New Patient Paperwork
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

This Book Belongs
ThisThis book book belongs belongs to: to: Family Notebook Index 1. Admission to the NICN Letter to parents from NICN Staff . .3 Letter to parents from Neonatal Pain Committee . .4 Visitation policy . .5 Breastfeeding in the NICN . .7 Feeding Log and Daily Diary . .9 “Welcome to the World” announcement . .13 2. Stabilization: Understanding the NICN environment Insurance Information . .15 People you may meet—doctors, nurses and other staff . .17 Case Management Team . .19 Your baby’s Physical Environment (sound, light, positioning, handling and touch) . .21 Feeding and Nutrition . .25 Respiratory Distress Syndrome . .26 MRSA ............................................................................28 Reminders: Family Resource Library, Family Focus, CaringBridge . .29 Smoking Cessation Program . .30 3. Growing: Caring for your baby in the NICN CordCare .........................................................................31 Using a Bulb Syringe . .31 Taking a Temperature . .32 Play ............................................................................34 4. Almost Home: Transfer to NPCN Letter to Parents from NPCN staff . .37 “Are You Ready for Your Baby to Go Home” Checklist . .39 Planning for baby’s homecoming—carseats, CPR classes, Basic Baby II class . .41 Car seat Basics . .42 5. Homecoming Day: Caring for your baby at home Bottle-feeding (forms of formula; feeding problems, like reflux and colic; vitamins; iron; fluoride; how to make formula) . .45 Bathing . .55 Circumcision . .57 Diapering . .59 Outings . .60 Visitors . .60 Temperature of Your Home . .61 Fussy Babies . .62 Illness . .64 Choking . .65 Safety and home safety checklist . .66 Safe Sleeping . .71 6. References Dictionary . .73 Resources . .81 Special Needs and Other Information . .85 Dear Parents, Congratulations on the birth of your baby. The staff of the Neonatal Intensive Care Nursery (NICN) and the Neonatal Progressive Care Nursery (NPCN) would like to welcome you. -

NICU Guide to Baby Care the Jennifer Gandel Kachura Neonatal Intensive Care Unit at Sinai Hospital NICU Guide to Baby Care
The Jennifer Gandel Kachura Neonatal Intensive Care Unit at Sinai Hospital NICU Guide to Baby Care The Jennifer Gandel Kachura Neonatal Intensive Care Unit at Sinai Hospital NICU Guide to Baby Care Dear Parent, Welcome to the Neonatal Intensive Care Please understand that everyone’s privacy Unit (NICU) at Sinai Hospital. Our goal is important to us. Therefore, we ask that is to provide your baby with the best care while in the NICU, you stay at your baby’s possible in a safe and family-centered bedside. environment. Your presence is important to your newborn, and our staff will help We try to keep noise at a minimum. Please you learn all about your new baby. That’s put your phone on vibrate and step outside why we consider you a care partner and the nursery for phone conversations. encourage you to be with your baby Remember to sanitize your phones and whenever possible. tablets frequently, and be sure to wash your hands before handling your baby. Please provide us with a list of up to six other adults, not including your baby’s We only have two family rooms for everyone siblings, who would be most helpful to to use, so please value your time there and you. Your list will be kept at the security treat the rooms and their contents with desk for identification when they arrive. respect. Though small, the Family Lounge They will not be allowed to hold your is also available for your use. baby or participate in your baby’s care Preventing infection is one of the most unless you give your approval. -

Returning Patient Paperwork
Dr. Ronnie G. Smalling, MD, FACC, FSCAI Smalling Vascular Institute – INVEIN 11025 Metcalf Ave Overland Park, KS 66210 (913) 912-3624 Welcome to IN VEIN by Smalling Vascular Institute. We are glad that you have chosen to receive vascular care within our office. Thank you for your trust. We are committed to your LEG HEALTH. Office Policies: Hours: Monday- Friday 9:00 am to 4:30 pm If communicating with the office after hours, please leave a message and someone will respond to you as soon as possible. If it is an emergency, please visit your local Emergency Department. Contact Information: Phone- 913.912.3624 / Fax- 913.717.6362 / Email: [email protected] Test Results: Please allow 5 to 10 days minimum for the physician to receive and review your test results or submit your insurance paperwork. Finance/Insurance: Each patient is responsible for payment of his/her medical bills unless otherwise stated in your new patient paperwork. Co-pays are due at the time services are rendered. We CAN NOT mediate disputes or resolves differences between you and your insurance company. Please keep in mind that it is your responsibility to advise our office immediately of any change in your insurance and contact information to ensure accuracy of care and to continue coverage so neither party is left with a bill being denied by your insurance provider. Appointment/Procedure Cancellation: When scheduled for a procedure, be aware that the time of your appointment may be later than initially scheduled. Please try to keep a clear schedule after your appointment on procedure days. -

Heartburn and Gastroesophageal Reflux Disease
Heartburn and Gastroesophageal Reflux Disease What Is Heartburn And Gastroesophageal Reflux Disease? The esophagus, commonly called the food pipe, is a narrow muscular tube, about nine and a half inches long, that begins below the tongue and ends at the stomach. It consists of three basic layers: an outer layer of fibrous tissue, a middle layer containing smoother muscle, and an inner membrane, which contains numerous tiny glands. The esophagus is narrowest at the top and bottom; it also narrows to a lesser degree in the middle, where it passes the aorta. Wave-like muscle contractions, known as peristalsis, move food down through the esophagus and into the stomach. In the stomach, acid and various enzymes, notably hydrochloric acid and pepsin, break down and digest the starch, fat, and protein in food. Unlike the lining of the stomach, which has a thin layer of protective mucus, the lining of the esophagus offers only a weak defense against stomach acid and other harmful substances. Perhaps the most important structure in protecting the esophagus is the lower esophageal sphincter (LES), which is a band of muscle around the bottom of the esophagus where it meets the stomach. The LES opens after a person swallows to let food enter the stomach and then immediately closes to prevent regurgitation of the stomach contents, including gastric acid. It maintains this pressure barrier until food is swallowed again. If, in spite of LES pressure, there is some acid back-up (reflux), an additional defense mechanism, the peristaltic action of the esophagus, pushes the residue back down into the stomach. -

Dysphagia from Wikipedia, the Free Encyclopedia Jump To: Navigation
Dysphagia From Wikipedia, the free encyclopedia Jump to: navigation, search Not to be confused with Dysphasia. Dysphagia ICD-10 R13 ICD-9 438.82, 787.2 DiseasesDB 17942 MedlinePlus 003115 eMedicine pmr/194 MeSH D003680 Dysphagia is the medical term for the symptom of difficulty in swallowing.[1][2][3] Although classified under "symptoms and signs" in ICD-10,[4] the term is sometimes used as a condition in its own right.[5][6][7] Sufferers are sometimes unaware of their dysphagia.[8][9] It is derived from the Greek dys meaning bad or disordered, and phago meaning "eat". It may be a sensation that suggests difficulty in the passage of solids or liquids from the mouth to the stomach,[10] a lack of pharyngeal sensation, or various other inadequacies of the swallowing mechanism. Dysphagia is distinguished from other symptoms including odynophagia, which is defined as painful swallowing,[11] and globus, which is the sensation of a lump in the throat. A psychogenic dysphagia is known as phagophobia. It is also worthwhile to refer to the physiology of swallowing in understanding dysphagia. Contents 1 Signs and symptoms 2 Differential diagnosis 3 Diagnostic approach 4 Epidemiology 5 References 6 See also 7 External links Signs and symptoms Some patients have limited awareness of their dysphagia, so lack of the symptom does not exclude an underlying disease.[12] When dysphagia goes undiagnosed or untreated, patients are at a high risk of pulmonary aspiration and subsequent aspiration pneumonia secondary to food or liquids going the wrong way into the lungs. Some people present with "silent aspiration" and do not cough or show outward signs of aspiration. -

The Complete Digestive Health Guide Final November 09
The Complete Digestive Health Guide The Complete Digestive Health Guide Empowering You with Knowledge and Solutions for Sustainable Good Health Edition 14 June 2010 Health & Personal Care Disclaimer: Content in this eBook is for reference purposes and is not intended to substitute for advice given by a physician, pharmacist, or other licensed health-care professional. You should not use this information as self-diagnosis or for treating a health problem or disease. Contact your health-care provider immediately if you suspect that you have a medical problem. Information and statements regarding dietary supplements have not been evaluated by the Food and Drug Administration and are not intended to diagnose, treat, cure, or prevent any disease or health condition. Page 1 of 89 Copyright © 2006 - 2010 www.perfectly-natural-health.com The Complete Digestive Health Guide COPYRIGHT NOTICE Copyright © 2006 - 2010 Published by www.perfectly-natural-health.com All rights reserved. All contents contained in “The Complete Digestive Health Guide” is protected under © Copyright 2006 - 2010. All literary work contained within “The Complete Digestive Health Guide” belongs to and is the sole property of www.perfectly-natural-health.com and can only be reprinted with permission. Reproduction, copying, or any other form of use of any part of this book is STRICTLY FORBIDDEN without the express and written permission of www.perfectly-natural- health.com. If perjury is discovered the offenders will be prosecuted to the full extent of the law. These rules have been established to protect the rights and ownership of the publisher. If you feel that someone else could benefit from a copy of this book, please ask them to visit www.perfectly-natural-health.com to get their own copy. -
(PROMIS) Gastrointestinal Symptom Scales
nature publishing group ORIGINAL CONTRIBUTIONS 1 see related editorial on page x Development of the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) Gastrointestinal Symptom Scales Brennan M.R. Spiegel , MD, MSHS, RFF, FACG, AGAF 1 , 2 , 3 , 4 , Ron D. Hays , PhD 4 , 5 , Roger Bolus , PhD 2 , Gil Y. Melmed , MD, MS 1 , Lin Chang , MD5 , 6 , Cynthia Whitman , MPH 2 , Puja P. Khanna , MD, MPH 7 , Sylvia H. Paz , PhD 4 , Tonya Hays , MS 4 , Steve Reise , PhD 8 and Dinesh Khanna , MD, MSc 7 OBJECTIVES: The National Institutes of Health (NIH) Patient-Reported Outcomes Measurement Information System (PROMIS ® ) is a standardized set of patient-reported outcomes (PROs) that cover physical, mental, and social health. The aim of this study was to develop the NIH PROMIS gastrointestinal (GI) symptom measures. METHODS: We fi rst conducted a systematic literature review to develop a broad conceptual model of GI symp- toms. We complemented the review with 12 focus groups including 102 GI patients. We developed FUNCTIONAL GI DISORDERS PROMIS items based on the literature and input from the focus groups followed by cognitive de- briefi ng in 28 patients. We administered the items to diverse GI patients (irritable bowel syndrome (IBS), infl ammatory bowel disease (IBD), systemic sclerosis (SSc), and other common GI disorders) and a census-based US general population (GP) control sample. We created scales based on con- fi rmatory factor analyses and item response theory modeling, and evaluated the scales for reliability and validity. RESULTS: A total of 102 items were developed and administered to 865 patients with GI conditions and 1,177 GP participants. -

Newborn Care Info.Docx
Newborn Care ALL THE LITTLE THINGS YOU FORGOT TO ASK… Umbilical Cord The umbilical cord stump will generally fall off in a week or 2. Please keep the area dry. You do not need to apply anything (i.e. alcohol) and please do not bathe the baby until it falls off. Keep the area as open to air as possible. When the stump falls off, it may be moist, bleed a bit, or have a yellow discharge. These things are all normal and will quickly dry-up. Please call your pediatrician if the area is very red or draining fluid regularly. Bathing A warm wet washcloth, every 2-3 days, is all you need until the cord falls off. Newborn’s skin is very dry and flaky. This is normal and will go away on its own. Plain Vaseline on any dry, cracked areas is safe to use. There is no need to use anything on the skin other than water and Vaseline. Nail Care Newborn’s nails grow very quickly, and your baby may have been born with very long, sharp nails. Using an emery board to file the nails, or very carefully using small nail clippers is safe. Eyes Sometimes, newborns have eye discharge or crustiness on and off for several weeks/ months. This is often due to a clogged tear duct. If the eyes are red and/or there are large amounts of discharge all day long, please call the pediatrician. It is normal for up to one year to have intermittent eye discharge/crustiness (without redness), especially after sleep. -

NICU Guide to Baby Care the Jennifer Gandel Kachura Neonatal Intensive Care Unit at Sinai Hospital NICU Guide to Baby Care
The Jennifer Gandel Kachura Neonatal Intensive Care Unit at Sinai Hospital NICU Guide to Baby Care The Jennifer Gandel Kachura Neonatal Intensive Care Unit at Sinai Hospital NICU Guide to Baby Care Dear Parent, Welcome to the Neonatal Intensive Care Please understand that everyone’s privacy Unit (NICU) at Sinai Hospital. Our goal is important to us. Therefore, we ask that is to provide your baby with the best care while in the NICU, you stay at your baby’s possible in a safe and family-centered bedside. environment. Your presence is important to your newborn, and our staff will help We try to keep noise at a minimum. Please you learn all about your new baby. That’s put your phone on vibrate and step outside why we consider you a care partner and the nursery for phone conversations. encourage you to be with your baby Remember to sanitize your phones and whenever possible. tablets frequently, and be sure to wash your hands before handling your baby. Please provide us with a list of up to six other adults, not including your baby’s We only have two family rooms for everyone siblings, who would be most helpful to to use, so please value your time there and you. Your list will be kept at the security treat the rooms and their contents with desk for identification when they arrive. respect. Though small, the Family Lounge They will not be allowed to hold your is also available for your use. baby or participate in your baby’s care Preventing infection is one of the most unless you give your approval. -
Digestive Enzymes
Digestive Wellness March 2010 how to reevaluate and regain control of your digestive health At the University of Chicago Medical Center, we ask questions like this every day. Questions that have the potential to forever CAN BACTERIA change the way gastrointestinal disorders are treated. BE GOOD FOR YOU? DISCOVER FOR YOURSELF. discover.uchospitals.edu | 888-UCH-0200 digestive wellness Eating Right: Optimizing Your Digestive Health By: JESSIE M. PAVlInAC, MS, RD, CSR, lD, PRESIDEnT, AMERICAn DIETETIC ASSoCIATIon At every stage of life, from infancy through our senior years, nutrition is essential to keeping our bodies running at their best. As we age, our nutrient needs change with our bodies. But for those with digestive issues, proper food choices not only CONTENTS help them lead a healthier life, but often a more comfortable life. 2 Eating Right 3 Treating Gastrointestinal Cancers 4 Digestive Enzymes igestive issues are more 96 percent of primary care physicians in nutrition science, others may have 5 Going Organic common than most people believe the nation’s healthcare sys- little if any actual nutrition training or 5 Probiotics And Dthink —approximately one tem should place more emphasis on just mail-order credentials. Even if a Preventive Nutrition in 25 people suffers from a food al - nutrition to treat and manage chronic person holds degrees from accredited 6 Starting Early lergy and many more suffer from food disease. However, only 12 percent be- institutions, nutrition may not be his 6 Should I Go Gluten-Free intolerances. Celiac disease affects an lieve physicians currently pay enough or her specialty. -

Prevalence and Severity Versus Care-Seeking Patients
Dig Dis Sci DOI 10.1007/s10620-014-3181-8 ORIGINAL ARTICLE GERD Symptoms in the General Population: Prevalence and Severity Versus Care-Seeking Patients Erica Cohen • Roger Bolus • Dinesh Khanna • Ron D. Hays • Lin Chang • Gil Y. Melmed • Puja Khanna • Brennan Spiegel Received: 24 December 2013 / Accepted: 20 April 2014 Ó Springer Science+Business Media New York (Outside the USA) 2014 Abstract scale. We then performed multivariable regression to Background Prior estimates suggest that up to 40 % of identify predictors of GERD severity. the US general population (GP) report symptoms of gas- Results There was no difference in the prevalence of troesophageal reflux disease (GERD). However, symptoms heartburn between the GP and patient groups (59 vs. in the GP versus patients seeking care for gastrointestinal 59 %), but regurgitation was more common in patients (GI) complaints have not been compared. We estimated the versus GP (46 vs. 39 %; p = 0.004). In multivariable prevalence and severity of GERD symptoms in the GP regression, having high visceral anxiety (p \ 0.001) and versus GI patients, and identified predictors of GERD being divorced or separated (p = 0.006) were associated severity. We hypothesized that similar to functional GI with higher GERD severity. disorders, psychosocial factors would predict symptom Conclusions More than half of a GP sample reports severity in GERD as much, or perhaps more, than care- heartburn—higher than previous series and no different seeking behavior alone. from GI patients. Although regurgitation was more pre- Methods We compared the prevalence of heartburn and valent in patients versus the GP, there was no difference in regurgitation between a sample from the US GP and GERD severity between groups after adjusting for other patients seeking GI specialty care. -
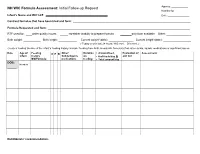
NH WIC Formula Assessment: Initial Follow-Up Request Nutritionist: ______
Agency: ____________ NH WIC Formula Assessment: Initial Follow-up Request Nutritionist: __________ Infant’s Name and WIC Id #: Date: _______________ Contract formulas that have been tried and form: ____________________________________________________________________________ Formula Requested and form: ____________________________________________________________________________________________ RTF used for: ____ water quality issues _____ caretaker inability to prepare formula _____only form available Other: ________________ Birth weight: ___________ Birth length: ____________ Current weight*(date): ________________ Current length*(date): __________________ (*Today or w/in last 24 hours; WIC mmt. Dr’s mmt.) Create a feeding timeline of the infant’s feeding history. Include: feeding from birth, breastmilk, formula(s) fed, other solids, liquids, medications or significant issues. Date Age of Feeding C P R Other: Duration Amount/feed, Evaluation of Assessment infant history Solids/liquids on # of feeds/day & amt fed BM/Formula: medications feeding Total amount/day DOB: Newborn ______ Nutritionists’ recommendation: Assessment—note significant findings. Nutrition needs of the infant Evaluation of feeding issues: Family history of allergies: Formula preparation and storage: 0 to 6months* 6month –1yr** Stomach capacity of newborn What allergies run in the General: Current weight# / 2.2 =KG [Use belly balls to show capacity] family? Tell me how you prepare the formula. KG X 108* [98**] kcal/day= Mom: Does anyone else prepare the formula? ~estimated calories needs Potential issues: Dad: What water do you use to prepare the formula? Under/overfeeding sibling(s): Is the water boiled? Covered or uncovered Estimated calorie needs/20 kcal Newborn 1.5 oz-3oz 2-3 hours pan? For how long? = Number of ounces formula [8-12 X 24] Is the child seen by an needed per day.