New Approaches for Reversing Oral Factor Xa Inhibitors EXAMINING the EVIDENCE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Current Sustaining Member Companies
CURRENT SUSTAINING MEMBER COMPANIES MEMBER FOR OVER: 10 Years 25 Years 50 Years Member Since (alphabetical order) 1976 3M Medical Markets Center 2010 Endo Pharmaceuticals 1963 Novartis Pharmaceuticals 2019 10-Square Solutions 2019 EMD Serono, Inc. 2019 Novo Nordisk, Inc. 1985 Abbott Laboratories, Inc. 2017 Exelixis 2019 Optinose 2013 AbbVie Inc. 2016 Express Scripts Federal Pharmacy 2018 Organogenesis 2017 ACADIA Pharmaceuticals, Inc. 2010 Federal Practitioner 2004 Otsuka America Pharmaceutical, Inc. 2019 Aimmune 2018 Foundation Medicine, Inc. 2018 Pacira BioSciences, Inc. 2003 Alcon Laboratories, Inc. 2006 Gilead Sciences 2018 Paratek Pharmaceuticals 2017 Alkermes, Inc. 1989 Genentech Inc. 1990 Pfizer Pharmaceuticals 2002 Allergan, Inc. 1983 GLAXOSMITHKLINE 2017 Pharmacyclics, LLC 2019 Almirall LLC 2013 Golden State Medical Supply, Inc. 2019 Portola Pharmaceuticals, Inc. 2019 Alnylam Pharmaceuticals 2019 Greenwich Biosciences 2019 Red One Medical 2019 Altarum Institute 2013 Gulf Coast Pharmaceuticals Plus, LLC 2009 Regenesis Biomedical, Inc. 2012 American Medical Depot 2008 Heritage Health Solutions, Inc. 2019 Relypsa, Inc. 2019 Aptive Resources LLC 2017 Hill-Rom Company 2011 Remund Group, LLC 2013 Arbor Pharmaceuticals, LLC 2018 Hu-Friedy Manufacturing Co 2018 Rigel Pharmaceuticals 2014 Argentum Medical, LLC 2019 Indivior 2016 Sage Products, LLC 2019 ASM Research, LLC 2019 ImmunoVation, LLC 2018 Sage Therapeutics 1986 Astellas Pharma US, Inc. 2019 Incyte Corporation 2000 Sanofi 1995 AstraZeneca 2015 Intercept Pharmaceuticals 2004 Siemens Medical Solutions 2018 Avanir Pharmaceuticals 2019 Ipsen Biopharmaceuticals, Inc. 2019 SK Life Science, Inc. 2017 Bausch Health Companies, Inc. 2018 IT Cadre 2002 Smith & Nephew, Inc. 1985 Baxter Healthcare Corporation 1989 J & J Health Care Systems, Inc. 2019 Sobi Inc. 1996 Bayer Corporation 2014 Jazz Pharmaceuticals Inc. -
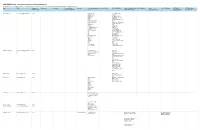
2020-2021 Cancer Communications Committee Disclosures All Relationships Are Considered Compensated
2020-2021 Cancer Communications Committee Disclosures All relationships are considered compensated. Relationships are self-held unless otherwise noted. I = Immediate Family Member, Inst = My Institution Name EMAIL Committee Employment Leadership Stock and Other Honoraria Consulting or Advisory Speakers' Bureau Research Funding Patents, Royalties, Other Expert Testimony Travel, Other Relationship (OPTIONAL) (OPTIONAL) Open Member Status Ownership Interests Role Intellectual Property Accommodations, Uncompensated Payments Link Expenses Relationships Neeraj Agarwal [email protected] Active Astellas Pharma Active Biotech (Inst) Astellas Pharma Amgen (Inst) AstraZeneca AstraZeneca (Inst) AstraZeneca Bavarian Nordic (Inst) AVEO Bayer (Inst) Bayer BN ImmunoTherapeutics Bristol-Myers Squibb (Inst) Calithera Biosciences Bristol-Myers Squibb (Inst) Eisai Calithera Biosciences EMD Serono (Inst) Exelixis Celldex (Inst) Foundation Medicine Eisai (Inst) Foundation One Inc Exelixis (Inst) Genentech Genentech (Inst) Janssen Oncology GlaxoSmithKline (Inst) Lilly Immunomedics (Inst) Lilly Janssen (Inst) lily Merck (Inst) Medivation/Astellas Newlink Genetics (Inst) MEI Pharma Novartis (Inst) Merck Pfizer (Inst) Nektar Prometheus (Inst) Novartis Rexahn Pharmaceuticals Pfizer (Inst) Pfizer Sanofi (Inst) Pharmacyclics Takeda (Inst) Seattle Genetics TRACON Pharma (Inst) Muhammad S. Beg muhammad.beg@utsouthwestern. Active Array BioPharma Agios (Inst) edu AstraZeneca/MedImmune ArQule (Inst) Cancer Commons AstraZeneca/MedImmune Ipsen (Inst) Legend Biotech -

News Release Tel
Bayer Pharma AG 13342 Berlin Germany News Release Tel. +49 30 468-1111 Not intended for U.S. and UK Media www.bayerpharma.com Portola Pharmaceuticals Announces Initial Phase II Results Demonstrating Dose-Dependent Reversal of Bayer’s Xarelto® Anticoagulation Activity with Andexanet Alfa (PRT4445) Data set with additional dosing cohorts to be presented at 55th American Society of Hematology (ASH) Annual Meeting and Exposition Berlin, Germany, November 11, 2013 – Bayer HealthCare announced today that initial results from a Phase II proof-of-concept study of Portola Pharmaceuticals’ andexanet alfa, an investigational Factor Xa inhibitor antidote, in healthy volunteers who were administered Bayer’s novel oral anticoagulant Xarelto® (rivaroxaban) have been accepted for presentation at the 55th American Society of Hematology (ASH) Annual Meeting and Exposition, which is being held in New Orleans, LA, USA, from December 7-10, 2013. Initial results from the first two dosing cohorts of the study, submitted by Portola Pharmaceuticals and now published online on the ASH website, demonstrated that andexanet alfa is able to dose-dependently reverse the anticoagulant effects of Xarelto. In addition, no serious adverse events were reported. These data, as well as data from additional cohorts evaluating higher doses of andexanet alfa, will be presented in a poster session on December 9. “Xarelto is a highly effective anticoagulant, and in previous Phase III studies has been shown to significantly reduce the risk of the most concerning bleeding events compared to warfarin. In rare emergency situations when the normalization of blood clotting becomes necessary, stopping Xarelto would allow for normalization of coagulation parameters within one day – this is as effective as giving Vitamin K to patients receiving warfarin,” said Kemal Malik, M.D., Member of the Bayer HealthCare Executive Committee and Head of Global Development. -

For Immediate Release
______________________________________________________________________________________ FOR IMMEDIATE RELEASE Clinical Trial Application to Conduct Phase III APEX Study of Betrixaban in China was Accepted for Review by China FDA Hong Kong, 28 August 2013 - Lee’s Pharmaceutical Holdings Limited (“the Group”) (Main Board Stock Code: 0950; Website: www.leespharm.com) today announced that the Group has successfully submitted an application to the China FDA to expand the Phase 3 APEX ( Acute Medically Ill VTE Prevention with Ex tended Duration Betrixaban) Study of Portola Pharmaceutical’s (Nasdaq: PTLA)_betrixaban into the Chinese population. APEX is an ongoing global randomized Phase 3 clinical study that is evaluating betrixaban, a novel, oral, once-daily Factor Xa inhibitor, for hospital and post-discharge prevention of venous thromboembolism (VTE) in high-risk acute medically ill patients. Currently, there is no anticoagulant approved for extended-duration VTE prophylaxis in this population. Betrixaban directly inhibits the activity of Factor Xa, an important validated target in the blood coagulation pathway. It is specifically designed for chronic, once-a-day treatment, with a half-life that supports true, once-daily dosing and a low peak-to-trough drug concentration ratio that minimizes anticoagulant variability. The clinical study application was submitted with the fast-tract designation, and has been accepted for review by the CFDA (Acceptance Notice Nos. JXHL1300320–40mg & JXHL1300321–80mg). “We’re pleased with the acceptance of review by the CFDA for this important application,” said Dr. Benjamin Li, Chief Executive Officer. “We are looking forward to moving the registration process forward and we’re very anxious for the China trial to get underway in the APEX Study next year.” About Betrixaban and the APEX Study Betrixaban is a novel, oral small molecule that directly inhibits the activity of Factor Xa, an important validated target in the blood coagulation pathway. -

Portola AHA Xa Inhibitor Antidote
Contacts: Mardi Dier Joey Fleury CFO, Portola Pharmaceuticals Invigorate AHA onsite mobile: 415-509-3632 AHA onsite cell: 925-784-5829 Portola Pharmaceuticals Announces Investigational Universal Factor Xa Inhibitor Antidote Reverses Anticoagulant Activity of Factor Xa Inhibitors – Findings Presented During Oral Presentation at AHA Scientific Sessions – – Elinogrel Data Selected by AHA for “Best of Specialty Conferences” Poster Session – CHICAGO AND SOUTH SAN FRANCISCO, Calif. (November 15, 2010) – Portola Pharmaceuticals, Inc. today announced preclinical study results for PRT064445, its universal Factor Xa inhibitor antidote, demonstrating that the agent can reverse the pharmacodynamic effects of anticoagulation by enoxaparin, a low molecular weight heparin, and fondaparinux, both Factor Xa inhibitors, and reduce blood loss caused by these compounds in an animal model. Previously, Portola presented proof of concept data showing that PRT064445 has the potential to act as a universal antidote to reverse the pharmacodynamic effects of all current and novel Factor Xa inhibitors. The new data were presented today by Portola in the “Novel Concepts for Anticoagulation and Fibrinolysis” oral session from 9 a.m. to noon Central Time during the American Heart Association (AHA) Scientific Sessions 2010 in Chicago. Today, Factor Xa inhibitors are widely used for the treatment and prevention of blood clots. By 2020, they are expected to be used by more than 40 million patients. However, Factor Xa inhibitors can cause clinically relevant bleeding and their anticoagulant activity may need to be reversed in some patients, including those with bleeding-related medical emergencies or those requiring cessation of anticoagulation prior to surgery. No antidote for Factor Xa inhibitors is currently available, and use of procoagulative treatment strategies have potential risks of unwanted thrombosis. -

Portola Pharmaceuticals Announces Data Presentations Highlighting
Contacts: Mardi Dier Jani Bergan CFO, Portola Pharmaceuticals Invigorate 650-246-7236 415-572-1353 Portola Pharmaceuticals Announces Data Presentations Highlighting Syk/JAK Inhibitor Clinical Development Program at 52nd American Society of Hematology Annual Meeting SOUTH SAN FRANCISCO, Calif. (December 4, 2010) – Portola Pharmaceuticals, Inc. today announced the presentation of preclinical study results for its novel Syk and JAK inhibitor program at the American Society of Hematology’s 52nd Annual Meeting and Exposition. Portola’s novel Syk and JAK inhibitors are in development to treat chronic inflammatory diseases, including rheumatoid arthritis, and certain cancers, including non-Hodgkin’s lymphoma and chronic lymphocytic leukemia. Poster Presentation Details Specific Inhibition of Syk Suppresses Leukocyte Immune Function and Alleviates Inflammation In Rodent Models of Rheumatoid Arthritis • Presenter: Greg Coffey, Ph.D., Portola Pharmaceuticals • Poster Session: Lymphocytes, Lymphocyte Activation and Immunodeficiency, Including HIV and Other Infections: Poster I • Date: Saturday, December 4, 5:30 - 7:30 p.m. ET • Location: Hall A3/A4 (Orange County Convention Center) • Poster Board I-707 P505-15, a Highly Selective SYK Inhibitor, Shows Significant Activity in Primary CLL Cells and is Synergistic with Fludarabine at Low Concentrations • Presenter: Stephen Spurgeon, M.D., Oregon Health & Science University Knight Cancer Institute • Poster Session: Lymphoma - Pre-Clinical - Chemotherapy and Biologic Agents: Poster I • Date: Sunday, December 5, 6:00 - 8:00 p.m. ET • Location: Hall A3/A4 (Orange County Convention Center) • Poster Board II-719 Spleen Tyrosine Kinase (Syk) Inhibitors Block B Cell Receptor Signaling and Survival In Chronic Lymphocytic Leukemia • Presenter: Jan Burger, M.D., Ph.D., MD Anderson Cancer Center • Poster Session: CLL - Biology and Pathophysiology, excluding Therapy: Poster III • Date: Monday, December 6, 6:00 - 8:00 p.m. -

News Release - Portola Pharmaceuticals, Inc
3/30/2019 Investors - News Release - Portola Pharmaceuticals, Inc. News Release Portola Pharmaceuticals Expands Clinical Collaboration Agreement with Daiichi Sank Worth Up to $25 Million to Develop AndexXa™ (andexanet alfa) in Germany SOUTH SAN FRANCISCO, Calif., Nov. 01, 2016 (GLOBE NEWSWIRE) -- Portola Pharmaceuticals Inc.® (Nasdaq:PTLA) tod announced that it has expanded its existing clinical collaboration agreement with Daiichi Sankyo to develop AndexXa (andexanet alfa) as an antidote for edoxaban, Daiichi Sankyo’s Factor Xa inhibitor. AndexXa is currently under EMA re reversal of Factor Xa inhibition in patients experiencing a life-threatening or uncontrolled bleed and for patients requ urgent or emergency surgery. As part of the updated agreement, Portola will expand the ongoing ANNEXA-4 study in patients in Germany. “As an industry, we need to address the signicant unmet medical need for managing Factor Xa inhibitor-related ma bleeding by bringing to market an antidote that specically reverses anti-Factor Xa activity, the anticoagulant mechan these agents. With this support from Daiichi Sankyo, we will be able to improve our ability to gather data on AndexXa reversal agent for edoxaban. Germany is the second largest market for Factor Xa inhibitors and one where edoxaba experienced signicant growth,” said Tao Fu, chief commercial and business ocer of Portola. “Our long-standing collaboration with Daiichi Sankyo, as well as all of the other manufacturers of Factor Xa inhibitors, demonstrates the condence these companies have in the AndexXa program.” Under the terms of the non-exclusive agreement with Daiichi Sankyo, Portola will receive a $15 million upfront paym is eligible to receive up to an additional $10 million upon meeting site initiation and enrollment targets. -

PORTOLA PHARMACEUTICALS INC Form 10-K Annual Report Filed
SECURITIES AND EXCHANGE COMMISSION FORM 10-K Annual report pursuant to section 13 and 15(d) Filing Date: 2019-03-01 | Period of Report: 2018-12-31 SEC Accession No. 0001564590-19-005772 (HTML Version on secdatabase.com) FILER PORTOLA PHARMACEUTICALS INC Mailing Address Business Address 270 EAST GRAND AVENUE, 270 EAST GRAND AVENUE, CIK:1269021| IRS No.: 000000000 | State of Incorp.:DE | Fiscal Year End: 1231 SUITE 22 SUITE 22 Type: 10-K | Act: 34 | File No.: 001-35935 | Film No.: 19648587 SOUTH SAN FRANCISCO CA SOUTH SAN FRANCISCO CA SIC: 2834 Pharmaceutical preparations 94080 94080 650-244-6864 Copyright © 2019 www.secdatabase.com. All Rights Reserved. Please Consider the Environment Before Printing This Document UNITED STATES SECURITIES AND EXCHANGE COMMISSION WASHINGTON, D.C. 20549 FORM 10-K (Mark One) ☒ ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the Fiscal Year Ended December 31, 2018 or ☐ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 Commission File Number: 001-35935 PORTOLA PHARMACEUTICALS, INC. (Exact name of registrant as specified in its charter) Delaware 2834 20-0216859 (State or other jurisdiction of (Primary Standard Industrial (I.R.S. Employer incorporation or organization) Classification Code Number) Identification No.) 270 E. Grand Avenue South San Francisco, California 94080 (Address of Principal Executive Offices) (Zip Code) (650) 246-7000 (Registrant’s Telephone Number, Including Area Code) Securities registered pursuant to Section 12(b) of the Act: Title of Each Class: Name of Each Exchange on which Registered Common Stock, par value $0.001 per share The Nasdaq Global Select Market Securities registered pursuant to Section 12(g) of the Act: None Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. -

TSHP Virtual Seminar 2020 Partner, Supporter, and Exhibitor Listing
TSHP Virtual Seminar 2020 Partner, Supporter, and Exhibitor Listing Abbvie https://www.abbvie.com/ ___________________________________________________________________________________ AcelRx Pharmaceuticals http://www.acelrx.com AcelRx Pharmaceuticals, Inc. is a specialty pharmaceutical company focused on the development and commercialization of innovative therapies for use in medically supervised settings. In November of 2018, its lead product candidate DSUVIA™ (sufentanil sublingual tablet 30 mcg) was approved by the U.S. Food and Drug Administration. ___________________________________________________________________________________ AIS Healthcare http://www.aiscaregroup.com The leading 503A specialty pharmacy and targeted drug delivery care provider, AIS Healthcare is driven to improve the everyday lives of patients and providers, in ways big and small. From higher quality and sterility standards to services that improve care delivery, we do what’s right, not just what’s expected— every time. ___________________________________________________________________________________ Allergan http://www.allergan.com Allergan is a world leader in neuromodulator therapy and neurosciences. For over three decades, we have been committed to the research and clinical development of BOTOX® (OnabotulinumtoxinA), one of the world’s most versatile medicines, to improve the physical well-being and resulting quality of life for people around the world who suffer from a variety of serious or debilitating disorders. BOTOX® is available in more than 75 countries with 20 approved indications. ___________________________________________________________________________________ AMAG Pharmaceuticals http://www.amagpharma.com AMAG is a pharmaceutical company focused on bringing innovative products to patients with unmet medical needs. Every day the people at AMAG aim higher, devoting our passion and perseverance to finding new and better ways to support the health of patients and families. For additional company information, please visit www.amagpharma.com. -

Global Health an ONLINE JOURNAL for the DIGITAL AGE
Global Health AN ONLINE JOURNAL FOR THE DIGITAL AGE alfa also inhibits tissue factor pathway inhibitor, which leads to an increase in tissue factor-initiated thrombin generation.1 In terms of safety, andexanet alfa does have a Black Box Warning for serious and life- threatening effects such as arterial and venous thromboembolic events, ischemic events, cardiac arrest, and sudden deaths. Due to these Ralf Jadoopat risks, patients should be closely monitored and Pharm D. Candidate 2019 anticoagulation should be initiated only when The University of Findlay College of medically appropriate. The most common Pharmacy adverse event based on clinical trial data was Findlay, OH infusion-related reactions (frequency of 18%). USA 45840 These reactions included flushing, cough, [email protected] dysgeusia, and dyspepsia. The symptoms were mild-to-moderate in severity and 90% of REVIEW OF ANDEXANET ALFA AND patients experiencing these effects did not IMPLICATIONS FOR GLOBAL HEALTH require treatment.1,2 There are two dosing regimens available for As direct oral anticoagulants (DOACs) are andexanet alfa. The regimen used is based on being more frequently prescribed, there is a specific factor Xa inhibitor given, the factor Xa pressing need for a reversal agent for these inhibitor dose, and time since it was last medications. Dabigatran was the first DOAC administered. The low dose regimen is a 400mg to have a specific reversal agent with the IV bolus administered at a rate of 30mg/min, approval of idarucizumab (Praxbind®). A new followed by a 4mg/min IV infusion for up to reversal agent called andexanet alfa 120min. The high dose regimen is an 800mg IV (Andexxa®), manufactured by Portola bolus administered at a rate of 30mg/min, Pharmaceuticals and was approved by FDA in followed by an 8mg/min IV infusion for up to May 2018 for patients treated with 120min.1,2 rivaroxaban or apixaban that are experiencing Each package of andexanet alfa contains four life-threatening or uncontrolled bleeding. -

2019 Annual Report
Dear Shareholders, ǨǦǧǯDžîƙîNjĚîƑūIJƙĿijŠĿǛČîŠƥîČČūŞƎŕĿƙĺŞĚŠƥƙIJūƑ¡ūƑƥūŕîîƙDžĚŞîēĚƥĺĚƥƑîŠƙĿƥĿūŠƥū îijŕūċîŕČūŞŞĚƑČĿîŕūƑijîŠĿǕîƥĿūŠȦ~ƭƑǜîijƙĺĿƎŞĚēĿČĿŠĚȡŠēĚNJNJî® ȱČūîijƭŕîƥĿūŠIJîČƥūƑÝî ȳƑĚČūŞċĿŠîŠƥȴȡĿŠîČƥĿDŽîƥĚēȹǕĺǕūȲȡĿƙŠūDžîDŽîĿŕîċŕĚƥūĺūƙƎĿƥîŕƙîŠēƎîƥĿĚŠƥƙĿŠƥĺĚÀŠĿƥĚē¬ƥîƥĚƙ îŠēîijƑūDžĿŠijŠƭŞċĚƑūIJ/ƭƑūƎĚîŠČūƭŠƥƑĿĚƙȦØĚîČĺĿĚDŽĚēƙĚDŽĚƑîŕŕîŠēŞîƑŒŞĿŕĚƙƥūŠĚƙIJūƑŠēĚNJNJî îŠē~ŠēĚNJNJNjîʆȳîŠēĚNJîŠĚƥîŕIJîȫƥĺĚƥƑîēĚŠîŞĚIJūƑŠēĚNJNJîĿŠ/ƭƑūƎĚȴƥĺîƥDžĿŕŕēƑĿDŽĚƥĺĚIJƭƥƭƑĚijƑūDžƥĺ ūIJƥĺĚČūŞƎîŠNjîŠēƙƭƎƎūƑƥūƭƑDŽĿƙĿūŠƥūēĚŕĿDŽĚƑŕĿIJĚȹƙîDŽĿŠijƥƑĚîƥŞĚŠƥƙIJūƑƙĚƑĿūƭƙċŕūūēȹƑĚŕîƥĚēēĿƙūƑēĚƑƙȦ U.S. COMMERCIAL LAUNCH ÀŠĿƥĚēeĿŠijēūŞîŠēƥĺĚƑǕŠĚĿŞĿƥƥĚŕŞîƑŒƥȹ ƥĺĚijŕūċîŕ ~×T'ȹǧǯƎîŠēĚŞĿČȡDžĺĿČĺĺîƙ OF ANDEXXA sĚƭūƑēŠƭŠijƙijĚƙĚƥǕȳqs~HȴĿŠHĚƑŞîŠNjȡ ČĺîŠijĚēîŕŕîƙƎĚČƥƙūIJūƭƑēîĿŕNjŕĿDŽĚƙîŠēƥĺĚ îŕŕūDžĿŠijIJūƑĿŠĿƥĿîŕƙîŕĚƙĿŠƥĺĚƙĚĿŞƎūƑƥîŠƥ DžîNjĿŠDžĺĿČĺDžĚČūŠēƭČƥċƭƙĿŠĚƙƙȦƙDžĚ ǨǦǧǯDžîƙƥĺĚǛƑƙƥIJƭŕŕNjĚîƑūIJƥĺĚŠēĚNJNJî ŞîƑŒĚƥƙĿŠƥĺĚƙĚČūŠēĺîŕIJūIJǨǦǧǯîŠēƙĚƥƥĿŠij ŠîDŽĿijîƥĚƥĺƑūƭijĺƥĺĿƙƎîŠēĚŞĿČȡ¡ūƑƥūŕîɄƙǛƑƙƥ ŕîƭŠČĺĿŠƥĺĚÀȦ¬ȦIJūŕŕūDžĿŠijƥĺĚîƎƎƑūDŽîŕūIJ ƥĺĚƙƥîijĚIJūƑƑĚĿŞċƭƑƙĚŞĚŠƥČūDŽĚƑîijĚ ƎƑĿūƑĿƥNjĿƙƥĺĚĺĚîŕƥĺîŠēƙîIJĚƥNjūIJĚŞƎŕūNjĚĚƙȡ ūƭƑƙĚČūŠēȹijĚŠĚƑîƥĿūŠŞîŠƭIJîČƥƭƑĿŠijƎƑūČĚƙƙ decisions in 2020. ƎîƥĿĚŠƥƙîŠēĺĚîŕƥĺČîƑĚƎƑūDŽĿēĚƑƙȦØĚĺîDŽĚ ƥîŒĚŠƎƑūîČƥĿDŽĚƙƥĚƎƙƥūŞĿƥĿijîƥĚƥĺĚƙƎƑĚîē ūŠ'ĚČĚŞċĚƑǩǧȡǨǦǧǮȦ~DŽĚƑƥĺĚČūƭƑƙĚūIJƥĺĚ ØĚîƑĚĚNJČĿƥĚēƥūŞūDŽĚČŕūƙĚƑƥūŞîŒĿŠij ūIJƥĺĚDŽĿƑƭƙDžĺĿŕĚîŕƙūDžūƑŒĿŠijƥūƎƑūDŽĿēĚ NjĚîƑȡDžĚîēēĚēǪǨǫŠĚDžĺūƙƎĿƥîŕČƭƙƥūŞĚƑƙIJūƑ ~ŠēĚNJNJNjîîDŽîĿŕîċŕĚƥūƎîƥĿĚŠƥƙĿŠƥĺĚƙĚŞîƑŒĚƥƙ ƭŠĿŠƥĚƑƑƭƎƥĚēƙƭƎƎūƑƥƥūĚŠƙƭƑĚƥĺîƥĺūƙƎĿƥîŕƙ îƥūƥîŕūIJǬǪǦĺūƙƎĿƥîŕƙƥĺîƥĺîDŽĚŠūDžūƑēĚƑĚē îŠēƥĺĚƑĚƙƥūIJ/ƭƑūƎĚȡIJƭƑƥĺĚƑĚNJƎîŠēĿŠijîČČĚƙƙ ČîŠČūŠƥĿŠƭĚƥūƭƙĚîŠēƑĚȹūƑēĚƑŠēĚNJNJîIJūƑ ŠēĚNJNJîĿŠƥĺĚÀȦ¬Ȧ¹ūijĚƥĺĚƑȡDžĚĚƙƥĿŞîƥĚƥĺîƥ ƥūƥĺĚǛƑƙƥîŠēūŠŕNjîƎƎƑūDŽĚēƑĚDŽĚƑƙîŕîijĚŠƥ ƎîƥĿĚŠƥƙƥîŒĿŠijƑĿDŽîƑūNJîċîŠūƑîƎĿNJîċîŠƥĺîƥ -

Current Sustaining Member Companies
CURRENT SUSTAINING MEMBER COMPANIES Member Since (alpabetical order) 1976 3M Medical Markets Center 2010 Endo Pharmaceuticals 1963 Novartis Pharmaceuticals 2019 10-Square Solutions 2019 EMD Serono, Inc. 2016 Novo Nordisk, Inc. 1954 Abbott Laboratories, Inc. 2017 Exelixis 2018 Organogenesis 2013 AbbVie Inc. 2016 Express Scripts Federal Pharmacy 2004 Otsuka America Pharmaceutical, Inc. 2017 ACADIA Pharmaceuticals, Inc. 2010 Federal Practitioner 2018 Pacira BioSciences, Inc. 2019 Aimmune 2018 Foundation Medicine, Inc. 2018 Paratek Pharmaceuticals 2003 Alcon Laboratories, Inc. 2018 Fujifilm Medical Systems USA 1990 Pfizer Pharmaceuticals 2017 Alkermes, Inc. 1989 Fujifilm Medical Systems USA 2017 Pharmacyclics, LLC 2002 Allergan, Inc. 2006 Gilead Sciences 2019 Portola Pharmaceuticals, Inc. 2012 American Medical Depot 2013 Golden State Medical Supply, Inc. 2009 Regenesis Biomedical, Inc. 2019 Alnylam Pharmaceuticals 2019 Greenwich Biosciences 2019 Relypsa, Inc. 2013 Arbor Pharmaceuticals, LLC 2013 Gulf Coast Pharmaceuticals Plus, LLC 2011 Remund Group, LLC 2014 Argentum Medical, LLC 2008 Heritage Health Solutions, Inc. 2018 Rigel Pharmaceuticals 2019 ASM Research, LLC 2017 Hill-Rom Company 2016 Sage Products, LLC 1986 Astellas Pharma US, Inc. 2018 Hu-Friedy Manufacturing Co 2018 Sage Therapeutics 1995 AstraZeneca 2019 Incyte Corporation 2000 Sanofi 2018 Avanir Pharmaceuticals 2015 Intercept Pharmaceuticals 2004 Siemens Medical Solutions 2017 Bausch Health Companies, Inc. 2018 IT Cadre 2019 SK Life Science, Inc. 1985 Baxter Healthcare Corporation 1989 J & J Health Care Systems, Inc. 2002 Smith & Nephew, Inc. 1996 Bayer Corporation 2014 Jazz Pharmaceuticals Inc. 2013 Stryker Orthopaedics 1954 BD 2007 Karl Storz Endoscopy America 2018 Sun Pharmaceutical 2018 Beacon Health Options, Inc. 2010 LLC Federal Solutions 1999 Sunoovion Pharmaceuticals, Inc. 2002 Biogen 2014 Lovell Government Services LLC 2016 Taiho Oncology, Inc.