Adult-Onset Nemaline Myopathy Presenting As Respiratory Failure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Z-Disc Proteins in Myopathy and Cardiomyopathy
International Journal of Molecular Sciences Review The Role of Z-disc Proteins in Myopathy and Cardiomyopathy Kirsty Wadmore 1,†, Amar J. Azad 1,† and Katja Gehmlich 1,2,* 1 Institute of Cardiovascular Sciences, College of Medical and Dental Sciences, University of Birmingham, Birmingham B15 2TT, UK; [email protected] (K.W.); [email protected] (A.J.A.) 2 Division of Cardiovascular Medicine, Radcliffe Department of Medicine and British Heart Foundation Centre of Research Excellence Oxford, University of Oxford, Oxford OX3 9DU, UK * Correspondence: [email protected]; Tel.: +44-121-414-8259 † These authors contributed equally. Abstract: The Z-disc acts as a protein-rich structure to tether thin filament in the contractile units, the sarcomeres, of striated muscle cells. Proteins found in the Z-disc are integral for maintaining the architecture of the sarcomere. They also enable it to function as a (bio-mechanical) signalling hub. Numerous proteins interact in the Z-disc to facilitate force transduction and intracellular signalling in both cardiac and skeletal muscle. This review will focus on six key Z-disc proteins: α-actinin 2, filamin C, myopalladin, myotilin, telethonin and Z-disc alternatively spliced PDZ-motif (ZASP), which have all been linked to myopathies and cardiomyopathies. We will summarise pathogenic variants identified in the six genes coding for these proteins and look at their involvement in myopathy and cardiomyopathy. Listing the Minor Allele Frequency (MAF) of these variants in the Genome Aggregation Database (GnomAD) version 3.1 will help to critically re-evaluate pathogenicity based on variant frequency in normal population cohorts. -

Current and Emerging Therapies in Becker Muscular Dystrophy (BMD)
Acta Myologica • 2019; XXXVIII: p. 172-179 OPEN ACCESS © Gaetano Conte Academy - Mediterranean Society of Myology Current and emerging therapies in Becker muscular dystrophy (BMD) Corrado Angelini, Roberta Marozzo and Valentina Pegoraro Neuromuscular Center, IRCCS San Camillo Hospital, Venice, Italy Becker muscular dystrophy (BMD) has onset usually in child- tients with a deletion in the dystrophin gene that have nor- hood, frequently by 11 years. BMD can present in several ways mal muscle strength and endurance, but present high CK, such as waddling gait, exercise related cramps with or with- and so far their follow-up and treatment recommenda- out myoglobinuria. Rarely cardiomyopathy might be the pre- senting feature. The evolution is variable. BMD is caused by tions are still a matter of debate. Patients with early cardi- dystrophin deficiency due to inframe deletions, mutations or omyopathy are also a possible variant of BMD (4, 5) and duplications in dystrophin gene (Xp21.2) We review here the may be susceptible either to specific drug therapy and/or evolution and current therapy presenting a personal series of to cardiac transplantation (6-8). Here we cover emerging cases followed for over two decades, with multifactorial treat- therapies considering follow-up, and exemplifying some ment regimen. Early treatment includes steroid treatment that phenotypes and treatments by a few study cases. has been analized and personalized for each case. Early treat- ment of cardiomyopathy with ACE inhibitors is recommended and referral for cardiac transplantation is appropriate in severe cases. Management includes multidisciplinary care with physi- Pathophysiology and rationale of otherapy to reduce joint contractures and prolong walking. -

Nemaline MYOPATHY Myopathy
NEMALINENemaline MYOPATHY Myopathy due to chest muscle weakness, feeding and swallowing What is nemaline myopathy? problems, and speech difficulties. Often, children with the condition have an elongated face and a Nemaline myopathy (NM) is a group of high arched palate. rare, inherited conditions that affect muscle tone and strength. It is also What causes nemaline myopathy? The condition can be caused by a mutation in one known as rod body disease because of several different genes that are responsible for at a microscopic level, abnormal making muscle protein. Most cases of nemaline rod-shaped bodies (nemalines) can myopathy are inherited, although there are some- be seen in affected muscle tissue. times sporadic cases. People with a family history may choose to undergo genetic counseling to help At various stages in life, the muscles of understand the risks of passing the gene on to their the shoulders, upper arms, pelvis and children. thighs may be affected. Symptoms usually start anywhere from birth to What are the types of nemaline myopathy? There are two main groups of nemaline myopathy: early childhood. In rare cases, it is ‘typical’ and ‘severe.’ Typical nemaline myopathy diagnosed during adulthood. NM is the most common form, presenting usually in affects an estimated 1 in 50,000 infants with muscle weakness and floppiness. It may people -- both males and females. be slowly progressive or non progressive, and most adults are able to walk. Severe nemaline myopathy is characterized by absence of spontaneous movement What are the symptoms? or respiration at birth, and often leads to death in Symptoms vary depending on the age of onset of the first months of life. -
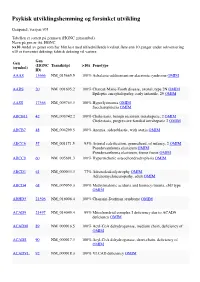
Psykisk Utviklingshemming Og Forsinket Utvikling
Psykisk utviklingshemming og forsinket utvikling Genpanel, versjon v03 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering x10 er forventet dekning; faktisk dekning vil variere. Gen Gen (HGNC Transkript >10x Fenotype (symbol) ID) AAAS 13666 NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AARS 20 NM_001605.2 100% Charcot-Marie-Tooth disease, axonal, type 2N OMIM Epileptic encephalopathy, early infantile, 29 OMIM AASS 17366 NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCB11 42 NM_003742.2 100% Cholestasis, benign recurrent intrahepatic, 2 OMIM Cholestasis, progressive familial intrahepatic 2 OMIM ABCB7 48 NM_004299.5 100% Anemia, sideroblastic, with ataxia OMIM ABCC6 57 NM_001171.5 93% Arterial calcification, generalized, of infancy, 2 OMIM Pseudoxanthoma elasticum OMIM Pseudoxanthoma elasticum, forme fruste OMIM ABCC9 60 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 61 NM_000033.3 77% Adrenoleukodystrophy OMIM Adrenomyeloneuropathy, adult OMIM ABCD4 68 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 21396 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 21497 NM_014049.4 99% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM 89 NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS 90 NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL 92 NM_000018.3 100% VLCAD -

Full Disclosure Forms
Expanding genotype/phenotype of neuromuscular diseases by comprehensive target capture/NGS Xia Tian, PhD* ABSTRACT * Wen-Chen Liang, MD Objective: To establish and evaluate the effectiveness of a comprehensive next-generation * Yanming Feng, PhD sequencing (NGS) approach to simultaneously analyze all genes known to be responsible for Jing Wang, MD the most clinically and genetically heterogeneous neuromuscular diseases (NMDs) involving spi- Victor Wei Zhang, PhD nal motoneurons, neuromuscular junctions, nerves, and muscles. Chih-Hung Chou, MS Methods: All coding exons and at least 20 bp of flanking intronic sequences of 236 genes causing Hsien-Da Huang, PhD NMDs were enriched by using SeqCap EZ solution-based capture and enrichment method fol- Ching Wan Lam, PhD lowed by massively parallel sequencing on Illumina HiSeq2000. Ya-Yun Hsu, PhD ; 3 Thy-Sheng Lin, MD Results: The target gene capture/deep sequencing provides an average coverage of 1,000 per Wan-Tzu Chen, MS nucleotide. Thirty-five unrelated NMD families (38 patients) with clinical and/or muscle pathologic Lee-Jun Wong, PhD diagnoses but without identified causative genetic defects were analyzed. Deleterious mutations Yuh-Jyh Jong, MD were found in 29 families (83%). Definitive causative mutations were identified in 21 families (60%) and likely diagnoses were established in 8 families (23%). Six families were left without diagnosis due to uncertainty in phenotype/genotype correlation and/or unidentified causative Correspondence to genes. Using this comprehensive panel, we not only identified mutations in expected genes but Dr. Wong: also expanded phenotype/genotype among different subcategories of NMDs. [email protected] or Dr. Jong: Conclusions: Target gene capture/deep sequencing approach can greatly improve the genetic [email protected] diagnosis of NMDs. -

Clinical Exome Sequencing for Genetic Identification of Rare Mendelian Disorders
Supplementary Online Content Lee H, Deignan JL, Dorrani N, Strom SP, Kantarci S, Quintero-Rivera F, et al. Clinical exome sequencing for genetic identification of rare Mendelian disorders. JAMA. doi:10.1001/jama.2014.14604. eMethods 1. Sample acquisition and pre-test sample processing eMethods 2. Exome capture and sequencing eMethods 3. Sequence data analysis eMethods 4. Variant filtration and interpretation eMethods 5. Determination of variant pathogenicity eFigure 1. UCLA Clinical Exome Sequencing (CES) workflow eFigure 2. Variant filtration workflow starting with ~21K variants across the exome and comparing the mean number of variants observed from trio-CES versus proband-CES eFigure 3. Variant classification workflow for the variants found within the primary genelist (PGL) eTable 1. Metrics used to determine the adequate quality of the sequencing test for each sample eTable 2. List of molecular diagnoses made eTable 3. List of copy number variants (CNVs) and uniparental disomy (UPD) reported and confirmatory status eTable 4. Demographic summary of 814 cases eTable 5. Molecular Diagnosis Rate of Phenotypic Subgroups by Age Group for Other Clinical Exome Sequencing References © 2014 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 10/01/2021 This supplementary material has been provided by the authors to give readers additional information about their work. © 2014 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 10/01/2021 eMethods 1. Sample acquisition and pre-test sample processing. Once determined by the ordering physician that the patient's presentation is clinically appropriate for CES, patients were offered the test after a counseling session ("pre-test counseling") [eFigure 1]. -

Myopathies Infosheet
The University of Chicago Genetic Services Laboratories 5841 S. Maryland Ave., Rm. G701, MC 0077, Chicago, Illinois 60637 Toll Free: (888) UC GENES (888) 824 3637 Local: (773) 834 0555 FAX: (773) 702 9130 [email protected] dnatesting.uchicago.edu CLIA #: 14D0917593 CAP #: 18827-49 Gene tic Testing for Congenital Myopathies/Muscular Dystrophies Congenital Myopathies Congenital myopathies are typically characterized by the presence of specific structural and histochemical features on muscle biopsy and clinical presentation can include congenital hypotonia, muscle weakness, delayed motor milestones, feeding difficulties, and facial muscle involvement (1). Serum creatine kinase may be normal or elevated. Heterogeneity in presenting symptoms can occur even amongst affected members of the same family. Congenital myopathies can be divided into three main clinicopathological defined categories: nemaline myopathy, core myopathy and centronuclear myopathy (2). Nemaline Myopathy Nemaline Myopathy is characterized by weakness, hypotonia and depressed or absent deep tendon reflexes. Weakness is typically proximal, diffuse or selective, with or without facial weakness and the diagnostic hallmark is the presence of distinct rod-like inclusions in the sarcoplasm of skeletal muscle fibers (3). Core Myopathy Core Myopathy is characterized by areas lacking histochemical oxidative and glycolytic enzymatic activity on histopathological exam (2). Symptoms include proximal muscle weakness with onset either congenitally or in early childhood. Bulbar and facial weakness may also be present. Patients with core myopathy are typically subclassified as either having central core disease or multiminicore disease. Centronuclear Myopathy Centronuclear Myopathy (CNM) is a rare muscle disease associated with non-progressive or slowly progressive muscle weakness that can develop from infancy to adulthood (4, 5). -

Genetic Neuromuscular Disease *
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.73.suppl_2.ii12 on 1 December 2002. Downloaded from GENETIC NEUROMUSCULAR DISEASE Mary M Reilly, Michael G Hanna ii12* J Neurol Neurosurg Psychiatry 2002;73(Suppl II):ii12–ii21 he clinical practice of neuromuscular disease is currently undergoing enormous change as a direct result of the wealth of recent molecular genetic discoveries. Indeed, the majority of gene Tdiscoveries in the area of neurological disease relate to neuromuscular disorders. The immedi- ate impact of these discoveries is that a precise DNA based diagnosis is possible. This often gives patients accurate prognostic and genetic counselling information. It will also facilitate rational screening programmes for recognised complications such as cardiac or respiratory involvement. Unfortunately, at present many eligible patients do not benefit from or have access to such diagnostic precision, although this is changing. The discovery of new genes and proteins has opened up unexplored avenues of research into therapies for neuromuscular patients. While therapeutic trials in genetic neuromuscular diseases remain in their infancy, it seems clear that a precise DNA based diagnosis will be essential. Eligi- bility for such trials and indeed for future proven therapies will be contingent upon DNA based diagnosis. For example, it is no longer acceptable to make “limb-girdle muscular dystrophy” based on simple histochemistry, a final diagnosis. Detailed immunocytochemistry and protein chemistry in combination with DNA analysis offer the patient the best chance of a precise diagnosis from which accurate prognostication, screening, and genetic counselling will follow. In this review we describe some of the more common genetic nerve and muscle diseases encountered by adult neurologists. -

Blueprint Genetics Comprehensive Muscular Dystrophy / Myopathy Panel
Comprehensive Muscular Dystrophy / Myopathy Panel Test code: NE0701 Is a 125 gene panel that includes assessment of non-coding variants. In addition, it also includes the maternally inherited mitochondrial genome. Is ideal for patients with distal myopathy or a clinical suspicion of muscular dystrophy. Includes the smaller Nemaline Myopathy Panel, LGMD and Congenital Muscular Dystrophy Panel, Emery-Dreifuss Muscular Dystrophy Panel and Collagen Type VI-Related Disorders Panel. About Comprehensive Muscular Dystrophy / Myopathy Muscular dystrophies and myopathies are a complex group of neuromuscular or musculoskeletal disorders that typically result in progressive muscle weakness. The age of onset, affected muscle groups and additional symptoms depend on the type of the disease. Limb girdle muscular dystrophy (LGMD) is a group of disorders with atrophy and weakness of proximal limb girdle muscles, typically sparing the heart and bulbar muscles. However, cardiac and respiratory impairment may be observed in certain forms of LGMD. In congenital muscular dystrophy (CMD), the onset of muscle weakness typically presents in the newborn period or early infancy. Clinical severity, age of onset, and disease progression are highly variable among the different forms of LGMD/CMD. Phenotypes overlap both within CMD subtypes and among the congenital muscular dystrophies, congenital myopathies, and LGMDs. Emery-Dreifuss muscular dystrophy (EDMD) is a condition that affects mainly skeletal muscle and heart. Usually it presents in early childhood with contractures, which restrict the movement of certain joints – most often elbows, ankles, and neck. Most patients also experience slowly progressive muscle weakness and wasting, beginning with the upper arm and lower leg muscles and progressing to shoulders and hips. -

Muscle Channelopathies
Muscle Channelopathies Stanley Iyadurai, MSc PhD MD Assistant Professor of Neurology, Neuromuscular Specialist, OSU, Columbus, OH August 28, 2015 24 F 9 M 18 M 23 F 16 M 8/10 Occasional “Paralytic “Seizures at “Can’t Release Headaches Gait Problems Episodes” Night” Grip” Nausea Few Seconds Few Hours “Parasomnia” “Worse in Winter” Vomiting Debilitating Few Days Full Recovery Full Recovery Video EEG Exercise – Light- Worse Sound- 1-2x/month 1-2x/year Pelvic Red Lobster Thrusting 1-2x/day 3-4/year Dad? Dad? 1-2x/year Dad? Sister Normal Exam Normal Exam Normal Exam Normal Exam Hyporeflexia Normal Exam “Defined Muscles” Photophobia Hyper-reflexia Phonophobia Migraines Episodic Ataxia Hypo Per Paralysis ADNFLE PMC CHANNELOPATHIES DEFINITION Channelopathy: a disease caused by dysfunction of ion channels; either inherited (Mendelian) or acquired/complex (Non-Mendelian, e.g., autoimmune), presenting either in neurologic or non-neurologic fashion CHANNELOPATHY SPECTRUM CHARACTERISTICS Paroxysmal Episodic Intermittent/Fluctuating Bouts/Attacks Between Attacks Patients are Usually Completely Normal Triggers – Hunger, Fatigue, Emotions, Stress, Exercise, Diet, Temperature, or Hormones Muscle Myotonic Disorders Periodic Paralysis MUSCLE CHANNELOPATHIES Malignant Hyperthermia CNS Migraine Episodic Ataxia Generalized Epilepsy with Febrile Seizures Plus Hereditary & Peripheral nerve Acquired Erythromelalgia Congenital Insensitivity to Pain Neuromyotonia NMJ Congenital Myasthenic Syndromes Myasthenia Gravis Lambert-Eaton MS Cardiac Congenital -

Myopathy Five New Things
Myopathy Five New Things Published with permission from Björn Oskarsson, MD BY BJÖRN OSKARSSON, MD have been made. Also, while the term myositis is often used interchangeably with myopathy in both clinical his brief review touches on 5 relatively practice and in the literature, in this review the term new things that ought to be useful for myositis will be used exclusively for the inflammatory neurologists in general practices. The myopathies. It is important to be aware that the term chosen topics include common condi- often is used to refer to all myopathies, inflammatory or tions, techniques that are rapidly not, and that it can not be taken to imply an inflamma- Tgrowing in utilization, and new developments that tory etiology. mandate new paradigms of treatment. Furthermore, all topics have had important developments in the last 5 TOXIC STATIN MYOPATHIES Statin drugs are years. The first section discusses the very common my- being used more and more frequently, with up to algias, myopathies, and rare rhabdomyolysis occurring 29.7 million people using them in the United States with statin use. Next, the recently established necrotiz- and with $19.7 billion US dollars being spent on ing myopathy associated with statins is described. The outpatient statin prescriptions in 2005.1 Neurolo- third topic is muscle imaging with MRI and ultra- gists are also frequently prescribing statins because sound, which are techniques used in conjunction with they are effective drugs for stroke prevention. Muscle neuromuscular examination, EMG, and muscle biop- complaints are common in statin users, occurring in sies, all of which remain the mainstay of diagnostic more than 10% of this population.2 There are mil- studies for muscle disease. -

Muscle Fibrillin Deficiency in Marfan's Syndrome Myopathy
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.74.5.633 on 1 May 2003. Downloaded from 633 PAPER Muscle fibrillin deficiency in Marfan’s syndrome myopathy W M H Behan, C Longman,RKHPetty, P Comeglio, A H Child, M Boxer, P Foskett, D G F Harriman ............................................................................................................................. J Neurol Neurosurg Psychiatry 2003;74:633–639 See end of article for authors’ affiliations Objective: To report a family with Marfan’s syndrome in whom a myopathy was associated with res- ....................... piratory failure; muscle biopsies from affected individuals were examined to determine whether there Correspondence to: were abnormalities in fibrillin. ProfessorWMHBehan, Methods: 21 family members underwent detailed clinical examination, including neurological and Department of Pathology, pulmonary assessment. Muscle biopsies in the most severely affected cases were immunostained using Western Infirmary, monoclonal antibodies to specific fibrillin components. Genomic DNA from all 21 members was ana- Glasgow G11 6NT, UK; lysed for mutations in the fibrillin gene, FBN1, on 15q21. [email protected] Results: 13 individuals had a C4621T base change in exon 37 of the FBN1 gene, which in four cases Received 29 August 2002 segregated with muscle weakness or evidence of respiratory muscle dysfunction or both. Their muscle In revised form biopsies revealed an abnormality in fibrillin immunoreactivity. 10 December 2002 Accepted Conclusions: Abnormalities in fibrillin can be detected in muscle biopsies from patients with Marfan’s 11 December 2002 syndrome who have myopathy. This pedigree, with a point mutation in FBN1, also draws attention to ....................... the potential for respiratory failure associated with myopathy. arfan’s syndrome is the commonest autosomal domi- and abnormal fibrillin immunoreactivity in the endomysium nant inherited disorder of connective tissue, with a and perimysium.