California Law Enforcement I I I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Teaching Social Issues with Film
Teaching Social Issues with Film Teaching Social Issues with Film William Benedict Russell III University of Central Florida INFORMATION AGE PUBLISHING, INC. Charlotte, NC • www.infoagepub.com Library of Congress Cataloging-in-Publication Data Russell, William B. Teaching social issues with film / William Benedict Russell. p. cm. Includes bibliographical references and index. ISBN 978-1-60752-116-7 (pbk.) -- ISBN 978-1-60752-117-4 (hardcover) 1. Social sciences--Study and teaching (Secondary)--Audio-visual aids. 2. Social sciences--Study and teaching (Secondary)--Research. 3. Motion pictures in education. I. Title. H62.2.R86 2009 361.0071’2--dc22 2009024393 Copyright © 2009 Information Age Publishing Inc. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, microfilming, recording or otherwise, without written permission from the publisher. Printed in the United States of America Contents Preface and Overview .......................................................................xiii Acknowledgments ............................................................................. xvii 1 Teaching with Film ................................................................................ 1 The Russell Model for Using Film ..................................................... 2 2 Legal Issues ............................................................................................ 7 3 Teaching Social Issues with Film -

Why Hollywood Isn't As Liberal As We Think and Why It Matters
Claremont Colleges Scholarship @ Claremont CMC Senior Theses CMC Student Scholarship 2019 Why Hollywood Isn't As Liberal As We Think nda Why It Matters Amanda Daily Claremont McKenna College Recommended Citation Daily, Amanda, "Why Hollywood Isn't As Liberal As We Think nda Why It Matters" (2019). CMC Senior Theses. 2230. https://scholarship.claremont.edu/cmc_theses/2230 This Open Access Senior Thesis is brought to you by Scholarship@Claremont. It has been accepted for inclusion in this collection by an authorized administrator. For more information, please contact [email protected]. 1 Claremont McKenna College Why Hollywood Isn’t As Liberal As We Think And Why It Matters Submitted to Professor Jon Shields by Amanda Daily for Senior Thesis Fall 2018 and Spring 2019 April 29, 2019 2 3 Abstract Hollywood has long had a reputation as a liberal institution. Especially in 2019, it is viewed as a highly polarized sector of society sometimes hostile to those on the right side of the aisle. But just because the majority of those who work in Hollywood are liberal, that doesn’t necessarily mean our entertainment follows suit. I argue in my thesis that entertainment in Hollywood is far less partisan than people think it is and moreover, that our entertainment represents plenty of conservative themes and ideas. In doing so, I look at a combination of markets and artistic demands that restrain the politics of those in the entertainment industry and even create space for more conservative productions. Although normally art and markets are thought to be in tension with one another, in this case, they conspire to make our entertainment less one-sided politically. -

2010 Annual Report
2010 ANNUAL REPORT Table of Contents Letter from the President & CEO ......................................................................................................................5 About The Paley Center for Media ................................................................................................................... 7 Board Lists Board of Trustees ........................................................................................................................................8 Los Angeles Board of Governors ................................................................................................................ 10 Media Council Board of Governors ..............................................................................................................12 Public Programs Media As Community Events ......................................................................................................................14 INSIDEMEDIA Events .................................................................................................................................14 PALEYDOCFEST ......................................................................................................................................20 PALEYFEST: Fall TV Preview Parties ...........................................................................................................21 PALEYFEST: William S. Paley Television Festival ......................................................................................... 22 Robert M. -

Honor Roll 2006
i annual report Jennifer Rodriquez, age 3 gifts Childrens hospiTal los angeles honor roll of donors for the time period of January 1, 2006, through December 31, 2006 in gratitude and recognition The patients, families, staff and Board of Trustees of Childrens Hospital Los Angeles are grateful to the many people who help us build for the future and provide clinical care, research and medical education through their financial support. We recognize esteemed individuals, organizations, corporations and foundations for their generosity during the 2006 calendar year. This Honor Roll lists donors who contributed at least $1,000 in cash gifts, pledges or pledge payments. To view the Red Wagon Society Honor Roll of Donors, which lists gifts of $150 to $999, please visit the electronic version of the Honor Roll at www.ChildrensHospitalLA.org/honorroll2006.pdf. Foregoing individual recognition, we also extend thanks to those who made generous contribu- tions directly to one of our Associate and Affiliate, or allied groups. Children’s Miracle Network (CMN) gifts to CMN National will be recognized in the next issue of Imagine. In spite of our best efforts, errors and omissions may occur. Please inform us of any inaccuracies by contacting Marie Logan, director of Donor Relations, at (323) 671-1733, or [email protected]. • | imagine spring 07 $10,000,000 and above The Sharon D. Lund Foundation Confidence Foundation Randy and Erika Jackson Anonymous Friend The Harold McAlister Charitable Corday Foundation Foundation i Foundation Kenneth and Sherry Corday Johnson & Johnson $4,000,000 to $9,999,999 Mrs. J. Thomas McCarthy Mr. -

DVD Profiler
101 Dalmatians II: Patch's London Adventure Animation Family Comedy2003 74 minG Coll.# 1 C Barry Bostwick, Jason Alexander, The endearing tale of Disney's animated classic '101 Dalmatians' continues in the delightful, all-new movie, '101 Dalmatians II: Patch's London A Martin Short, Bobby Lockwood, Adventure'. It's a fun-filled adventure fresh with irresistible original music and loveable new characters, voiced by Jason Alexander, Martin Short and S Susan Blakeslee, Samuel West, Barry Bostwick. Maurice LaMarche, Jeff Bennett, T D.Jim Kammerud P. Carolyn Bates C. W. Garrett K. SchiffM. Geoff Foster 102 Dalmatians Family 2000 100 min G Coll.# 2 C Eric Idle, Glenn Close, Gerard Get ready for outrageous fun in Disney's '102 Dalmatians'. It's a brand-new, hilarious adventure, starring the audacious Oddball, the spotless A Depardieu, Ioan Gruffudd, Alice Dalmatian puppy on a search for her rightful spots, and Waddlesworth, the wisecracking, delusional macaw who thinks he's a Rottweiler. Barking S Evans, Tim McInnerny, Ben mad, this unlikely duo leads a posse of puppies on a mission to outfox the wildly wicked, ever-scheming Cruella De Vil. Filled with chases, close Crompton, Carol MacReady, Ian calls, hilarious antics and thrilling escapes all the way from London through the streets of Paris - and a Parisian bakery - this adventure-packed tale T D.Kevin Lima P. Edward S. Feldman C. Adrian BiddleW. Dodie SmithM. David Newman 16 Blocks: Widescreen Edition Action Suspense/Thriller Drama 2005 102 min PG-13 Coll.# 390 C Bruce Willis, Mos Def, David From 'Lethal Weapon' director Richard Donner comes "a hard-to-beat thriller" (Gene Shalit, 'Today'/NBC-TV). -
![Talking Book Topics July-August 2021 [PDF]](https://docslib.b-cdn.net/cover/8250/talking-book-topics-july-august-2021-pdf-3338250.webp)
Talking Book Topics July-August 2021 [PDF]
ISSN 0039-9183 Talking Book Topics July–August 2021 Get BARD Like us on www.loc.gov/nls Need help ordering books or changing your subscription status? Your local braille and talking-book library is always the place to start. For general information and to order books, call 888-NLS-READ (888-657-7323) to be connected to the appropriate library for you. Emails and phone numbers for libraries around the country can be found on the final pages of this publication, or visit www.loc.gov/nls and select “Find Your Library.” You may also change your Talking Book Topics subscription by completing the form on the inside back cover and mail it to your local cooperating library. Get books fast from BARD About Talking Book Topics Most books and magazines listed in Talking Book Topics, published in audio, large Talking Book Topics are available to print, and online, is distributed free to people eligible readers for download on the unable to read regular print and is available NLS Braille and Audio Reading Download in an abridged form in braille. Talking Book (BARD) site. To use BARD, contact Topics lists a selection of titles recently added your local cooperating library or visit to the NLS collection. The entire collection, nlsbard.loc.gov for more information. with hundreds of thousands of titles, is The free BARD Mobile app is available available at www.loc.gov/nls. Select from the App Store, Google Play, and “Catalog Search” to view the collection. Amazon’s Appstore. Talking Book Topics is also online at www.loc.gov/nls/tbt and in downloadable Need Overseas Service? audio files from BARD. -

IN the COURT of CHANCERY of the STATE of DELAWARE R.A. FEUER, Suing Derivatively on Behalf of CBS CORPORATION, Plaintiff, V
IN THE COURT OF CHANCERY OF THE STATE OF DELAWARE R.A. FEUER, suing derivatively on ) behalf of CBS CORPORATION, ) ) Plaintiff, ) ) v. ) C.A. No. 12575-CB ) SUMNER M. REDSTONE, SHARI ) REDSTONE, DAVID ANDELMAN, ) JOSEPH A. CALIFANO, JR., ) WILLIAM S. COHEN, GARY L. ) COUNTRYMAN, CHARLES K. ) GIFFORD, LEONARD GOLDBERG, ) BRUCE S. GORDON, LINDA M. ) GRIEGO, ARNOLD KOPELSON, ) LESLIE MOONVES, DOUG ) MORRIS, and FREDERIC V. ) SALERNO, ) ) Defendants, ) ) and ) ) CBS CORPORATION, ) ) Nominal Defendant. ) MEMORANDUM OPINION Date Submitted: January 16, 2018 Date Decided: April 19, 2018 Norman M. Monhait and P. Bradford deLeeuw of ROSENTHAL MONHAIT & GODDESS, P.A., Wilmington, Delaware; Richard D. Greenfield, Marguerite R. Goodman, and Ilene Freier Brookler of GREENFIELD & GOODMAN, LLC, New York, New York; Michael D. Donovan of DONOVAN AXLER, LLC, Berwyn, PA; Counsel for Plaintiff. Kurt M. Heyman, Patricia L. Enerio, and Melissa N. Donimirski of HEYMAN ENERIO GATTUSO & HIRZEL LLP, Wilmington, Delaware; Paul Vizcarrondo, Jonathan Moses, Lauren Kofke, and Courtney Heavey of WACHTELL, LIPTON, ROSEN & KATZ, New York, New York; Counsel for Defendants David Andelman, Joseph A. Califano, Jr., William S. Cohen, Gary L. Countryman, Charles K. Gifford, Leonard Goldberg, Bruce S. Gordon, Linda M. Griego, Arnold Kopelson, Leslie Moonves, Doug Morris, and Nominal Defendant CBS Corporation. A. Thompson Bayliss, Michael A. Barlow, and David A. Seal of ABRAMS & BAYLISS LLP, Wilmington, Delaware; Michael C. Tu of ORRICK, HERRINGTON & SUTCLIFFE LLP, Los Angeles, California; Robert N. Kliger of HUESTON HENNIGAN LLP, Los Angeles, California; Counsel for Defendant Sumner M. Redstone. Anne C. Foster, Lisa A. Schmidt, and Kevin M. Gallagher of RICHARDS, LAYTON & FINGER, P.A., Wilmington, Delaware; Elizabeth B. -
Helicopter Crash Kills 1
C M Y K www.newssun.com NEWS-SUN Highlands County’s Hometown Newspaper Since 1927 Sunday, December 8, 2013 Volume 94/Number 146 | 75 cents Streaks roll Sebring cruises to win over district foe A Classic Thousands line streets of Lemon Bay Sebring to see annual parade SPORTS, B1 Christmas PHOTOS INSIDE ON A3 PAGE B12 County HELICOPTER CRASH KILLS 1 to study Witness: Crop duster nosed private dived, exploded EMS at sod farm By BARRY FOSTER News-Sun correspondent By SAMANTHA GHOLAR SEBRING – Despite a stri- [email protected] dent stand against even talk- SEBRING — A helicopter ing about the idea of privatiz- reportedly nosed-dived into the ing Highlands County’s ground at a sod farm near the Emergency Medical Services Sebring airport late Friday after- by Commissioner Jim noon, apparently killing the pilot. Brooks, the balance of the No official information had been Highlands County released as of Saturday afternoon, Commission Tuesday agreed but an eyewitness spoke to the to continue investigating the News-Sun Saturday morning near possibility. the scene of the crash site on the Brooks, a former Sod, Citrus and Cane property near Highlands County EMS coor- Sebring International Raceway. dinator himself, said he was The National Transportation not in favor of even entertain- Safety Board was probing the ing the idea. wreckage, which was near an irri- “The coun- gation pond, Saturday morning. ty is respon- Joshua Snell, an employee with sible for pro- the contracting company that helps viding EMS manage the property, said the inci- service. dent occurred around 5:20 p.m. -

DISTINGUISHED Residentsof
DISTINGUISHED 1 RESI D ENTS of Hillside Memorial Park and Mortuary DISTINGUISHED RESIDENTS IRV I NG AA RONSON (1895 – 1963) EV E RL A ST I NG Pea C E Irving Aaronson’s career began at the age of 11 as a movie theater pianist. DISTINGUISHED RE S I D E NTS GU I D E : A LE G A CY OF LE G E NDS In the 1920’s he became a Big Band leader with the Versatile Sextette and Irving Aaronson & the Commanders. The Commanders recorded “I’ll Get By,” Cole Porter’s “Let’s Misbehave,” “All By Ourselves in the Hillside Memorial Park and Mortuary has provided a place to Moonlight,” “Don’t Look at Me That Way” and “Hi-Ho the Merrio.” Irving Aaronson His band included members Gene Krupa, Claude Thornhill and Artie honor the accomplishments and legacies of the Jewish community Shaw. He later worked for MGM as a music coordinator for “Arrivederci Roma” (1957), “This Could Be the Night” (1957), “Meet Me in Las Vegas” since 1942. We have made it our mission to provide southern (1956) and as music advisor for “The Merry Widow” (1952). California with a memorial park and mortuary dedicated to ROSLYN ALF I N –SL A T E R (1916 – 2002) GA RD E N OF SA R A H honoring loved ones in a manner that is fitting and appropriate. Dr. Roslyn Alfin-Slater was a highly esteemed UCLA professor and nutrition expert. Her early work included studies on the relationship between cholesterol and essential fatty acid metabolism. -

California Teachers Association
CALIFORNIA TEACHERS ASSOCIATION Report of Board of Directors, Committees, and Items of New Business to be presented to STATE COUNCIL OF EDUCATION June 1-6, 2020 Los Angeles, California Printed by the Office Services Department of California Teachers Association OUR MISSION The California Teachers Association exists to protect and promote the well-being of its members; to improve the conditions of teaching and learning; to advance the cause of free, universal, and quality public education; to ensure that the human dignity and civil rights of all children and youth are protected; and to secure a more just, equitable, and democratic society. To fulfill its mission, the California Teachers Association pursues the following goals: I. CTA plans and executes programs and strategies designed to enhance the quality of education for students and the professional and personal lives of its members. II. CTA assists its local chapters in bargaining for salaries and individual and employment rights in keeping with the academic and professional status of its members. III. CTA represents members in governmental relations -- to influence state and federal legislation and actions by state and federal agencies. IV. CTA strengthens its role as the preeminent voice for public education in California -- projects a strong, coherent and consistent image -- such that its members play the major role in shaping public policy on education. V. CTA represents members in professional and career development matters. VI. CTA represents members and provides a program of economic benefits and resources for members. VII. CTA works to maintain and expand its membership so as to remain effective in defending and advancing its members' interests. -

Proquest Dissertations
Licensed to shill: How video and computer games tarnished the silver screen Item Type text; Dissertation-Reproduction (electronic) Authors Ruggill, Judd E. Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 30/09/2021 07:23:18 Link to Item http://hdl.handle.net/10150/280772 LICENSED TO SHILL: HOW VIDEO AND COMPUTER GAMES TARNISHED THE SILVER SCREEN by Judd Ethan Ruggill Copyright © Judd Ethan Ruggill 2005 A Dissertation Submitted to the Faculty of the GRADUATE INTERDISCIPLINARY PROGRAM IN COMPARATIVE CULTURAL AND LITERARY STUDIES In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY WITH A MAJOR IN MEDIA ARTS In the Graduate College THE UNIVERSITY OF ARIZONA 2 00 5 UMI Number: 3158216 Copyright 2005 by Ruggill, Judd Ethan All rights reserved. INFORMATION TO USERS The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleed-through, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. UMI UMI Microform 3158216 Copyright 2005 by ProQuest Information and Learning Company. All rights reserved. -
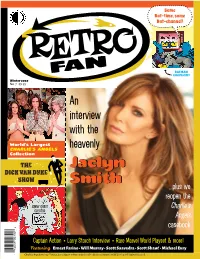
Retrofan7preview (Pdf) Download
Same Bat-time, same Bat-channel! BATMAN GOOFS OFF! Winter 2020 No. 7 $9.95 An interview with the World’s Largest CHARLIE’S ANGELS heavenly Collection THE JaclynJaclyn DICK VAN DYKE SHOW SmithSmith …plus we reopen the JONNY QUEST Charlie’s CREATOR Angels 6 casebook 0 9 3 0 0 8 Captain Action • Larry Storch Interview • Rare Marvel World Playset & more! 5 6 2 8 Featuring Ernest Farino • Will Murray • Scott Saavedra • Scott Shaw! • Michael Eury 1 Charlie's Angels © Sony Pictures. Jonny Quest © Hanna-Barbera Productions. Batman © DC Comics. All Rights Reserved. The crazy cool culture we grew up with CONTENTS Issue #7 Winter 2020 15 Columns and Special Features Departments 3 2 Retro Television Retrotorial Charlie’s Angels 20 23 15 Too Much TV Quiz Retro Interview Jaclyn Smith 23 Retro Super-Heroes 28 Captain Action Will Murray’s 20th Century 51 Panopticon 37 Jonny Quest creator Super Collector Doug Wildey Charlie’s Angels Collectibles by Jack Condon 34 Retro Interview 60 3 Larry Storch RetroFad Streaking 45 Scott Saavedra’s 63 28 Secret Sanctum Retro Toys The Not-So-Super Collector Marvel World 51 72 Ernest Farino’s Celebrity Crushes Retro Fantasmagoria The Dick Van Dyke Show 73 66 Retro Travel 66 The Land of Oz – Beech Oddball World of Scott Shaw! Mountain, North Carolina 37 Batman #183 (1966) 78 RetroFanmail 73 80 ReJECTED RetroFan fantasy cover by Scott Saavedra RetroFan™ #7, Winter 2020. Published quarterly by TwoMorrows Publishing, 10407 Bedfordtown Drive, Raleigh, NC 27614. Michael Eury, Editor-in-Chief. John Morrow, Publisher. Editorial Office: RetroFan, c/o Michael Eury, Editor-in-Chief, 112 Fairmount Way, New Bern, NC 28562.