Microvascular Changes After Conbercept Therapy in Central Retinal Vein Occlusion Analyzed by Optical Coherence Tomography Angiography
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

China Kepei Education Group Limited 中國科培教育
696795 \ (China Kepei Education) \ 25/04/2019 \ M11 China Kepei Education Group Limited 中國科培教育集團有限公司 (Incorporated in the Cayman Islands with limited liability) (Stock Code: 1890) FORM OF PROXY FOR USE AT ANNUAL GENERAL MEETING I/We (Name) (Block capitals) of (Address) being the holder(s) of (see Note 1) shares of US$0.00001 each in the capital of China Kepei Education Group Limited (the “Company”) hereby appoint (Name) of (Address) or failing him/her (Name) of (Address) or failing him/her, the chairman of the meeting (see Note 2) as my/our proxy to attend and vote for me/us and on my/our behalf at the Annual General Meeting of the Company to be held at Room 109, No. 35 Building, Guangdong Polytechnic College, Qifu Road, Gaoyao District, Zhaoqing City, Guangdong Province, the PRC on 3 June 2019 at 10:30 a.m. and at any adjournment thereof or on any resolution or motion which is properly proposed thereat. My/Our proxy is authorised and instructed to vote as indicated (see Note 3) in respect of the undermentioned resolutions: Ordinary Resolutions (see Note 3) FOR (see Note 3) AGAINST (see Note 3) 1. To receive and adopt the audited consolidated financial statements of the Company for the year ended 31 December 2018 and the reports of the directors and auditor thereon. 2. To declare a final dividend of HK$0.10 per share for the year ended 31 December 2018. 3. (a) To re-elect the following retiring directors of the Company (“Directors”, each a “Director”): (i) Mr. -

A Study on the Differences of Mandarin Mingled By
316 INTERNATIONAL JOURNAL OF SOCIAL SCIENCE, INNOVATION AND EDUCATIONAL TECHNOLOGIES (ONLINE) - ISSN: 2717-7130 Vol:1, Issue: 3 pp: 316-323 JEL Codes: Z1, Z13,Z19 LI J. (2020). “A Study on the Differences of Mandarin Mingled by Cantonese in the Pearl River Delta of China” Vol: 1 Issue: 3 pp: 316-323 Key words: Cantonese; Mandarin mingled by Cantonese; heterogeneous words; Mandarin level; variance analysis. Article Type Research Article A Study on the Differences of Mandarin Mingled by Cantonese in the Pearl River Delta of China Arrived Date Accepted Date Published Date 17.07.2020 24.07.2020 31.07.2020 Jinfeng Li * ABSTRACT The phenomenon of Mandarin Mingled by Cantonese is widespread in Guangdong dialect area. It is mainly reflected in the heterogeneous pronunciation and vocabulary, and its performance degree reflects speakers’ Mandarin level. In the summer of 2019, this paper investigated the Pearl River Delta area and found that: The development of Mandarin level is unbalanced. According to variance analysis and expert scoring, the equilibrium degree can be divided into four gradients from good to bad. The first gradient: Shenzhen; the second gradient: Zhuhai, Guangzhou, Dongguan; the third gradient: Foshan, Huizhou; the fourth gradient: Zhongshan, Jiangmen, Zhaoqing. It’s wise to strengthen the promotion of Mandarin in Guangdong, to promote the balanced development of regional economic integration. INTRODUCTION With the development of science and technology, economy and education, the integration of Mandarin in China has been greatly accelerated, which has intensified the integration of Mandarin and dialects, and fierce competition has been launched between them. According to Thomason and Terrence (1988) and Thomason (2001), when two or more languages come into contact with each other, the interaction and long-term effects of different languages may result in new fused languages with traces of the original language. -

Ceramic Tiles No
รายชื่อโรงงานที่ท าผลิตภณั ฑใ์ นต่างประเทศที่ได้รับการขึ้นทะเบยี น List of Registered Foreign Manufacturer ขอบข่ายตามมาตรฐานเลขที่ มอก.2508-2555 กระเบื้องเซรามิก TIS 2508-2555 : Ceramic tiles No. Manufacture name Address Country Certificate of Date of Date of Expiry Registration No. Registration 1 PRIME DAI LOC JOINT STOCK DAI QYABG UBDYSTRUAK ZIBEM DAU LOC, SOCIALIST R2508-238 25-Oct-2017 24-Oct-2020 COMPANY QUANG NAM REPUBLIC OF VIETNAM 2 FOSHAN CHANCHENG HUALIN QIAOLE ROAD (SIDE OF JILI TRANSFORMER PEOPLE'S REPUBLIC R2508-239 30-Oct-2017 29-Oct-2020 CERAMIC CO., LTD. SUBSTATION), NANZHUANG TOWN CHANCHENG OF CHINA DISTRICT, FOSHAN CITY, GUANGDONG PROVINCE 3 R.A.K. CERAMICS P.J.S.C P.O. BOX 4714, RAS AL KHAIMAH UNITED ARAB R2508-240 7-Nov-2017 6-Nov-2020 EMIRATES 4 PT. KIA SERPIH MAS KOTA INDUSTRI SURYA CIPTA, JL SURYALESTARI REPUBLIC OF R2508-241 16-Nov-2017 15-Nov-2020 KAV1-2 KEC CIAMPEL KARAWANG TIMUR INDONESIA 1/28 รายชื่อโรงงานที่ท าผลิตภณั ฑใ์ นต่างประเทศที่ได้รับการขึ้นทะเบยี น List of Registered Foreign Manufacturer ขอบข่ายตามมาตรฐานเลขที่ มอก.2508-2555 กระเบื้องเซรามิก TIS 2508-2555 : Ceramic tiles No. Manufacture name Address Country Certificate of Date of Date of Expiry Registration No. Registration 5 MOD CERAMIC INDUSTRIES LTD 8-A, NATIONAL HIGHWAY, MORBI-363 642 REPUBLIC OF INDIA R2508-242 23-Nov-2017 22-Nov-2020 GUJARAT 6 PIONEER CERAMIC INDUSTRIES 8A NATIONAL HIGHWAY, OPP, LALPAR VILLAGE REPUBLIC OF INDIA R2508-243 24-Nov-2017 23-Nov-2020 MORBI 363642, GUJARAT 7 HEYUAN ROMANTIC CERAMICS HUANGTULING VILLAGE, DENGTA TOWN, PEOPLE' S R2508-244 14-Dec-2017 13-Dec-2020 CO., LTD. DONGYUAN COUNTY HEYUAN CITY, GUANGDONG REPUBLIC OF CHINA 8 PORCELAINGRES GMBH IRISSTRASSE, 1-03226 VETSCHAU, REPUBLIC OF R2508-245 18-Dec-2017 17-Dec-2020 (BRANDENBURG) FEDERAL GERMANY 2/28 รายชื่อโรงงานที่ท าผลิตภณั ฑใ์ นต่างประเทศที่ได้รับการขึ้นทะเบยี น List of Registered Foreign Manufacturer ขอบข่ายตามมาตรฐานเลขที่ มอก.2508-2555 กระเบื้องเซรามิก TIS 2508-2555 : Ceramic tiles No. -

On the Historical Context and the Inheritance Strategy of the Water Transport City in Guigang
E3S Web of Conferences 143, 01032 (2 020) https://doi.org/10.1051/e3sconf/20 2014301032 ARFEE 2019 On the historical context and the inheritance strategy of the water transport city in Guigang Liyuan Guo1, Liangchu Long2, Yanhua Wan3* and Ruidong Shi4 1 Master of Urban and Rural Planning, College of Civil and Architectural Engineering, Guilin University of Technology, Guilin,China 2 Professor, College of Civil and Architectural Engineering, Guilin University of Technology, Guilin,China 3 Professor, College of Architecture and Urban Planning, Huazhong University of Science and Technology, Wuhan,China 4 Master of Urban and Rural Planning, College of Civil and Architectural Engineering, Guilin University of Technology, Guilin,China Abstract. As the most extensive port in Guangxi's inland economic hinterland, waterway transportation is an important driving force for the development of Guigang's cities. On the basis of tracing the development history of Guigang water transport city, this paper summarizes and analyzes the historical characteristics of water transport development and the spatial evolution of Guigang city, and proposes the planning strategy of Guigang's water transport city historical context, in order to improve the competitiveness of Guigang city and promote the development of Guigang city. Historically, shipping traffic was the main means of 1 Introduction transportation in Guangxi. At that time, the primitive commercial port of Guigang was formed. The South China Guigang is located in the geometric center of Nanning, Sea and Gaoyao District of Guangdong Province are the Beihai, Liuzhou, Wuzhou and other central cities in main places for business. The starting stations are all in Guangxi Autonomous Region. -

International Registration Designating India Trade Marks Journal No: 1841 , 19/03/2018 Class 1
International Registration designating India Trade Marks Journal No: 1841 , 19/03/2018 Class 1 2665685 05/08/2013 [International Registration No. : 1174717] Neogen Corporation 620 Lesher Place Lansing, MI 48912 United States of America United States of America Address for service in India/Agents address: ZEUSIP 9, BIRBAL ROAD, JANGPURA EXTENSION, NEW DELHI-110014 Proposed to be Used IR DIVISION Diagnostic kits comprising biological or chemical reagents for detecting microorganisms or chemicals in various environments. 9346 Trade Marks Journal No: 1841 , 19/03/2018 Class 1 Priority claimed from 20/09/2017; Application No. : 710514 ;Switzerland 3748424 06/12/2017 [International Registration No. : 1386829] Clariant AG Rothausstrasse 61 CH-4132 Muttenz Switzerland Proposed to be Used IR DIVISION Active chemical ingredients and chemical products used in industry. 9347 Trade Marks Journal No: 1841 , 19/03/2018 Class 1 Priority claimed from 26/09/2017; Application No. : 30 2017 109 743 ;Germany 3750659 04/12/2017 [International Registration No. : 1387472] BYK Additives Ltd. Moorfield Road Widnes, Cheshire WA8 0JU United Kingdom Proposed to be Used IR DIVISION Chemical products for industrial purposes; chemical additives; silicates; phyllosilicates used as additives for catalytic activities; phyllosilicates used as absorbents; catalysts. 9348 Trade Marks Journal No: 1841 , 19/03/2018 Class 1 3760088 12/12/2017 [International Registration No. : 1389104] "IBA GmbH" Rudolf-Wissell-Str.28 37079 Göttingen Germany Proposed to be Used IR DIVISION Chemicals used in industry and science, namely fusion proteins and fusion peptides as well as their gene sequences; analysis kits used in science for purification and/or detection and/or immobilisation of fusion proteins and/or fusion peptides, mainly consisting of chemical reagents. -

Research on the Construction of Zhaoqing Urban Ecological Infrastructure Based on Ecological Security - 9159
Zhang: Research on the construction of Zhaoqing urban ecological infrastructure based on ecological security - 9159 - RESEARCH ON THE CONSTRUCTION OF ZHAOQING URBAN ECOLOGICAL INFRASTRUCTURE BASED ON ECOLOGICAL SECURITY ZHANG, H. College of Life Sciences, Zhaoqing University, Guangdong, China (e-mail: [email protected]) (Received 19th Mar 2019; accepted 22nd May 2019) Abstract. In the process of urbanization, the region faces environmental problems such as destruction of ecological corridors, fragmentation of biological habitats, and soil erosion, which pose potential risks to the regional ecological environment. Therefore, it is of great significance to identify lands with ecological conflict, establish core ecological protection zones and ecological corridors, and build an ecological security pattern for regional sustainable development. The research subject of this paper is Zhaoqing area. From the perspective of landscape ecological security pattern, it identifies the green land in Zhaoqing City, hydrological system, local culture, natural ecological protection, and the chance of geological disasters, and combines RS (Remote Sensing) and GIS (Geographic Information System) technology to evaluate green land and identify environmental core protection. Urban ecological infrastructure patterns are built in district, ecological corridors and ecological buffer zones and land with ecological conflict is curbed form expansion. The study found that it is necessary to carry out controlled development of ecological conflict zones such as the Xijiang River Basin, the Beiling Mountain Forest Land, and the Gaoyao Plain to ensure the safety of the fundamental ecological facilities in Zhaoqing. Keywords: core ecological protection zone, ecological assessment, ecological source, ecological buffer zone, control development Introduction At present, China’s rapid economic development promotes urban construction, but it is accompanied by an ecological environmental crisis that threatens the national ecological security. -

Clifford Modern Living Holdings Limited 祈福生活服務
The Stock Exchange of Hong Kong Limited and the Securities and Future Commission take no responsibility for the contents of this PHIP, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this PHIP. Post Hearing Information Pack of CLIFFORD MODERN LIVING HOLDINGS LIMITED 祈福生活服務控股有限公司 (incorporated in the Cayman Islands with limited liability) (the “Company”) (incorporated in the Cayman Islands with limited liability) WARNING The publication of this Post Hearing Information Pack (“PHIP”) is required by The Stock Exchange of Hong Kong Limited (the “Stock Exchange”) and the Securities and Futures Commission (the “SFC”) solely for the purpose of providing information to the public in Hong Kong. This PHIP is in draft form. The information contained in it is incomplete and is subject to change which can be material. By viewing this PHIP, you acknowledge, accept and agree with the Company, its sponsor, advisers or members of the underwriting syndicate that: (a) this document is only for the purpose of providing information about the Company to the public in Hong Kong and not for any other purposes. No investment decision should be based on the information contained in this document; (b) the publication of this document or supplemental, revised or replacement pages on the Stock Exchange’s website does not give rise to any obligation of the Company, its sponsor, advisers or members of the underwriting syndicate to proceed with an offering in Hong Kong or any other jurisdiction. -

(JD 7204) [email protected] Ashly E
Jason M. Drangel (JD 7204) [email protected] Ashly E. Sands (AS 7715) [email protected] Brieanne Scully (BS 3711) [email protected] Danielle Futterman (DY 4228) [email protected] EPSTEIN DRANGEL LLP 60 East 42nd Street, Suite 2520 New York, NY 10165 Telephone: (212) 292-5390 Facsimile: (212) 292-5391 Attorneys for Plaintiff FoxMind Canada Enterprises Ltd. UNITED STATES DISTRICT COURT SOUTHERN DISTRICT OF NEW YORK Civil Case No.: 21-cv-5135 (KPF) FOXMIND CANADA ENTERPRISES LTD., Plaintiff 1) TEMPORARY RESTRAINING ORDER; 2) ORDER v. RESTRAINING MERCHANT STOREFRONTS AND ASDA TECHNOLOGY (ZHAOQING) CO., DEFENDANTS’ ASSETS WITH LTD., CHANGSHA SHANGHAO THE FINANCIAL INSTITUTIONS; TECHNOLOGY CO., LTD., DONGGUAN 3) ORDER TO SHOW CAUSE AVIC INDUSTRY & TRADE CO., LTD., WHY A PRELIMINARY DONGGUAN BAISHUN SILICONE & INJUNCTION SHOULD NOT PLASTIC PRODUCTS CO., LTD., ISSUE; 4) ORDER AUTHORIZING DONGGUAN BLUE OCEAN GIFTS LIMITED, BIFURCATED AND DONGGUAN CHANGQIANG HARDWARE & ALTERNATIVE SERVICE; AND 5) PLASTIC CO., LTD., DONGGUAN CHCC ORDER AUTHORIZING TECH CO., LTD, DONGGUAN CHENLANG EXPEDITED DISCOVERY ELECTRONIC TECHNOLOGY CO., LTD., DONGGUAN CHONGSHANG TECHNOLOGY LTD., DONGGUAN CITY TINGFENG FILED UNDER SEAL SILICONE CO., LTD., DONGGUAN HUAQI SEALING CO., LTD., DONGGUAN HUAQIN ELECTRONIC TECHNOLOGY CO., LTD., DONGGUAN HUAYI GIFT PACKAGING CO., LTD., DONGGUAN IMAITONG ELECTRONICS CO., LTD., DONGGUAN JIAYUE SILICONE RUBBER PRODUCTS CO., LTD., DONGGUAN ORK RUBBER PRODUCTS CO., LTD., DONGGUAN QUNYI TECHNOLOGY CO., LTD., -
参展商名录索引index of Exhibitors
中国广州国际家具生产设备及配料展览会 CHINA INTERNATIONAL FURNITURE MACHINERY & FURNITURE RAW MATERIALS FAIR (GUANGZHOU) interzum guangzhou 参展商名录索引 Index of Exhibitors (按公司英文名称字母排序) (Alphabetical List of Exhibitors) 2018.03.28-31 中国广州国际家具生产设备及配料展览会 CHINA INTERNATIONAL FURNITURE MACHINERY & FURNITURE RAW MATERIALS FAIR (GUANGZHOU) interzum guangzhou 2018.03.28-31 A A&D JASMINE INTERNATIONAL CO., LTD. 佳饰美国际事业有限公司 ................................................................................................................. 14.1E23 .....................................370 A1-OZEMEK PLASTIK PROFIL VE KALIP SAN. TIC. LTD. STI. ...................................................... 14.1G23 ....................................381 Aaron Woodworking Machinery Co., Ltd 广州爱伦木工机械有限公司 ............................................................................................................ 11.1A31 .....................................246 AB & M FURNITURE COMPONENTS CO., LTD. 江门市捷荣实业投资有限公司 ....................................................................................................... S16.2A16 ..................................509 ABC Aluminium Co., Ltd. 佛山南海万象家居材料有限公司 .................................................................................................. 14.1C05 .....................................362 Adler (Far East) Co., Ltd 东莞市爱乐缝制设备有限公司 ....................................................................................................... 12.1D05 .....................................277 ADVANCE HARDWARE 杭州德美五金有限公司 ..................................................................................................................... -

Ss21 Footwear & Accessory Suppliers
SS21 FOOTWEAR & ACCESSORY SUPPLIERS Accessories COUNTRY SUPPLIER GROUP FACTORY NAME ADDRESS China Creaton Handbag Factory WORKERS <500 Tian Tou Jiao FEMALE >50% MALE >25% Management Area Qiao Tou Town OAR ID CN2019085CN0H73 Dongguan City GEOLOCATION Guangdong Province 523526 23.006788 114.034613 China GOLD MEDAL zhejiang laxdi kniting co.,ltd WORKERS <500 north industrial zone FEMALE MALE xiaoshun town jindong area OAR ID CN2019085RSNH23 jinhua city GEOLOCATION zhejiang 29.1826594 119.8505314 China GOLD MEDAL Zhejiang Sunmans Knitting Co., Ltd WORKERS <500 No. 139 Biyun North Rd FEMALE >75% MALE <25% Haining Zhejiang OAR ID CN20190857W3QS0 GEOLOCATION 30.54765065 120.7068713 Page 1 of 40 SS21 FOOTWEAR & ACCESSORY SUPPLIERS Accessories COUNTRY SUPPLIER GROUP FACTORY NAME ADDRESS China GOLD MEDAL Zhejiang Meikan Garment& Accessories Co.,LTD WORKERS <500 No.318Xiachuan Road FEMALE >75% MALE <25% Haining Zhejiang OAR ID CN2019085EX7Q5R GEOLOCATION 30.54275905 120.7132257 China GOLD MEDAL WUXI ZEZHONG KNITTING & TEXTILE CO.,LTD WORKERS <500 No.5 XIAGUANGROAD FEMALE >75% MALE <25% QIAOQI INDUSTRIAL DISTRICT XU-XIAKETOWN OAR ID CN2019085KQ3X5S JIANGYIN GEOLOCATION JIANGSU 31.802932 120.333789 China GOLD MEDAL ZHUJI CITY KAIWEI KNITTING CO., LTD. WORKERS <500 No.6 Biquan Road FEMALE >25% MALE >50% Taozhu Street Zhuji City OAR ID CN2020028W7E0S9 Zhejiang GEOLOCATION Shaoxing 311800 29.7001176 120.1952722 Page 2 of 40 SS21 FOOTWEAR & ACCESSORY SUPPLIERS Accessories COUNTRY SUPPLIER GROUP FACTORY NAME ADDRESS China GOLD MEDAL zhejiang kainiwei knitting cloting co.,ltd WORKERS <500 North industrial zone FEMALE MALE Xiaoshun town Jindong area OAR ID CN2019085RSNH23 Jinhua city GEOLOCATION Zhejiang 29.182661 119.868041 China Leatherlove ZhuHai Xing Fa Handbag Mgf. -

2018 Footwear & Accessory Suppliers
2018 FOOTWEAR & ACCESSORY SUPPLIERS Accessories COUNTRY SUPPLIER GROUP FACTORY NAME ADDRESS China Charming Gifts Vanvon Manufacturing Limited WORKERS <500 Ground Floor, No. 6 Beach Wai Tangxia Village OAR ID CN2019085021Z9N Tangxia Township Jiangmen GEOLOCATION 22.6804167 113.0128255 China GOLD MEDAL Zhejiang Meikan Garment& Accessories Co.,LTD WORKERS <500 No.318Xiachuan Road Haining OAR ID CN2019085EX7Q5R Zhejiang GEOLOCATION 30.54275905 120.7132257 China GOLD MEDAL Zhejiang Sunmans Knitting Co., Ltd WORKERS <500 No. 139 Biyun North Rd Haining OAR ID CN20190857W3QS0 Zhejiang GEOLOCATION 30.54765065 120.7068713 Page 1 of 53 2018 FOOTWEAR & ACCESSORY SUPPLIERS Accessories COUNTRY SUPPLIER GROUP FACTORY NAME ADDRESS China GOLD MEDAL zhejiang laxdi kniting co.,ltd WORKERS <500 north industrial zone xiaoshun town OAR ID CN2019085RSNH23 jindong area jinhua city GEOLOCATION zhejiang 29.1826594 119.8505314 China HOBO DONG GUAN YEN HENG LEATHER GOODS MFG. CO. LTD. WORKERS 501 - 1,000 DA YUAN HUA YUAN GONG YE INDUSTRIAL ZONE SHI XIA VILLAGE OAR ID CN2019085K8ZH5T DA LANG TOWN DONG GUAN CITY GEOLOCATION GUANG DONG PROVINCE 22.912898 113.975477 China Landau Sacamoto Hao Lang leatherware WORKERS <500 Yang Qiao Town south section huizhou OAR ID CN2019085HG0YT3 bo luo county Guangdong GEOLOCATION 516100 23.4333652 114.4779661 Page 2 of 53 2018 FOOTWEAR & ACCESSORY SUPPLIERS Accessories COUNTRY SUPPLIER GROUP FACTORY NAME ADDRESS China Laurence C Dongguan Jiankai Leather Co., Ltd. WORKERS <500 No.18 Hou Sha Road ChongKou District OAR ID CN20190866HHYZG Houjie Town Dongguan GEOLOCATION Guangdong 22.922366 113.627927 China Leatherlove ZhuHai Xing Fa Handbag Mgf. Ltd. WORKERS <500 2602 Ping Dong Road Ping Sha District OAR ID CN20190853EP5MA Zhu Hai Guangdong GEOLOCATION 22.092658 113.2045493 China Marigold YI WU OU YI LEATHER PRODUCT CO. -
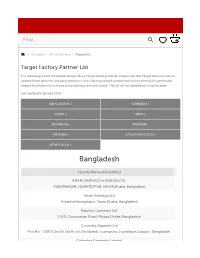
Factory List
Our Latest Home, Women's and Men's Offers Shop Now › Find... Company Ethical Sourcing Factory List Target Factory Partner List The following is a list of factories that produce Target brand products. Please note that Target does not own or operate these factories, any party wishing to visit a factory should contact that factory directly for permission, respect local laws and customs around privacy and site access. This list will be updated on a regular basis. Last updated 9 January 2018. BANGLADESH > CAMBODIA > CHINA > INDIA > INDONESIA > PAKISTAN > VIETNAM > OTHER NON OECD > OTHER OECD > Bangladesh Factory Name and Address AMAN GRAPHICS & DESIGN LTD. NAZIMNAGAR, HEMAYETPUR, SAVAR,Dhaka, Bangladesh Aman Knittings Ltd KulashurHemayetpur, Savar,Dhaka, Bangladesh Babylon Garments Ltd 2-B/1, Darussalam Road, Mirpur,Dhaka, Bangladesh Columbia Apparels Ltd Plot No - 228/1 (2nd & 3rd floor),Tin Sharak, Luxmipura, Joydebpur,Gazipur, Bangladesh Columbia Garments Limited Columbia Garments Limited Homepage › VograChandana, Gazipur Sadar,Gazipur, Bangladesh Dazzling Dresses Ltd. Women 51-52,Shah Kabir Mazar Road,Dhaka, Bangladesh Epyllion Styles Limited Beauty BahadurpurVhawal Mirzapur,Gazipur, Bangladesh Baby Flamingo Fashions Ltd. Mariali, Joydebpur,Gazipur, Bangladesh Kids Frank Apparels Ltd Frank Complex280/D,Chittagong, Bangladesh Men Impress- Newtex Composite Textiles Limited Home Moin Nogor, GoraiMirzapur,Tangail,Dhaka, Bangladesh KDS Garment Industries Ltd Toy2s55, Nasirabad Industrial Area Baizidbostami Road,Chittagong, Bangladesh Kenpark Bangladesh (Pvt) Limited (K-6) EntertaiSnF FSmB# 7eFacntoryt Bay Area,Chittagong, Bangladesh Kenpark Bangladesh (Pvt.) Limited (K-1) SpPolot r31–t 4 2&, Sec tOor 8u, Chtittdagoong Eoxporrt Processing Zone,Chittagong, Bangladesh Sale MASCOT FASHIONS LTD 146, DEWAN IDRIS ROAD, ZIRABO,YEARPUR, ASHULIA, DHAKA,Dhaka, Bangladesh My Account Newage Apparels Limited South Norshingpur, Nischintapur,Zirabo, Asulia, Savar,Dhaka, Bangladesh Help Noman Terry Towel Mills Ltd.