STARCROSS HOSPITAL: What the Voices Tell Us
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
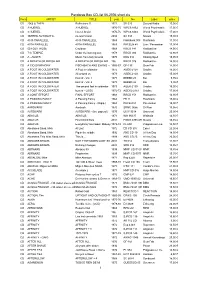
Pandoras Box CD-List 06-2006 Short
Pandoras Box CD-list 06-2006 short.xls Form ARTIST TITLE year No Label price CD 2066 & THEN Reflections !! 1971 SB 025 Second Battle 15,00 € CD 3 HUEREL 3 HUEREL 1970-75 WPC6 8462 World Psychedelic 17,00 € CD 3 HUEREL Huerel Arisivi 1970-75 WPC6 8463 World Psychedelic 17,00 € CD 3SPEED AUTOMATIC no man's land 2004 SA 333 Nasoni 15,00 € CD 49 th PARALLELL 49 th PARALLELL 1969 Flashback 008 Flashback 11,90 € CD 49TH PARALLEL 49TH PARALLEL 1969 PACELN 48 Lion / Pacemaker 17,90 € CD 50 FOOT HOSE Cauldron 1968 RRCD 141 Radioactive 14,90 € CD 7 th TEMPLE Under the burning sun 1978 RRCD 084 Radioactive 14,90 € CD A - AUSTR Music from holy Ground 1970 KSG 014 Kissing Spell 19,95 € CD A BREATH OF FRESH AIR A BREATH OF FRESH AIR 196 RRCD 076 Radioactive 14,90 € CD A CID SYMPHONY FISCHBACH AND EWING - (21966CD) -67 GF-135 Gear Fab 14,90 € CD A FOOT IN COLDWATER A Foot in coldwater 1972 AGEK-2158 Unidisc 15,00 € CD A FOOT IN COLDWATER All around us 1973 AGEK-2160 Unidisc 15,00 € CD A FOOT IN COLDWATER best of - Vol. 1 1973 BEBBD 25 Bei 9,95 € CD A FOOT IN COLDWATER best of - Vol. 2 1973 BEBBD 26 Bei 9,95 € CD A FOOT IN COLDWATER The second foot in coldwater 1973 AGEK-2159 Unidisc 15,00 € CD A FOOT IN COLDWATER best of - (2CD) 1972-73 AGEK2-2161 Unidisc 17,90 € CD A JOINT EFFORT FINAL EFFORT 1968 RRCD 153 Radioactive 14,90 € CD A PASSING FANCY A Passing Fancy 1968 FB 11 Flashback 15,00 € CD A PASSING FANCY A Passing Fancy - (Digip.) 1968 PACE-034 Pacemaker 15,90 € CD AARDVARK Aardvark 1970 SRMC 0056 Si-Wan 19,95 € CD AARDVARK AARDVARK - (lim. -

Environment Agency South West Region
ENVIRONMENT AGENCY SOUTH WEST REGION 1997 ANNUAL HYDROMETRIC REPORT Environment Agency Manley House, Kestrel Way Sowton Industrial Estate Exeter EX2 7LQ Tel 01392 444000 Fax 01392 444238 GTN 7-24-X 1000 Foreword The 1997 Hydrometric Report is the third document of its kind to be produced since the formation of the Environment Agency (South West Region) from the National Rivers Authority, Her Majesty Inspectorate of Pollution and Waste Regulation Authorities. The document is the fourth in a series of reports produced on an annua! basis when all available data for the year has been archived. The principal purpose of the report is to increase the awareness of the hydrometry within the South West Region through listing the current and historic hydrometric networks, key hydrometric staff contacts, what data is available and the reporting options available to users. If you have any comments regarding the content or format of this report then please direct these to the Regional Hydrometric Section at Exeter. A questionnaire is attached to collate your views on the annual hydrometric report. Your time in filling in the questionnaire is appreciated. ENVIRONMENT AGENCY Contents Page number 1.1 Introduction.............................. .................................................... ........-................1 1.2 Hydrometric staff contacts.................................................................................. 2 1.3 South West Region hydrometric network overview......................................3 2.1 Hydrological summary: overview -

The London Gazette, 26Th January 1990
1208 THE LONDON GAZETTE, 26TH JANUARY 1990 Name Location Maximum Length Type of Scale of Charges and of Stay Vehicle Special Conditions Exeter Road Newton Abbot 48 hours A B Scale III Abbotsbury Road Newton Abbot 48 hours A B Scale II Multi-Storey Newton Abbot 12 hours B Levels 1-6 Scale VIII and Levels 7-8 Scale XX Closed between 6.30 p.m. and 6.0 a.m. Carlisle Street Newton Abbot No restriction A B Scale II Devon Square Newton Abbot No restriction AB Scale I & II Wolborough Street Newton Abbot No restriction A B Scale VIII and Scale II Elm Road Newton Abbot No restriction A B Scale III Highweek entrance Newton Abbot No restriction A B Scale II Halcyon Road Newton Abbot No restriction A B Scale II Racecourse Newton Abbot 48 hours C D Scale I Multi-Storey (Basement) Newton Abbot 48 hours E Scale Xffl and Scale XVII Back Road Newton Abbot No restriction A B Scale II Gestridge Road Kings teign ton 48 hours A B Scale I Brook Street Teignmouth 48 hours AB Scale IV Teign Street Teignmouth 48 hours AB Scale IV Brunswick Street Teignmouth 48 hours A B Scale IV Lr. Bitton Car Park Teignmouth 48 hours A B Scale I The Point Teignmouth 48 hours AB Scale VIA XIV Eastcliff Teignmouth 48 hours ABC Scale V, XVI and XIV Lower Point Teignmouth 48 hours AB Scale VI The Ness Shaldon 48 hours A B Scale V Ness Overflow Shaldon 48 hours A B Scale V Labrador Bay Shaldon 12 hours A B Closed from 9 p.m. -

West of Exeter Route Resilience Study Summer 2014
West of Exeter Route Resilience Study Summer 2014 Photo: Colin J Marsden Contents Summer 2014 Network Rail – West of Exeter Route Resilience Study 02 1. Executive summary 03 2. Introduction 06 3. Remit 07 4. Background 09 5. Threats 11 6. Options 15 7. Financial and economic appraisal 29 8. Summary 34 9. Next steps 37 Appendices A. Historical 39 B. Measures to strengthen the existing railway 42 1. Executive summary Summer 2014 Network Rail – West of Exeter Route Resilience Study 03 a. The challenge the future. A successful option must also off er value for money. The following options have been identifi ed: Diffi cult terrain inland between Exeter and Newton Abbot led Isambard Kingdom Brunel to adopt a coastal route for the South • Option 1 - The base case of continuing the current maintenance Devon Railway. The legacy is an iconic stretch of railway dependent regime on the existing route. upon a succession of vulnerable engineering structures located in Option 2 - Further strengthening the existing railway. An early an extremely challenging environment. • estimated cost of between £398 million and £659 million would Since opening in 1846 the seawall has often been damaged by be spread over four Control Periods with a series of trigger and marine erosion and overtopping, the coastal track fl ooded, and the hold points to refl ect funding availability, spend profi le and line obstructed by cliff collapses. Without an alternative route, achieved level of resilience. damage to the railway results in suspension of passenger and Option 3 (Alternative Route A)- The former London & South freight train services to the South West peninsula. -

Fine Books and Manuscripts Books Fine
Wednesday 21 March 2018 21 March Wednesday FINE BOOKS AND MANUSCRIPTS FINE BOOKS AND MANUSCRIPTS | Knightsbridge, London | Wednesday 21 March 2018 24633 FINE BOOKS AND MANUSCRIPTS Wednesday 21 March 2018 at 10am Knightsbridge, London BONHAMS ENQUIRIES Please see page 2 for bidder Montpelier Street Matthew Haley information including after-sale Knightsbridge Simon Roberts collection and shipment. London SW7 1HH Luke Batterham www.bonhams.com Sarah Lindberg Please see back of catalogue +44 (0) 20 7393 3828 for important notice to bidders VIEWING +44 (0) 20 7393 3831 Sunday 18 March ILLUSTRATIONS 11am - 3pm Shipping and Collections Front cover: Lot 83 Monday 19 March Leor Cohen Back cover: Lot 245 9am - 4.30pm +44 (0) 20 7393 3841 Tuesday 20 March +44 (0) 20 7393 3879 Fax 9am - 4.30pm [email protected] Please note that Bonhams will be closed Friday 30 March BIDS PRESS ENQUIRIES 2018 – Monday 2 April 2018 +44 (0) 20 7447 7447 [email protected] for the Easter Holiday. +44 (0) 20 7447 7401 fax [email protected] CUSTOMER SERVICES To bid via the internet Monday to Friday please visit www.bonhams.com 8.30am – 6pm +44 (0) 20 7447 7447 New bidders must also provide proof of identity when submitting LIVE ONLINE BIDDING IS bids. Failure to do this may result AVAILABLE FOR THIS SALE in your bids not being processed. Please email [email protected] with “Live bidding” in the subject Please note that bids should be line up to 48 hours before the submitted no later than 4pm on auction to register for this service. -

Devon County Council Surface Water Management Plan Phase 1
Devon County Council Surface Water Management Plan Phase 1 – Strategic Assessment 28 February 2012 Rev: A Contents Glossary 1 Introduction 1 1.1 Introduction to a Surface Water Management Plan 1 1.2 Links to Sea and Main River Flooding 2 1.3 Methodology and Objectives 2 1.4 Outputs from Phase 1 4 1.5 Local Flood Risk Management Partnerships 5 2 Data Collation 6 2.1 Collation of Available Data 6 2.2 Observations from Data Review 8 3 Review of Other Flood Risk Management Studies 10 3.1 Introduction 10 3.2 National Surface Water Mapping Studies 10 3.3 Preliminary Flood Risk Assessment 12 3.4 Strategic Flood Risk Assessments 14 3.5 Catchment Flood Management Plans 19 3.6 Integrated Urban Drainage Studies 21 4 Local Flooding and Environmentally Sensitive Areas 22 4.1 Introduction 22 4.2 Legislative Context 22 4.3 Methodology 22 4.4 Results 24 5 Local Flooding and Heritage Assets 26 5.1 Introduction 26 6 Local Flooding and Impounded Water Bodies 28 7 Groundwater Flooding 29 7.1 Introduction 29 7.2 Recorded Incidents of Groundwater Flooding 29 7.3 Predicted Risk of Groundwater Flooding 30 7.4 Summary 31 8 Areas Identified for Development 34 8.1 The Importance of Planning in Flood Risk Management 34 8.2 Proposed Development in East Devon 35 8.3 Proposed Development in Exeter 37 8.4 Proposed Development in Mid Devon 38 8.5 Proposed Development in North Devon and Torridge 38 Devon SWMP – Phase 1 Strategic Assessment 8.6 Proposed Development in South Hams 39 8.7 Proposed Development in Teignbridge 39 8.8 Proposed Development in West Devon 41 9 Observations -
Black's Guide to Devonshire
$PI|c>y » ^ EXETt R : STOI Lundrvl.^ I y. fCamelford x Ho Town 24j Tfe<n i/ lisbeard-- 9 5 =553 v 'Suuiland,ntjuUffl " < t,,, w;, #j A~ 15 g -- - •$3*^:y&« . Pui l,i<fkl-W>«? uoi- "'"/;< errtland I . V. ',,, {BabburomheBay 109 f ^Torquaylll • 4 TorBa,, x L > \ * Vj I N DEX MAP TO ACCOMPANY BLACKS GriDE T'i c Q V\ kk&et, ii £FC Sote . 77f/? numbers after the names refer to the page in GuidcBook where die- description is to be found.. Hack Edinburgh. BEQUEST OF REV. CANON SCADDING. D. D. TORONTO. 1901. BLACK'S GUIDE TO DEVONSHIRE. Digitized by the Internet Archive in 2010 with funding from University of Toronto http://www.archive.org/details/blacksguidetodevOOedin *&,* BLACK'S GUIDE TO DEVONSHIRE TENTH EDITION miti) fffaps an* Hlustrations ^ . P, EDINBURGH ADAM AND CHARLES BLACK 1879 CLUE INDEX TO THE CHIEF PLACES IN DEVONSHIRE. For General Index see Page 285. Axniinster, 160. Hfracombe, 152. Babbicombe, 109. Kent Hole, 113. Barnstaple, 209. Kingswear, 119. Berry Pomeroy, 269. Lydford, 226. Bideford, 147. Lynmouth, 155. Bridge-water, 277. Lynton, 156. Brixham, 115. Moreton Hampstead, 250. Buckfastleigh, 263. Xewton Abbot, 270. Bude Haven, 223. Okehampton, 203. Budleigh-Salterton, 170. Paignton, 114. Chudleigh, 268. Plymouth, 121. Cock's Tor, 248. Plympton, 143. Dartmoor, 242. Saltash, 142. Dartmouth, 117. Sidmouth, 99. Dart River, 116. Tamar, River, 273. ' Dawlish, 106. Taunton, 277. Devonport, 133. Tavistock, 230. Eddystone Lighthouse, 138. Tavy, 238. Exe, The, 190. Teignmouth, 107. Exeter, 173. Tiverton, 195. Exmoor Forest, 159. Torquay, 111. Exmouth, 101. Totnes, 260. Harewood House, 233. Ugbrooke, 10P. -

Planning Committee
PLANNING COMMITTEE Dear Councillor NOTICE IS HEREBY GIVEN that a Meeting of the Planning Committee at which your attendance is summoned, will be held at Remote Meeting - Zoom on Thursday, 3rd December 2020 at 7.00 pm to transact the business specified in the Agenda as set out. To join the meeting, please click the following link or click the ‘Join Meeting’ button in the Zoom app and enter the meeting ID: 837 0251 9351 and Password: 418048. If wishing to join by telephone, please dial: +44 203 481 5237 United Kingdom Note – calls are charged at Zoom rates and +44 203 481 5240 United Kingdom are payable by the user. More info at +44 131 460 1196 United Kingdom https://zoom.us/zoomconference/rates +44 203 051 2874 United Kingdom After dialling the number when requested enter the meeting ID 83702519351 with no spaces followed by #, then when prompted for participant ID enter #, then when prompted for meeting password enter 418048 followed by # Yola Mitchell Finance Officer Distribution: The Mayor and Members of Planning Committee as follows: Councillors Goodman-Bradbury (Chairman), Taylor (Deputy Chairman), Heath, M. Lowther, Mayne, Tamlyn, Wrigley, Foden (ex-Officio) and Mawhood (ex-Officio) For information – to be taken as read: 1 Declarations of Interest – Members are reminded that they should declare any interest in the items to be considered and are also advised that the timescale to alter their stated interests with the District Council’s Monitoring Officer is 28 days. 2 Items requiring urgent attention – to consider those items which, in the opinion of the Committee Chair, should be considered by the meeting as matter of urgency (if any). -

Transport Information
TIVERTON www.bicton.ac.uk 1hr 30mins CULLOMPTON TRANSPORT TRANSPORT GUIDELINES 55mins - The cost for use of the daily transport for all non-residential students can be paid for per HONITON INFORMATION term or in one payment in the Autumn term to cover the whole year - Autumn, Spring & CREDITON 45mins Summer terms. 1hr 5mins AXMINSTER 1hr 10mins - No knives to be taken onto the contract buses or the college campus. - Bus passes will be issued on payment and must be available at all times for inspection. BICTON COLLEGE - Buses try to keep to the published times, please be patient if the bus is late it may have EXETER been held up by roadworks or a breakdown, etc. If you miss the bus you must make 30 - 45mins your own way to college or home. We will not be able to return for those left behind. - SEAT BELTS MUST BE WORN. DAWLISH LYME REGIS - All buses arrive at Bicton College campus by 9.00am. 1hr 25mins 1hr 20mins - Please ensure that you apply to Bicton College for transport. SIDMOUTH 15mins - PLEASE BE AT YOUR BUS STOP 10 MINUTES BEFORE YOUR DEPARTURE TIME. NEWTON ABBOT - Buses leave the campus at 5.00pm. 1hr SEATON 1hr - Unfortunately transport cannot be offered if attending extra curricular activities e.g. staying TEIGNMOUTH late for computer use, discos, late return from sports fixtures, equine duties or work 1hr 15mins experience placements. - Residential students can access the transport to go home at weekends by prior arrangement with the Transport Office. - Bicton College operates a no smoking policy in all of our vehicles. -

University Public Transport Map and Guide 2018
Fancy a trip to Dartmouth Plymouth Sidmouth Barnstaple Sampford Peverell Uffculme Why not the beach? The historic port of Dartmouth Why not visit the historic Take a trip to the seaside at Take a trip to North Devon’s Main Bus has a picturesque setting, maritime City of Plymouth. the historic Regency town main town, which claims to be There are lots of possibilities near Halberton Willand Services from being built on a steep wooded As well as a wide selection of of Sidmouth, located on the the oldest borough in England, try a day Exeter, and all are easy to get to valley overlooking the River shops including the renowned Jurassic Coast. Take a stroll having been granted its charter Cullompton by public transport: Tiverton Exeter Dart. The Pilgrim Fathers sailed Drakes Circus shopping centre, along the Esplanade, explore in 930. There’s a wide variety Copplestone out by bus? Bickleigh Exmouth – Trains run every from Dartmouth in 1620 and you can walk up to the Hoe the town or stroll around the of shops, while the traditional Bradninch There are lots of great places to half hour and Service 57 bus many historic buildings from for a great view over Plymouth Connaught Gardens. Pannier Market is well worth Crediton runs from Exeter Bus station to Broadclyst visit in Devon, so why not take this period remain, including Sound, visit the historic a visit. Ottery St Mary Exmouth, Monday to Saturday Dartmouth Castle, Agincourt Barbican, or take a trip to view Exeter a trip on the bus and enjoy the Airport every 15 mins, (daytime) and Newton St Cyres House and the Cherub Pub, the ships in Devonport. -

Dawlish-Teignmouth Cliffs Unmanned Aerial Vehicle (UAV) Survey Interpretation Report
EXETER TONEWTON ABBOT GEO - ENVIRONMENTAL RESILIENCE STUDY Dawlish-Teignmouth Cliffs Unmanned Aerial Vehicle (UAV) Survey Interpretation Report Prepared for Network Rail October 2016 Halcrow Group Ltd. Burderop Park Wroughton SN4 0QD Exeter to Newton Abbot Geo-Environmental Resilience Study Dawlish-Teignmouth Cliffs Unmanned Aerial Vehicle (UAV) Survey Interpretation Report October 2016 Notice This document and its contents have been prepared and are intended solely for Network Rail’s information and use in relation to the Exeter to Newton Abbot Geo-Environmental Resilience Study. CH2M assumes no responsibility to any other party in respect of or arising out of or in connection with this document and/or its contents. Document History Version Date Description Created by Verified by Approved by 1 Oct 2016 Draft Oliver Dabson Roger Moore Peter Barter DAWLISH-TEIGNMOUTH CLIFFS UAV SURVEY INTERPRETATION REPORT Contents Section Page Contents ....................................................................................................................................... i Acronyms and abbreviations ........................................................................................................ ii 1. Introduction .................................................................................................................... 1 1.1 Summary ....................................................................................................................... 1 1.2 Data processing and quality control ............................................................................ -
![DEVON and SLAVERY Traders and Settlers [2] the African Presence in Devon the Davy Family Prospered Through Slave Ownership](https://docslib.b-cdn.net/cover/0493/devon-and-slavery-traders-and-settlers-2-the-african-presence-in-devon-the-davy-family-prospered-through-slave-ownership-1120493.webp)
DEVON and SLAVERY Traders and Settlers [2] the African Presence in Devon the Davy Family Prospered Through Slave Ownership
LEGACIES OF BRITISH SLAVE-OWNERSHIP DEVON AND SLAVERY Traders and settlers [2] The African presence in Devon The Davy family prospered through slave ownership. In the Medieval church carvings of Africans in Devon include 1760s, James Davy, a tenant farmer at Wear Barton. started Politicians and landowners a pew end in Sandford Church depicting a person with to run some small businesses importing coal and lime by extremely tight curls, and a black saint in Uffculme boat up the Exe estuary. His son Robert became interested Denys Rolle (1725–1797) of Stevenstone, North Devon Church, which may also have been a pew end. There in repairing and then building these small boats and went and MP for Barnstaple 1761–77, was awarded land in are records of Africans, described in the language on to build large sailing ships, including West Indiamen. the Bahamas after Britain lost the American War of of the time (‘negarre’, ‘neyger’, ‘blackmore’, ‘negro’, Independence in 1783. His son, John Rolle (1751–1842) ‘black’) in sources such as parish records, a news Robert’s younger brothers James Davy (1765–1825) and thus became the largest slave owner in the Bahamas and broadsheet, a private diary and in paintings from Edward (1776–1803) travelled to Jamaica in the 1790s also acquired extensive land in Devon from his uncle. the sixteenth century onwards. The status of such where they bought properties growing coffee and allspice John Rolle was MP for the county of Devon 1780–96 and individuals is unclear but their presence in Devon was and raising cattle, all using slave labour.