Glaucoma : Science and Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Suppression of Keratoepithelin and Myocilin by Small Interfering Rnas (Sirna) in Vitro Ching Yuan University of Minnesota - Twin Cities
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2007 Suppression of keratoepithelin and myocilin by small interfering RNAs (siRNA) in vitro Ching Yuan University of Minnesota - Twin Cities Emily J. Zins University of Minnesota - Twin Cities Abbott .F Clark Alcon Research Ltd. Andrew J.W. Huang Washington University School of Medicine in St. Louis Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Yuan, Ching; Zins, Emily J.; Clark, Abbott .;F and Huang, Andrew J.W., ,"Suppression of keratoepithelin and myocilin by small interfering RNAs (siRNA) in vitro." Molecular Vision.13,. 2083-2095. (2007). https://digitalcommons.wustl.edu/open_access_pubs/1812 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. Molecular Vision 2007; 13:2083-95 <http://www.molvis.org/molvis/v13/a236/> ©2007 Molecular Vision Received 25 July 2007 | Accepted 24 October 2007 | Published 7 November 2007 Suppression of keratoepithelin and myocilin by small interfering RNAs (siRNA) in vitro Ching Yuan,1 Emily J. Zins,1 Abbott F. Clark,2 Andrew J.W. Huang1,3 1Department of Ophthalmology, University of Minnesota Minneapolis, MN; 2Alcon Research Ltd., Fort Worth, TX; 3Department of Ophthalmology and Visual Sciences, Washington University, St. Louis, MO Purpose: Mutations of keratoepithelin (KE) and myocilin (MYOC) have been linked to certain types of inherited corneal stromal dystrophy and open-angle glaucoma, respectively. We investigated the potential use of small interfering RNAs (siRNAs) to suppress the expression of KE and MYOC and the related cytotoxicity of mutant myocilins in vitro. -

The Very Long Mystery of Epsilon Aurigae
A Unique Eclipsing Variable TheThe VeryVery LongLong MMysteryystery ofof EpsilonEpsilon AAurigaeurigae robertrobert e. sstenceltencel one of the great scientifi c advances of the 20th A remarkable naked-eye star century was the theory of stellar evolution, as physicists worked out not just how stars shine, but how they origi- will soon start dimming for nate, live, change, and die. To test theory against reality, however, astronomers had to determine accurate masses the eighth time since 1821. for many diff erent kinds of stars — and this meant analyz- What’s going on is still ing the motions of binary pairs. Theorists also needed the stars’ exact diameters, and this meant analyzing the light not exactly clear. curves of eclipsing binaries in particular. A century ago, S&T ILLUSTRATION BY CASEY REED giants of early astrophysics worked intensely on the prob- lem of eclipsing-binary analysis. Henry Norris Russell’s paper “On the Determination of the Orbital Elements of Eclipsing Variable Stars,” published in 1912, set the stage for what followed. BIG WHITE STAR, BIGGER BLACK PARTNER Epsilon Aurigae, hotter than the Sun and larger than Earth’s entire orbit, pours forth some 130,000 times the Sun’s light — which is why it shines as brightly as 3rd magnitude even from 2,000 light-years away. According to the currently favored model, a long, dark object will start sliding across its middle this summer. The object seems to be an opaque warped disk 10 a.u. wide and appearing roughly 1 a.u. tall. Whatever lies at its center seems to be hidden — though there’s also evidence that we see right through the center. -

PITX2 and FOXC1 Spectrum of Mutations in Ocular Syndromes
European Journal of Human Genetics (2012) 20, 1224–1233 & 2012 Macmillan Publishers Limited All rights reserved 1018-4813/12 www.nature.com/ejhg ARTICLE PITX2 and FOXC1 spectrum of mutations in ocular syndromes Linda M Reis1, Rebecca C Tyler1, Bethany A Volkmann Kloss1,2,KalaFSchilter1,2, Alex V Levin3,RBrianLowry4, Petra JG Zwijnenburg5,ElizaStroh3,UlrichBroeckel1, Jeffrey C Murray6 and Elena V Semina*,1,2 Anterior segment dysgenesis (ASD) encompasses a broad spectrum of developmental conditions affecting anterior ocular structures and associated with an increased risk for glaucoma. Various systemic anomalies are often observed in ASD conditions such as Axenfeld-Rieger syndrome (ARS) and De Hauwere syndrome. We report DNA sequencing and copy number analysis of PITX2 and FOXC1 in 76 patients with syndromic or isolated ASD and related conditions. PITX2 mutations and deletions were found in 24 patients with dental and/or umbilical anomalies seen in all. Seven PITX2-mutant alleles were novel including c.708_730del, the most C-terminal mutation reported to date. A second case of deletion of the distant upstream but not coding region of PITX2 was identified, highlighting the importance of this recently discovered mechanism for ARS. FOXC1 deletions were observed in four cases, three of which demonstrated hearing and/or heart defects, including a patient with De Hauwere syndrome; no nucleotide mutations in FOXC1 were identified. Review of the literature identified several other patients with 6p25 deletions and features of De Hauwere syndrome. The 1.3-Mb deletion of 6p25 presented here defines the critical region for this phenotype and includes the FOXC1, FOXF2, and FOXQ1 genes. -

Microphthalmos Associated with Cataract, Persistent Fetal Vasculature, Coloboma and Retinal Detachment
Case Report Case report: Microphthalmos associated with cataract, persistent fetal vasculature, coloboma and retinal detachment VP Singh1, Shrinkhal2,* 1Professor, 2Junior Resident, Department of Ophthalmology, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh *Corresponding Author: Email: [email protected] Abstract We present here a case of left eye microphthalmos associated with cataract, persistent fetal vasculature (previously known as persistent hyperplastic primary vitreous), iris and retinochoroidal coloboma and retinal detachment. No surgical intervention was done and the patient was kept on regular follow-up. Keywords: Microphthalmos, Cataract, Persistent fetal vasculature, Coloboma, Retinal detachment. Case Summary reacting in left eye. Mature cataract (Fig. 2) was present A 12 years old girl was referred to our department with fundus details not visible. with chief complaint of sudden diminution of vision in left eye for last 20 days. She was apparently well 20 days back, and then incidentally she closed her right eye and noticed diminution of vision in her left eye. Antenatal history was uneventful. There was no history of trauma during delivery or during perinatal period. Parents took her to a local practioner where she was diagnosed with unilateral left eye congenital cataract and referred to our centre. Her visual acuity at presentation was 6/6 in right eye on Snellen’s chart; left eye visual acuity was only 6/60 on Snellen’s visual acuity chart. Intraocular pressure was 18 mm of Hg in right eye and 14 mm of Hg in left eye by Applanation tonometry. There was no history of trauma, fever, headache, any drug intake before she Fig. -

Nei Vision Report.Pdf
VISION RESEARCH A NATIONAL PLAN: 19992003 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES PUBLIC HEALTH SERVICE NATIONAL INSTITUTES OF HEALTH NATIONAL EYE INSTITUTE A Report of the National Advisory Eye Council DEDICATION Not long after the Roys great intellect, careful experimental approach, creation of the National Eye and keen scientific insights earned him the MERIT Institute (NEI) by Congress Award from the NEI and the Friedenwald Award from in 1968, a young, promising the Association for Research in Vision and vision research scientist Ophthalmology. While maintaining an active and named Roy Steinberg vigorous vision research program, Roy also found time received one of the first to serve as an adviser to the National Institutes of Roy H. Steinberg, M.D., Ph.D. NEI Research Career Health and the NEI. He was a member and later Chair Development Awards. This of the Visual Disorders Study Section, the forerunner marked the beginning of of todays Visual Sciences C. He served as Chair of a long and productive association between the NEI the Retinal Diseases Panel for the NEIs Vision and a researcher who served the vision community ResearchA National Plan: 1987 Evaluation and in many ways. Update and as a consultant to the 19781982 and the 19941998 national plans. He authored the highlights With his great breadth of knowledge and sharp mind, and recommendations from two NEI-sponsored Roy had a clearer grasp than most of the many facets workshopsthe first on the Cell Biology of Retinal of retinal research, both clinical and laboratory. Most Detachment in 1986, and the second on Repair and productive scientists establish a single theme to their Replacement to Restore Sight in 1991. -

Naming the Extrasolar Planets
Naming the extrasolar planets W. Lyra Max Planck Institute for Astronomy, K¨onigstuhl 17, 69177, Heidelberg, Germany [email protected] Abstract and OGLE-TR-182 b, which does not help educators convey the message that these planets are quite similar to Jupiter. Extrasolar planets are not named and are referred to only In stark contrast, the sentence“planet Apollo is a gas giant by their assigned scientific designation. The reason given like Jupiter” is heavily - yet invisibly - coated with Coper- by the IAU to not name the planets is that it is consid- nicanism. ered impractical as planets are expected to be common. I One reason given by the IAU for not considering naming advance some reasons as to why this logic is flawed, and sug- the extrasolar planets is that it is a task deemed impractical. gest names for the 403 extrasolar planet candidates known One source is quoted as having said “if planets are found to as of Oct 2009. The names follow a scheme of association occur very frequently in the Universe, a system of individual with the constellation that the host star pertains to, and names for planets might well rapidly be found equally im- therefore are mostly drawn from Roman-Greek mythology. practicable as it is for stars, as planet discoveries progress.” Other mythologies may also be used given that a suitable 1. This leads to a second argument. It is indeed impractical association is established. to name all stars. But some stars are named nonetheless. In fact, all other classes of astronomical bodies are named. -

Supplementary Table 3 Complete List of RNA-Sequencing Analysis of Gene Expression Changed by ≥ Tenfold Between Xenograft and Cells Cultured in 10%O2
Supplementary Table 3 Complete list of RNA-Sequencing analysis of gene expression changed by ≥ tenfold between xenograft and cells cultured in 10%O2 Expr Log2 Ratio Symbol Entrez Gene Name (culture/xenograft) -7.182 PGM5 phosphoglucomutase 5 -6.883 GPBAR1 G protein-coupled bile acid receptor 1 -6.683 CPVL carboxypeptidase, vitellogenic like -6.398 MTMR9LP myotubularin related protein 9-like, pseudogene -6.131 SCN7A sodium voltage-gated channel alpha subunit 7 -6.115 POPDC2 popeye domain containing 2 -6.014 LGI1 leucine rich glioma inactivated 1 -5.86 SCN1A sodium voltage-gated channel alpha subunit 1 -5.713 C6 complement C6 -5.365 ANGPTL1 angiopoietin like 1 -5.327 TNN tenascin N -5.228 DHRS2 dehydrogenase/reductase 2 leucine rich repeat and fibronectin type III domain -5.115 LRFN2 containing 2 -5.076 FOXO6 forkhead box O6 -5.035 ETNPPL ethanolamine-phosphate phospho-lyase -4.993 MYO15A myosin XVA -4.972 IGF1 insulin like growth factor 1 -4.956 DLG2 discs large MAGUK scaffold protein 2 -4.86 SCML4 sex comb on midleg like 4 (Drosophila) Src homology 2 domain containing transforming -4.816 SHD protein D -4.764 PLP1 proteolipid protein 1 -4.764 TSPAN32 tetraspanin 32 -4.713 N4BP3 NEDD4 binding protein 3 -4.705 MYOC myocilin -4.646 CLEC3B C-type lectin domain family 3 member B -4.646 C7 complement C7 -4.62 TGM2 transglutaminase 2 -4.562 COL9A1 collagen type IX alpha 1 chain -4.55 SOSTDC1 sclerostin domain containing 1 -4.55 OGN osteoglycin -4.505 DAPL1 death associated protein like 1 -4.491 C10orf105 chromosome 10 open reading frame 105 -4.491 -

Neuro-Opthalmology (Developments in Ophthalmology, Vol
Neuro-Ophthalmology Developments in Ophthalmology Vol. 40 Series Editor W. Behrens-Baumann, Magdeburg Neuro- Ophthalmology Neuronal Control of Eye Movements Volume Editors Andreas Straube, Munich Ulrich Büttner, Munich 39 figures, and 3 tables, 2007 Basel · Freiburg · Paris · London · New York · Bangalore · Bangkok · Singapore · Tokyo · Sydney Andreas Straube Ulrich Büttner Department of Neurology Department of Neurology Klinikum Grosshadern Klinikum Grosshadern Marchioninistrasse 15 Marchioninistrasse 15 DE–81377 Munich DE–81377 Munich Library of Congress Cataloging-in-Publication Data Neuro-ophthalmology / volume editors, Andreas Straube, Ulrich Büttner. p. ; cm. – (Developments in ophthalmology, ISSN 0250-3751 ; v. 40) Includes bibliographical references and indexes. ISBN 978-3-8055-8251-3 (hardcover : alk. paper) 1. Neuroophthalmology. I. Straube, Andreas. II. Büttner, U. III. Series. [DNLM: 1. Eye Movements–physiology. 2. Ocular Motility Disorders. 3. Oculomotor Muscles–physiology. 4. Oculomotor Nerve-physiology. W1 DE998NG v.40 2007 / WW 400 N4946 2007] RE725.N45685 2007 617.7Ј32–dc22 2006039568 Bibliographic Indices. This publication is listed in bibliographic services, including Current Contents® and Index Medicus. Disclaimer. The statements, options and data contained in this publication are solely those of the individ- ual authors and contributors and not of the publisher and the editor(s). The appearance of advertisements in the book is not a warranty, endorsement, or approval of the products or services advertised or of their effectiveness, quality or safety. The publisher and the editor(s) disclaim responsibility for any injury to persons or property resulting from any ideas, methods, instructions or products referred to in the content or advertisements. Drug Dosage. The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication. -

Eye Abnormalities Present at Birth
Customer Name, Street Address, City, State, Zip code Phone number, Alt. phone number, Fax number, e-mail address, web site Eye Abnormalities Present at Birth Basics OVERVIEW • Single or multiple abnormalities that affect the eyeball (known as the “globe”) or the tissues surrounding the eye (known as “adnexa,” such as eyelids, third eyelid, and tear glands) observed in young dogs and cats at birth or within the first 6–8 weeks of life • Congenital refers to “present at birth”; congenital abnormalities may be genetic or may be caused by a problem during development of the puppy or kitten prior to birth or during birth • The “cornea” is the clear outer layer of the front of the eye; the pupil is the circular or elliptical opening in the center of the iris of the eye; light passes through the pupil to reach the back part of the eye (known as the “retina”); the iris is the colored or pigmented part of the eye—it can be brown, blue, green, or a mixture of colors; the “lens” is the normally clear structure directly behind the iris that focuses light as it moves toward the back part of the eye (retina); the “retina” contains the light-sensitive rods and cones and other cells that convert images into signals and send messages to the brain, to allow for vision GENETICS • Known, suspected, or unknown mode of inheritance for several congenital (present at birth) eye abnormalities • Remaining strands of iris tissue (the colored or pigmented part of the eye) that may extend from one part of the iris to another or from the iris to the lining of the -

Myocilin Is Involved in Ngr1/Lingo-1-Mediated Oligodendrocyte Differentiation and Myelination of the Optic Nerve
The Journal of Neuroscience, April 16, 2014 • 34(16):5539–5551 • 5539 Cellular/Molecular Myocilin Is Involved in NgR1/Lingo-1-Mediated Oligodendrocyte Differentiation and Myelination of the Optic Nerve Heung Sun Kwon,1 Naoki Nakaya,1 Mones Abu-Asab,2 Hong Sug Kim,3 and Stanislav I. Tomarev1 1Retinal Ganglion Cell Biology Section, Laboratory of Retinal Cell and Molecular Biology and 2Histology Core, National Eye Institute, National Institutes of Health (NIH), Bethesda, Maryland 20892, and 3Neuro-Oncology Branch, National Cancer Institute, NIH, Bethesda, Maryland 20892 Myocilin is a secreted glycoprotein that belongs to a family of olfactomedin domain-containing proteins. Although myocilin is detected in several ocular and nonocular tissues, the only reported human pathology related to mutations in the MYOCILIN gene is primary open-angle glaucoma. Functions of myocilin are poorly understood. Here we demonstrate that myocilin is a mediator of oligodendrocyte differentiation and is involved in the myelination of the optic nerve in mice. Myocilin is expressed and secreted by optic nerve astrocytes. Differentiation of optic nerve oligodendrocytes is delayed in Myocilin-null mice. Optic nerves of Myocilin-null mice contain reduced levels of several myelin-associated proteins including myelin basic protein, myelin proteolipid protein, and 2Ј3Ј-cyclic nucleotide 3Ј- phosphodiesterase compared with those of wild-type littermates. This leads to reduced myelin sheath thickness of optic nerve axons in Myocilin-null mice compared with wild-type littermates, and this difference is more pronounced at early postnatal stages compared with adult mice. Myocilin also affects differentiation of oligodendrocyte precursors in vitro. Its addition to primary cultures of differentiating oligodendrocyte precursors increases levels of tested markers of oligodendrocyte differentiation and stimulates elongation of oligoden- drocyte processes. -
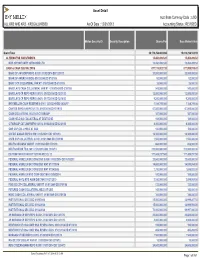
Asset Detail Acct Base Currency Code : USD ALL KR2 and KR3 - KR2GALLKRS00 As of Date : 12/31/2013 Accounting Status : REVISED
Asset Detail Acct Base Currency Code : USD ALL KR2 AND KR3 - KR2GALLKRS00 As Of Date : 12/31/2013 Accounting Status : REVISED . Mellon Security ID Security Description Shares/Par Base Market Value Grand Total 36,179,254,463.894 15,610,214,163.19 ALTERNATIVE INVESTMENTS 15,450,499.520 15,450,499.52 MKP OPPORTUNITY OFFSHORE LTD 15,450,499.520 15,450,499.52 CASH & CASH EQUIVALENTS 877,174,023.720 877,959,915.42 BANC OF AM CORP REPO 0.010% 01/02/2014 DD 12/31/13 20,000,000.000 20,000,000.00 BANK OF AMERICA (BOA) 01/01/2049 DD 07/01/08 52,000.000 52,000.00 BARC CCP COLLATERAL VAR RT 01/01/2049 DD 07/01/08 28,000.000 28,000.00 BARCLAYS CASH COLLATERAL VAR RT 01/01/2049 DD 07/01/08 543,000.000 543,000.00 BARCLAYS CP REPO REPO 0.010% 01/02/2014 DD 12/31/13 12,000,000.000 12,000,000.00 BARCLAYS CP REPO REPO 0.040% 01/17/2014 DD 12/18/13 9,200,000.000 9,200,000.00 BNY MELLON CASH RESERVE 0.010% 12/31/2049 DD 06/26/97 1,184,749.080 1,184,749.08 CANTOR REPO A REPO 0.170% 01/02/2014 DD 12/19/13 67,000,000.000 67,000,000.00 CASH COLLATERAL HELD AT CITIGROUP 387,000.000 387,000.00 CASH HELD AS COLLATERAL AT DEUTSCHE 169,000.000 169,000.00 CITIGROUP CAT 2MM REPO 0.010% 01/02/2014 DD 12/31/13 8,300,000.000 8,300,000.00 CME CCP COLL HELD AT GSC 100,000.000 100,000.00 CREDIT SUISSE REPO 0.010% 01/02/2014 DD 12/31/13 16,300,000.000 16,300,000.00 CSFB CCP COLLATERAL 0.010% 01/01/2049 DD 07/01/08 1,553,000.000 1,553,000.00 DEUTSCHE BANK VAR RT 01/01/2049 DD 07/01/08 668,000.000 668,000.00 DEUTSCHE BK TD 0.180% 01/02/2014 DD 12/18/13 270,000,000.000 270,000,000.00 -

CRISPR-Cas9–Based Treatment of Myocilin-Associated Glaucoma
CRISPR-Cas9–based treatment of myocilin- associated glaucoma Ankur Jaina, Gulab Zodeb,1, Ramesh B. Kasettib, Fei A. Ranc, Winston Yanc, Tasneem P. Sharmad, Kevin Buggea, Charles C. Searbya, John H. Fingertd, Feng Zhangc, Abbot F. Clarkb, and Val C. Sheffielda,d,1 aDepartment of Pediatrics, Carver College of Medicine, University of Iowa, Iowa City, IA 52242; bNorth Texas Eye Research Institute, University of North Texas Health Science Center, Fort Worth, TX 76107; cMcGovern Institute for Brain Research, Massachusetts Institute of Technology, Cambridge, MA 02142; and dStephen A. Wynn Institute for Vision Research, Department of Ophthalmology, Carver College of Medicine, University of Iowa, Iowa City, IA 52242 Edited by Donald J. Zack, Johns Hopkins University, Baltimore, MD, and accepted by Editorial Board Member Jeremy Nathans August 25, 2017 (received for review April 22, 2017) Primary open-angle glaucoma (POAG) is a leading cause of protein itself (transcription or translational inhibition). While irreversible vision loss worldwide, with elevated intraocular pres- siRNA and shRNA provide potentially viable treatment op- sure (IOP) a major risk factor. Myocilin (MYOC) dominant gain-of- tions (31), we elected to directly target the MYOC gene using function mutations have been reported in ∼4% of POAG cases. gene editing with clustered regularly interspaced short palindromic MYOC mutations result in protein misfolding, leading to endoplas- repeats (CRISPR)-Cas9 technology to treat myocilin-associated mic reticulum (ER) stress in the trabecular meshwork (TM), the tis- glaucoma. sue that regulates IOP. We use CRISPR-Cas9–mediated genome Originally part of the prokaryotic adaptive immune system, the editing in cultured human TM cells and in a MYOC mouse model CRISPR-Cas9 system has been adapted as a genome-editing tool, of POAG to knock down expression of mutant MYOC, resulting in in which the Cas9 endonuclease is directed by a guide RNA relief of ER stress.