Removal! Results Seen Same Day No Pain, No Surgery, No Downtime Contour Light! Background • The 635nm red light technology was originally developed as an adjunct treatment to liposuction • The technology has been used safely in the medical community for over 4o years. • Based on sound scientific and physiologic principles • Clinical trials have proven effectiveness and safety Why Am I Just Hearing About This? Previously in the U.S. body sculpting has been used by the rich and famous due to the cost. Many movie stars use similar programs to get back into shape after having a baby. How do you think they lost the baby weight so fast? Today it is affordable and available to you! What Is Contour Light? • Contour Light is a 635 nm Red Light Therapy • Contour Light has 4 extra large pads that are 28”x 12” which are applied directly to the skin for 25 minutes • Each Pad has 320 diodes. Each diode emits 40 mW of light energy for a total of 51,200 mW of power, making it the most powerful device on the market! • Covers more area of the body than any other device on the market! Making it the easiest to use! • The wavelength opens the fat cells allowing the fat to exit the cell • The results? Incredible spot reduction on the arms, neck, back, breasts, saddlebags, inner thighs, knees- virtually anywhere you have excess fat • No pain, no bruising, no swelling, no burning, no downtime… NO side effects! Contour Light delivers the most power and covers -

Effects of HIIT on Fat Loss
International Journal of Obesity (2008) 32, 684–691 & 2008 Nature Publishing Group All rights reserved 0307-0565/08 $30.00 www.nature.com/ijo ORIGINAL ARTICLE The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women EG Trapp1, DJ Chisholm2, J Freund1 and SH Boutcher1 1Faculty of Medicine, University of New South Wales, Sydney, New South Wales, Australia and 2Garvan Institute, Sydney, New South Wales, Australia Objective: To determine the effects of a 15-week high-intensity intermittent exercise (HIIE) program on subcutaneous and trunk fat and insulin resistance of young women. Design and procedures: Subjects were randomly assigned to one of the three groups: HIIE (n ¼ 15), steady-state exercise (SSE; n ¼ 15) or control (CONT; n ¼ 15). HIIE and SSE groups underwent a 15-week exercise intervention. Subjects: Forty-five women with a mean BMI of 23.2±2.0 kg mÀ2 and age of 20.2±2.0 years. Results: Both exercise groups demonstrated a significant improvement (Po0.05) in cardiovascular fitness. However, only the HIIE group had a significant reduction in total body mass (TBM), fat mass (FM), trunk fat and fasting plasma insulin levels. There was significant fat loss (Po0.05) in legs compared to arms in the HIIE group only. Lean compared to overweight women lost less fat after HIIE. Decreases in leptin concentrations were negatively correlated with increases in VO2peak (r ¼À0.57, Po0.05) and positively correlated with decreases in TBM (r ¼ 0.47; Po0.0001). There was no significant change in adiponectin levels after training. -

Cryolipolysis for Fat Reduction and Bod...Fficacy of Current Treatment Paradigms
10/12/2017 Cryolipolysis for Fat Reduction and Body Contouring: Safety and Efficacy of Current Treatment Paradigms PLASTIC AND RECONSTRUCTIVE SURGERY Plast Reconstr Surg. 2015 Jun; 135(6): 1581–1590. PMCID: PMC4444424 Published online 2015 May 28. doi: 10.1097/PRS.0000000000001236 Cryolipolysis for Fat Reduction and Body Contouring: Safety and Efficacy of Current Treatment Paradigms Michael J. Ingargiola, M.D., Saba Motakef, M.D., Michael T. Chung, M.D., Henry C. Vasconez, M.D., and Gordon H. Sasaki, M.D. New York, N.Y.; Loma Linda, Calif.; Durham, N.C.; and Louisville, Ky. From the Division of Plastic and Reconstructive Surgery, Mount Sinai Hospital; Department of Plastic Surgery, Loma Linda University; Division of Plastic, Maxillofacial, and Oral Surgery, Duke University; and the Division of Plastic Surgery, University of Kentucky. Corresponding author. Gordon H. Sasaki, M.D., Department of Plastic Surgery, Loma Linda University, 11175 Campus Street, CP 21126, Loma Linda, Calif. 92354, [email protected] Received 2014 Jul 3; Accepted 2014 Dec 12. Copyright © 2015 by the American Society of Plastic Surgeons This is an openaccess article distributed under the terms of the Creative Commons AttributionNonCommercialNoDerivatives 3.0 License, where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially. This article has been cited by other articles in PMC. Abstract Go to: Background: Cryolipolysis is a nonsurgical technique for localized fat reduction. With the increased risk of complications from more invasive methods such as liposuction, cryolipolysis presents a promising method for nonsurgical body contouring. -

Weight Training Introduction 1) You Have 206 Bones in the Adult Human
Weight Training Introduction 1) You have 206 bones in the adult human body. 2) There are approximately 600 muscles in the body that make up 50% of your body weight 3) 40% are voluntary (skeletal), 10% Involuntary (cardiac, smooth(digestive)) 4) Physical benefits of weight training include: Muscle strength, balance, posture, injury prevention, increase bone density, increase muscle endurance, increased metabolism. Emotional/mental benefits: release tension, release anger, alleviates depression, increases self-esteem, teaches discipline 5) Possible grips used: overhand (pronate); underhand (supinate); combo 6) Set realistic goals, know what you want to achieve through your lifting program 7) Machines vs. Free weights - *Machines: safe without spotter, provide variable resistance throughout (the resistance varies so that the intensity remains the same), easy to adjust weight, encourages proper form *Free weights: learn proper form, using stabilizing muscles, more free range of motion, some machines don’t adjust to fit your body, more variety of exercises, more technically difficult Key Points 1) You should lift no less than 2 days a week, preferably at least 3, work all major muscle groups all days 2) OR 4-6 workout days a week, varying muscle groups to give 48 hours rest to each group between workouts 3) As a beginner lifter: Week 1 and 2 – 1 set of 20 reps per muscle group Week 3 and 4 – 2 sets of 20 reps per group Week 5 and 6 – will start to vary based on long-term goals 4) Lift the largest muscle groups first; also the most technically difficult exercises first. 5) Lift opposing muscles for muscle balance and to help prevent injury 6) Use full range of motion during a lift, stretching (static), warm-up (cardio or light weight) – for full flexibility retention 7) Exhale on exertion (hardest phase of lift) 8) Proper form is: relaxed knees and shoulders, abdominals contracted isometrically, standing – feet hip width apart 9) Never hyperextend (lockout) or hyperflex any joint Extension – opening of a joint (i.e. -

Regional Fat Changes Induced by Localized Muscle Endurance Resistance Training
REGIONAL FAT CHANGES INDUCED BY LOCALIZED MUSCLE ENDURANCE RESISTANCE TRAINING RODRIGO RAMI´REZ-CAMPILLO,1 DAVID C. ANDRADE,2 CHRISTIAN CAMPOS-JARA,3 CARLOS HENRI´QUEZ-OLGUI´N,4 CRISTIAN ALVAREZ-LEPI´N,5 AND MIKEL IZQUIERDO6 1Physical Activity Sciences Department, Los Lagos University, Osorno, Chile; 2Celular Physiology Laboratory, Biomedical Department, Faculty of Health Sciences, Antofagasta University, Antofagasta, Chile; 3Kinesiology Department, Los Lagos University, Puerto Montt, Chile; 4Physiology Laboratory, Biological Sciences Department, Biological Sciences Faculty, Andres Bello University, Santiago, Chile; 5Los Lagos Family Health Center, Health Promotion Center for Women, Los Lagos, Chile; and 6Department of Health Sciences, Public University of Navarre, Tudela, Spain ABSTRACT segment. The present results expand the limited knowledge avail- Ramı´rez-Campillo,R,Andrade,DC,Campos-Jara,C,Henrı´quez- able about the plastic heterogeneity of regional body tissues when Olguı´n, C, Alvarez-Lepı´n, C, and Izquierdo, M. Regional fat a localized resistance training program is applied. changes induced by localized muscle endurance resistance train- KEY WORDS spot reduction, DXA, corporal composition, ing. J Strength Cond Res 27(8): 2219–2224, 2013—The purpose exercise of this study was to examine the effects of a localized muscle endurance resistance training program on total body and regional INTRODUCTION tissue composition. Seven men and 4 women (aged 23 6 1years) xercise programs (aerobic or resistance training) were trained with their nondominant leg during 12 weeks, 3 ses- may lead to differential regional adipose tissue depot sions per week. Each session consisted of 1 set of 960–1,200 loss, possibly by differential regional alterations of repetitions (leg press exercise), at 10–30% 1 repetition maximum. -

WHY MANY WOMEN NEVER GET TONED Introduction If You’Re Like Most People, You’Ve Tried Dieting and Learned the Hard Way That It Doesn’T Work
WHY MANY WOMEN NEVER GET TONED Introduction If you’re like most people, you’ve tried dieting and learned the hard way that it doesn’t work. You’ve been working out hard, but despite your best efforts, you haven’t got the results you wanted and your body looks the same. You just haven’t been able to achieve the lean, toned body you want. Well here’s a no-nonsense guide to help you de-bunk many of the myths and misinformation around getting toned, to explain why many women never get toned, and to set you on the right path – so you can look good, feel great and be healthy. .com STARTING with the facts Firstly, there’s no such thing as toning exercises - no particular exercise or combination of sets and reps can directly cause tone. No style or type of training that in itself allows you to tone up a specific area of your body (or your entire body for that matter). There’s no magical method or workout that you can do. And no machines, products or supplements that can make you toned (despite the claims of the multi- billion dollar weight-loss and fitness industry). Secondly, you can’t tone a specific area or muscle because it is not possible to target and burn fat from one specific area of your body (spot reduction). Even though your body tends to deposit fat in certain areas, burning it off doesn’t work the same way. The human body is only capable of losing fat from the entire body as a whole. -

Can Alternating Lower Body Negative and Positive Pressure During Exercise Alter Regional Body Fat Distribution Or Skin Appearance?
Eur J Appl Physiol (2012) 112:1861–1871 DOI 10.1007/s00421-011-2147-1 ORIGINAL ARTICLE Can alternating lower body negative and positive pressure during exercise alter regional body fat distribution or skin appearance? Elisabeth Löberbauer-Purer · Nanna L. Meyer · Susanne Ring-Dimitriou · Judith Haudum · Helmut Kässmann · Erich Müller Received: 21 March 2011 / Accepted: 3 August 2011 / Published online: 16 September 2011 © Springer-Verlag 2011 Abstract The purpose of this study was to determine and fat mass when compared with D, while no signiWcant whether physical activity, with and without lower body diVerence was observed between the other groups. A simi- pressure, leads to increased regional fat loss in the lower lar pattern was seen for circumference measurement data. extremities of overweight females. Eighty-six obese A signiWcant perceived improvement was made by the DEP women with a female phenotype were randomly assigned group when compared with C, D and DE groups for skin into four groups: control group (C), diet only (D), diet plus condition and also between the DEP versus C and D groups exercise (DE) or diet, exercise and lower body pressure for cellulite. The combination of diet and exercise is suc- intervention (DEP). The three treatment groups followed cessful for weight reduction. The additional application of the same diet, the two exercise groups (DE and DEP) addi- lower body pressure especially aVects skin appearance. tionally followed an endurance training program of 30 min of cycling at 50%VO2max three times per week with or Keywords Body fat distribution · Lower body negative without lower body pressure.