Acute Empyema. the Primary Cause of Acute Empyema Is Seldom from Without; It Is Almost from Within the and to Such Conditions As
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical and Surgical Management of Empyema
361 Medical and Surgical Management of Empyema Mark S. Godfrey, MD1 Kyle T. Bramley, MD1 Frank Detterbeck, MD2 1 Pulmonary, Critical Care and Sleep Medicine, Yale New Haven Address for correspondence Frank Detterbeck, MD, 330 Cedar Street, Hospital, New Haven, Connecticut P.O. Box 208062, New Haven, CT 06520 2 Section of Thoracic Surgery, Yale University School of Medicine, (e-mail: [email protected]). New Haven, Connecticut Semin Respir Crit Care Med 2019;40:361–374. Abstract Infection of the pleural space is an ancient and common clinical problem, the incidence which is on the rise. Advances in therapy now present clinicians of varying disciplines with an array of therapeutic options ranging from thoracentesis and chest tube drainage (with or without intrapleural fibrinolytic therapies) to video-assisted thoracic surgery (VATS) or thoracotomy. A framework is provided to guide decision making, which involves weighing multiple factors (clinical history and presentation, imaging characteristics, comorbidities); Keywords multidisciplinary collaboration and active management are needed as the clinical course ► empyema over a few days determines subsequent refinement. The initial choice of antibiotics depends ► pleural infection on whether the empyema is community-acquired or nosocomial, and clinicians must ► tissue plasminogen recognize that culture results often do not reflect the full disease process. Antibiotics alone activator are rarely successful and can be justified only in specific circumstances. Early drainage with ► deoxyribonuclease or without intrapleural fibrinolytics is usually required. This is successful in most patients; ► thoracoscopy however, when surgical decortication is needed, clear benefit and low physiologic impact ► video-assisted are more likely with early intervention, expeditious escalation of interventions, and care at a thoracic surgery center experienced with VATS. -

Empyema and Ruptured Lung Abscess in Adults'
Thorax: first published as 10.1136/thx.19.6.492 on 1 November 1964. Downloaded from Thorax (1964), 19, 492. Empyema and ruptured lung abscess in adults' ROWAN NICKS From the Thoracic Surgical Unit, Page Chest Pavilion, Royal Prince Alfred Hospital, Melbourne This brief annotation concerns 18 adult patients TABLE II with empyema complicating the rupture of a lung RESULTS OF TREATMENT abscess into the pleural cavity who were referred to my service during the period 1957 to 1962. No. Cure No Cure Medical treatment By different methods of treatment all these Antibiotics .. 18 patients have been returned to health, but in some Primary surgical treatment earlier cases the illness was painful and prolonged Drainage: Infected .9 2 7 and multiple operations were necessary to attain Sterile. I a final cure. Primary decortication These are compared with patients treated Non-infected 5 5 recently in whom convalescence has been rapid, Infected .. 2 I I uncomplicated, and without loss of tissue. Primary pleuro-resection .. 1 Total .. .. 18 10 8 CLINICAL MATERIAL Particulars relevant to the treatment of 18 patients A cure followed simple drainage in three copyright. of comprising the series are summarized in Table I. 10 patients. Five sterile cases treated by primary decortica- TABLE I tion were cured, and, of two infected cases, one EMPYEMA COMPLICATING INTRAPLEURAL RUPTURE OF recurred. LUNG ABSCESS IN ADULTS, 1957 TO 1962 In the one with a localized empyema treated Total no. of cases 18 by pleurolobectomy and thoracoplasty, a curehttp://thorax.bmj.com/ Died. 0 resulted. Final cure .. .. .. 18 Primary surgery failed to achieve a cure in eight Culture: Sterile. -

Medical and Surgical Management of Empyema
361 Medical and Surgical Management of Empyema Mark S. Godfrey, MD1 Kyle T. Bramley, MD1 Frank Detterbeck, MD2 1 Pulmonary, Critical Care and Sleep Medicine, Yale New Haven Address for correspondence Frank Detterbeck, MD, 330 Cedar Street, Hospital, New Haven, Connecticut P.O. Box 208062, New Haven, CT 06520 2 Section of Thoracic Surgery, Yale University School of Medicine, (e-mail: [email protected]). New Haven, Connecticut Semin Respir Crit Care Med 2019;40:361–374. Abstract Infection of the pleural space is an ancient and common clinical problem, the incidence which is on the rise. Advances in therapy now present clinicians of varying disciplines with an array of therapeutic options ranging from thoracentesis and chest tube drainage (with or without intrapleural fibrinolytic therapies) to video-assisted thoracic surgery (VATS) or thoracotomy. A framework is provided to guide decision making, which involves weighing multiple factors (clinical history and presentation, imaging characteristics, comorbidities); Keywords multidisciplinary collaboration and active management are needed as the clinical course ► empyema over a few days determines subsequent refinement. The initial choice of antibiotics depends ► pleural infection on whether the empyema is community-acquired or nosocomial, and clinicians must ► tissue plasminogen recognize that culture results often do not reflect the full disease process. Antibiotics alone activator are rarely successful and can be justified only in specific circumstances. Early drainage with ► deoxyribonuclease or without intrapleural fibrinolytics is usually required. This is successful in most patients; ► thoracoscopy however, when surgical decortication is needed, clear benefit and low physiologic impact ► video-assisted are more likely with early intervention, expeditious escalation of interventions, and care at a thoracic surgery center experienced with VATS. -
Pneumonectomy for Empyema
7 Review Article Page 1 of 7 Pneumonectomy for empyema Marko Kostic1, Jean-Marc Baste2 1Serbia and Montenegro, Clinic for Thoracic Surgery, Clinical Centre of Serbia, Belgrade, Serbia; 2Department of General and Thoracic Surgery, UNIROUEN, Inserm U1096, Rouen University Hopsital, Normandie University, Rouen, France Contributions: (I) Conception and design: All authors; (II) Administrative support: All authors; (III) Provision of study material or patients: All authors; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Marko Kostic. Serbia and Montenegro, Clinic for Thoracic Surgery, Clinical Centre of Serbia, Belgrade, Serbia. Email: [email protected]. Abstract: Pneumonectomy for chronic lung infections and consecutive empyema has been averted because of the potential intraoperative and postoperative complications. In this analysis we have evaluated 10 prominent articles targeting mortality and morbidity outcome. Mortality rate were from 1.2–24.6% and morbidity were from 11.9–53%. Complications like postoperative empyema, bronchopleural fistula (BF) and postoperative bleeding affects the prognosis, also technique and operative duration. The surgical technique is of the paramount significance to reduce postoperative morbidity and mortality in this high risk operation. Pneumonectomy for empyema should be left to be a treatment alternative only for carefully selected patients. Keywords: Morbidity; mortality; pneumonectomy; empyema Received: 17 March 2020; Accepted: 04 June 2020; Published: 10 April 2021. doi: 10.21037/shc-20-62 View this article at: http://dx.doi.org/10.21037/shc-20-62 Introduction pneumonectomy. This sort of surgery made great progress with endotracheal mechanical ventilation. -
Fundamentals of Surgery University of Tennessee Medical Center at Knoxville Department of Surgery
Fundamentals of Surgery University of Tennessee Medical Center at Knoxville Department of Surgery Gallbladder and the Extrahepatic Biliary System ANATOMY The Gallbladder z The gallbladder is a pear-shaped sac, about 7 to 10 cm long with an average capacity of 30 to 50 mL z Same peritoneal lining covers the liver covers the fundus and the inferior surface of the gallbladder. z Lined by a single, highly-folded, tall columnar epithelium that contains cholesterol and fat globules. z The epithelial lining of the gallbladder is supported by a lamina propria. z The muscle layer has circular longitudinal and oblique fibers, but without well-developed layers. z The cystic artery that supplies the gallbladder is usually a branch of the right hepatic artery The Bile Ducts z The left hepatic duct is longer than the right and has a greater propensity for dilatation as a consequence of distal obstruction z The segment of the cystic duct adjacent to the gallbladder neck bears a variable number of mucosal folds called the spiral valves of Heister. z The common bile duct is about 7 to 11 cm in length and 5 to 10 mm in diameter. z The arterial supply to the bile ducts is derived from the gastroduodenal and the right hepatic arteries, with major trunks running along the medial and lateral walls of the common duct Anomalies z Small ducts (of Luschka) may drain directly from the liver into the body of the gallbladder. z In about 20% of patients the right hepatic artery comes off the superior mesenteric artery PHYSIOLOGY Bile Formation and Composition z Normal adult consuming an average diet produces within the liver 500 to 1000 mL of bile a day. -

Parapneumonic Pleural Effusion and Empyema
Thematic Review Series 2008 Respiration 2008;75:241–250 DOI: 10.1159/000117172 Parapneumonic Pleural Effusion and Empyema Coenraad F.N. Koegelenberga Andreas H. Diaconb Chris T. Bolligera a b Division of Pulmonology, Department of Medicine, Division of Medical Physiology, Department of Biomedical Sciences, University of Stellenbosch and Tygerberg Academic Hospital, Cape Town , South Africa Key Words tween tube thoracostomy (with or without fibrinolytics) and -Parapneumonic pleural effusion ؒ Empyema ؒ Fibrinolytics ؒ thoracoscopy. Open surgical intervention is sometimes re -Thoracoscopy ؒ Thoracotomy ؒ Thoracostomy quired to control pleural sepsis or to restore chest mechan ics. This review gives an overview of parapneumonic effu- sion and empyema, focusing on recent developments and Abstract controversies. Copyright © 2008 S. Karger AG, Basel At least 40% of all patients with pneumonia will have an as- sociated pleural effusion, although a minority will require an intervention for a complicated parapneumonic effusion or empyema. All patients require medical management with Introduction and Definitions antibiotics. Empyema and large or loculated effusions need to be formally drained, as well as parapneumonic effusions At least 40% of all patients diagnosed with pneumonia with a pH ! 7.20, glucose ! 3.4 mmol/l (60 mg/dl) or positive will have an associated pleural effusion, although the mi- microbial stain and/or culture. Drainage is most frequently nority of these will require active intervention [1, 2] . A achieved with tube thoracostomy. The use of fibrinolytics parapneumonic pleural effusion refers to any effusion remains controversial, although evidence suggests a role for secondary to pneumonia or lung abscess [1] . It becomes the early use in complicated, loculated parapneumonic effu- ‘complicated’ when an invasive procedure is necessary sions and empyema, particularly in poor surgical candidates for its resolution, or if bacteria can be cultured from the and in centres with inadequate surgical facilities. -

Part IL a Clinical Study
148 W. S. Hwang Gut: first published as 10.1136/gut.11.2.148 on 1 February 1970. Downloaded from References Chou, S. T., and Gibson, J. B. (1968). Experimental cholangitis Leong, H. K. (1959). Opium addiction in Singapore. Dissertation and cholelithiasis. Brit. J. exp. Path., 49, 565-573. for Diploma in Public Health. London School of Hygiene Cleland, J. B. (1953). Gallstones in 7,000 postmortem exam- and Tropical Medicine. inations. Med. J. Aust., 2, 488-489. Lieber, M. M. (1952). The incidence of gallstones and their cor- Cobo, A., Hall, R. C., Torres, E., and Cuello, C. J. (1964). relation with other diseases. Ann. Surg., 135, 394-405. Intrahepatic calculi. Arch. Surg., 89, 936-941. Maki, T. (1961). Cholelithiasis in the Japanese. Arch. Surg., 82, Cook, J., Hou, P. C., Ho, H. C., and McFadzean, A. J. S. (1954). 599-612. Recurrent pyogenic cholangeitis. Brit. J. Surg., 42, 188-203. Muir, C. S. (1964). Demography and age-sex distribution of the Digby, K. H. (1930). Common-duct stones of liver origin. Brit. autopsy populations of multiracial Singapore. Singapore J. Surg., 17, 578-591. med. J., 5, 96-104. Dineen, P. (1964). The importance of the route of infection in Newman, H. F., and Northrup, J. D. (1959). The autopsy experimental biliarytract obstruction. Surg. Gynec. Obstet., incidence of gallstones. Int. Abstr. Surg., 109, 1-13. 119, 1001-1008. Ong, G. B. (1962). A study of recurrent pyogenic cholangitis. Flemma, R. J. F., Flint, L. M., Osterhout, S., and Shingleton, Arch. Surg., 84,199-225. W. W. (1967). Bacteriologic studies ofbiliarytract infection. -

Management of Parapneumonic Effusions in Pediatrics: Current Practice
REVIEW Management of Parapneumonic Effusions in Pediatrics: Current Practice Sarah C. McBride, MD Pneumonia with associated complex pleural disease is a cause of significant mor- bidity among hospitalized children. The management of this patient population Children’s Hospital Boston, Harvard Medical continues to be a challenge and varies even among single institutions. The article School, Boston, Massachusetts. presented here reviews the management goals for pediatric patients hospitalized with complex parapneumonic effusions and provides updated summaries of both medical and surgical therapies. Journal of Hospital Medicine 2008;3:263–270. VC 2008 Society of Hospital Medicine. KEYWORDS: pediatrics, pneumonia, effusion, management guidelines. neumonia complicated by lung necrosis and pleural disease P consisting of parapneumonic effusion or empyema is a cause of significant morbidity among pediatric inpatients. Current practice in caring for these patients is highly variable, even within single institutions. Medical management of hospitalized children with complex pneumonias includes an attempt to iso- late the offending organism, tailored antibiotic therapy, and ade- quate pain management in association with pleural catheter drainage of large effusions. Thrombolytic agents are frequently trialed in an attempt to lyse loculated effusions without surgical intervention. Surgical drainage or decortication of walled-off infections is employed when there is poor response to more conservative treatment with pleural catheter drainage. The major therapeutic goal for this patient population is promotion of clin- ical recovery despite residual pleural abnormality at time of hos- pital discharge, with the knowledge that complete disease resolution is almost universal. Variability in management as well as unpredictable patient response to differing therapeutic modalities has hindered the de- velopment of clear practice guidelines. -

Respiratory Therapy in Pleural Empyema: a Systematic Review Of
Fisioterapia respiratória no empiema pleural. Revisão sistemática da literatura 551 Artigo de Revisão Fisioterapia respiratória no empiema pleural. Revisão sistemática da literatura* Respiratory therapy in pleural empyema. A systematic review of the literature MURILO CARLOS AMORIM DE BRITTO1, MARIA DO CARMO MENEZES BEZERRA DUARTE2, SILVIA MARIA MENDES DA CONCEIÇÃO SILVESTRE3 RESUMO Alguns dos recursos utilizados em fisioterapia respiratória não são baseados em evidências científicas comprovadas. A má utilização desses recursos pode ser nociva do ponto de vista de efeitos adversos, ou levar a um custo-benefício não favorável. Os autores fizeram uma revisão sistemática da literatura, através das bases de dados Oldmedline, Medline, Cinahl, Lilacs, e nos registros de ensaios clínicos da Biblioteca Cochrane e do National Institutes of Health, dos EUA, visando a encontrar ensaios sobre a eficácia da fisioterapia respiratória no empiema pleural em crianças, adolescentes ou adultos. Nenhum ensaio sobre o assunto foi encontrado. Os autores concluem que faltam evidências sobre a eficácia da fisioterapia no empiema pleural. Ensaios clínicos são necessários para responder a esta questão. Descritores: Empiema pleural/reabilitação; Medicina baseada em evidências; Técnicas de fisioterapia; Revisão [Tipo de publicação]; Ensaios controlados aleatórios ABSTRACT Some techniques used in respiratory therapy are not based on sound scientific evidence. The misuse of such techniques can be harmful in terms of adverse effects and may not be cost-effective. A systematic review of the literature was performed using the Oldmedline, Medline, Cinahl and Lilacs databases, as well as the registry of clinical trials registered by the Cochrane Library and National Institutes of Health. The focus of the review was on trials addressing the efficacy of respiratory therapy in treating pleural empyema in children, adolescents and adults. -

Empyema Thoracis: New Insights Into an Old Disease
Eur Respir Rev 2010; 19: 117, 220–228 DOI: 10.1183/09059180.00005610 CopyrightßERS 2010 REVIEW: ENDOSCOPY Empyema thoracis: new insights into an old disease F.J.H. Brims*,#, S.M. Lansley", G.W. Waterer" and Y.C.G. Lee#," ABSTRACT: Pleural infection is a disease of historical importance and is still a modern menace, AFFILIATIONS with incidences rising in adults and children, and a significant mortality in adults. Basic research is *Respiratory Dept, Portsmouth Hospitals NHS Trust, Portsmouth, hampered by limitations with in vivo models, and the bacteriology of empyema is complex. The role UK. of thoracic ultrasound in guiding investigation and drainage of empyema is clear. Prompt treatment #Respiratory Dept, Sir Charles with appropriate systemic antibiotics and chest tube drainage are the key; in cases of failure of Gairdner Hospital, Perth, and " these measures, thoracic surgery is of proven efficacy in the treatment of this age-old disease. School of Medicine and Pharmacology and Lung Institute of Western Australia, University of KEYWORDS: Empyema, infection, mesothelial, pleural, pneumonia Western Australia, Perth, Australia. CORRESPONDENCE leural infection is one of the oldest and Pleural infection can also complicate thoracic Y.C.G. Lee severest diseases. Drainage of the pleural (open or closed) trauma and iatrogenic proce- University Dept of Medicine, 4/F, G Block cavity was attempted by Hippocrates over dures, such as surgery (especially lung resection) P QE II Medical Center 2,000 years ago to treat empyema. During the or oesophageal rupture. ‘‘Spontaneous’’ bacterial Perth influenza pandemic of 1917–1919, closed pleural empyema is rare. It is possible that genetic pre- WA 6009 drainage became widely practiced to treat post- disposition contributes to development of empy- Australia pneumonic empyema [1]. -
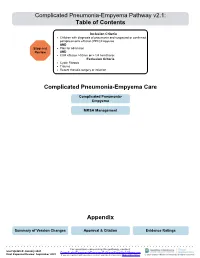
Complicated Pneumonia-Empyema Pathway V2.1: Table of Contents
Complicated Pneumonia-Empyema Pathway v2.1: Table of Contents Inclusion Criteria · Children with diagnosis of pneumonia and suspected or confirmed parapneumonic effusion (PPE)/Empyema AND Stop and · Plan for admission Review AND · CXR effusion >10mm or > 1/4 hemithorax Exclusion Criteria · Cystic Fibrosis · Trauma · Recent thoracic surgery or infection Complicated Pneumonia-Empyema Care Complicated Pneumonia- Empyema MRSA Management Appendix Summary of Version Changes Approval & Citation Evidence Ratings For questions concerning this pathway, contact: Last Updated: January 2021 [email protected] Next Expected Review: September 2023 If you are a patient with questions contact your medical provider, Medical Disclaimer © 2021 Seattle Children’s Hospital, all rights reserved Complicated Pneumonia-Empyema Pathway v2.1 Inclusion Criteria · Children with diagnosis of pneumonia and suspected or confirmed parapneumonic effusion (PPE)/Empyema AND Stop and · Plan for admission AND Review · CXR effusion >10mm or > 1/4 hemithorax Exclusion Criteria Antibiotic Selection: · Cystic Fibrosis Management of MRSA coverage · Trauma among empyema patients · Recent thoracic surgery or infection First Line: · Ceftriaxone AND Clindamycin · If suspect Clindamycin- Initial Work-Up resistant MRSA or critically ill, · Blood Culture, CBC w diff, CRP, Coags, PIV, then substitute Vancomycin for Chest US and start appropriate IV Antibiotics Clindamycin · Consult Pulmonary, General Surgery, and · If allergic to Ceftriaxone, then Infectious -

Lung Abscess Predicts the Surgical Outcome in Patients with Pleural
Huang et al. Journal of Cardiothoracic Surgery 2010, 5:88 http://www.cardiothoracicsurgery.org/content/5/1/88 RESEARCH ARTICLE Open Access Lung abscess predicts the surgical outcome in patients with pleural empyema Hung-Che Huang1, Heng-Chung Chen1, Hsin-Yuan Fang2*, Yi-Chieh Lin1, Chin-Yen Wu1, Ching-Yuan Cheng1 Abstract Objectives: Most cases of pleural empyema are caused by pulmonary infections, which are usually combined with pneumonia or lung abscess. The mortality of patients with pleural empyema remains high (up to 20%). It also contributes to higher hospital costs and longer hospital stays. We studied pleural empyema with combined lung abscess to determine if abscess was associated with mortality. Methods: From January 2004 to December 2006, we retrospectively reviewed 259 patients diagnosed with pleural empyema who received thoracscopic decortications of the pleura in a single medical center. We evaluated their clinical data and analyzed their chest computed tomography scans. Outcomes of pleural empyema were compared between groups with and without lung abscess. Results: Twenty-two pleural empyema patients had lung abscesses. Clinical data showed significantly higher incidences in the lung abscess group of pre-operative leukocytosis, need for an intensive care unit stay and mortality. Conclusion: Patients with pleural empyema and lung abscess have higher intensive care unit admission rate, higher mortality during 30 days and overall mortality than patients with pleural empyema. The odds ratio of lung abscess is 4.685. Physician shall pay more attention on high risk patient of lung abscess for early detection and management. Background clinical courses of patients with parapneumonic effu- Pleural empyema is one of the serious complications of sions or pleural empyema are varied.