2021 Rnai Roundtable
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
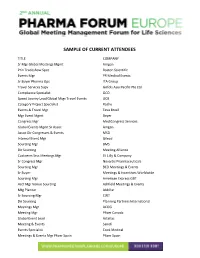
Sample of Current Attendees
SAMPLE OF CURRENT ATTENDEES TITLE COMPANY Sr Mgr Global Meetings Mgmt Amgen Prin Tradeshow Spec Boston Scientific Events Mgr PR Medical Events Sr Buyer Pharma Ops ITA Group Travel Services Supv Grifols Asia Pacific Pte Ltd Compliance Specialist GCO Spend Jouney Lead Global Mtgs Travel Events UCB Category Project Specialist Roche Events & Travel Mgr Teva Brasil Mgr Event Mgmt Bayer Congress Mgr MediCongress Services Global Events Mgmt Sr Assoc Amgen Assoc Dir Congresses & Events MSD Internal Event Mgr Gilead Sourcing Mgr BMS Dir Sourcing Meeting Alliance Custoerm Srvs Meetings Mgr Eli Lilly & Company Sr Congress Mgr Novartis Pharmaceuticals Sourcing Mgr BCD Meetings & Events Sr Buyer Meetings & Incentives Worldwide Sourcing Mgr American Express GBT Acct Mgr Venue Sourcing Ashfield Meetings & Events Mtg Planner AbbVie Sr Sourcing Mgr CWT Dir Sourcing Planning Partners International Meetings Mgr ACOG Meeting Mgr Pfizer Canada Global Event Lead Astellas Meeting & Events Sanofi Events Specialist Cook Medical Meetings & Events Mgr Pfizer Spain Pfizer Spain Sr Mgr Hotel Procurement Meetings & Incentives WorldWide Inc Event Planner SFU BCcampus Mgr Global Strategic Mtg Mgmt Teva Pharmaceuticals Global Mtgs & Events Virtual Mtgs Specialist AstraZeneca Global Congress Strategy Lead MSD Assoc Dir Congresses & Events Alnylam Pharmaceuticals Event Planner AbbVie Institutional & Scientific Events Coordr Almirall Congress Mgr AO Spine Sr Meeting Planner Medtronic Mgr Global Mtgs Mgmt Alnylam Pharmaceuticals Meeting Planner AbbVie Global Audit Meetings -

View State-Of-The-Art Clinical Symposium Disclosures
Planning Committee Members The following Planning Committee members have no relevant financial relationship(s) with ineligible companies to disclose. Mastering E/M Changes for 2021 • Antanya Chung-Gardiner, BSc • Melesia Tillman 2021 Access in Rheumatology Planning Committee • Marcus Snow, MD 2021 Fellow-in-Training Educational Session Planning Committee • Nadia Elias, MD • Tate Johnson, MD • Justin Levinson, MD, MBA • Jean Lin, MD, PhD • Megan Lockwood, MD • Tyler Reese, MD • Zahra Rehman, MD • Didem Saygin, MD • Rachel Wallwork, MD 2021 State-of-the-Art Clinical Symposium Planning Committee • Sobia Hassan, MD • Aman Kugasia, MD • Jeanie Lee, MD • Manjari Malkani, MD • Rebecca Manno, MD, MHS The following Planning Committee members have relevant financial relationship(s) with ineligible companies to disclose. 2021 Access in Rheumatology Planning Committee • Christopher Phillips, MD - Pfizer (Self): 5 2021 Fellow-in-Training Educational Session Planning Committee • Mary Mamut, DO - Bendcare (Self): 8 2021 State-of-the-Art Clinical Symposium Planning Committee • Rohit Aggarwal, MD, MS - AbbVie, Amgen, , Genzyme, , Novartis, Roche, Sandoz, UCB (Self): 1, 5, 2; AdMIRx, Inc. / Now Q-32 (Self): 5, 2; Alexion (Self): 5; Argenx (Self): 5; AstraZeneca (Self): 5; Boehringer Ingelheim (BI) (Self): 5; Bristol-Myers Squibb(BMS) (Self): 5, 2; Corbus (Self): 5; CSL Behring (Self): 1, 5; EMD Serono (Self): 5, 2; Genentech (Self): 2; Janssen (Self): 5; Kezar (Self): 5; Kyverna (Self): 5; Mallinckrodt (Self): 1, 2; Octapharma (Self): 1, 5; Orphazyme (Self): 1; Pfizer (Self): 5, 2; Scipher Medicine: 5 • Narender Annapureddy, MD, MS - Medpage (Self): 1, Expert Reviewers for the ACR Reading Room section of MedPage Today. • Lianne Gensler, MD - AbbVie (Self): 1, 5; Eli Lilly (Self): 5; Gilead: 5; GSK (Self): 5; Janssen (Self): 5; Novartis (Self): 5; Pfizer (Self): 5, 2; UCB: 5 Faculty The following Faculty members have no relevant financial relationship(s) with ineligible companies to disclose. -

Pushing the Limits: Being Innovative in a Regulated Industry
ISPE Boston Area Chapter Presents: Pushing the Limits: Being Innovative in a Regulated Industry Thursday, November 15, 2018 5:30 pm to 8:30 pm Alnylam 300 Third Street THANK YOU TO OUR PROGRAM SPONSOR Cambridge, MA 02142 EVENT INFORMATION: Join the ISPE Boston Area Chapter for an open forum on innovation. Push your own limits by participating in our pre-program activity with pharma colleagues while enjoying refreshments and a cash bar. Please have valid I. D. ready for a security checkpoint. Walk-ins are still welcome to register onsite. PROGRAM SUMMARY: Innovation comes in many forms ranging from scientific breakthroughs to new technologies and processes. This panel discussion will focus on innovation, and how it impacts the phases of the drug development lifecycle through regulatory compliance. The intent of this discussion is to allow for an interactive look into how innovation can be applied in a regulated field by providing an open forum for the moderator and audience to interact with industry leaders. If you want to better understand how to integrate innovation in your business, or the effects of innovation on your business, this panel will provide much-needed insight. By having people walking the walk of innovation from Development, Engineering, Manufacturing and Regulatory Affairs, we will be able to look to interdependencies, conflict, and synergies of innovative products. Topics will range from technical, personnel, and regulatory decisions needed to incorporate innovation into your business. WHO SHOULD ATTEND: Development, Engineering, Manufacturing, Quality Assurance and Regulatory Affairs personnel. Anybody that wants to better understand how to develop and execute teams when implementing innovative platforms or technologies. -

Human Sequencing Resource with UK Biobank
January 8, 2018 Regeneron Forms Consortium of Leading Life Sciences Companies to Accelerate Largest Widely-Available 'Big Data' Human Sequencing Resource with UK Biobank By end of 2019, Regeneron plans to sequence the exomes of all 500,000 people within the UK Biobank resource, all with associated health records, creating an unprecedented resource linking human genetic variations to human biology and disease AbbVie, Alnylam Pharmaceuticals, AstraZeneca, Biogen and Pfizer will join Regeneron to co-fund one of the industry's most ambitious 'pre-competitive' research efforts Exome sequencing data and findings will be openly available to other researchers TARRYTOWN, N.Y., Jan. 8, 2018 /PRNewswire/ -- Regeneron Pharmaceuticals, Inc. (NASDAQ: REGN), along with new collaborators AbbVie, Alnylam Pharmaceuticals, AstraZeneca, Biogen and Pfizer Inc., today announced the formation of a major 'pre-competitive' consortium to fund the generation of genetic exome sequence data from the 500,000 volunteer participants who make up the UK Biobank health resource. The newly announced collaborators will each commit $10 million to enable a dramatic acceleration of sequencing timelines, and additional companies are considering joining the consortium. Regeneron will conduct the sequencing effort. The sequencing data will be paired with detailed, de-identified medical and health records within the UK Biobank resource, including enhanced measures such as brain, heart and body imaging, to create an unparalleled resource for linking human genetic variations to human biology and disease. It was originally planned that sequencing of all 500,000 samples in the UK Biobank would be completed by 2022, with the first 50,000 people sequenced during 2017 with funding from Regeneron and GlaxoSmithKline. -

Cell and Gene Therapy Gathers Pace
Next-generation therapeutics: cell and gene therapy gathers pace At one of its most exciting phases of growth, the cell and gene therapy market has gained momentum in dealmaking, product sales and big Brain light/Alamy Stock Photo Stock Brain light/Alamy pharma interest, all of which are analyzed in this feature. feature Paul Verdin and Lisa Urquhart Therapeutic approaches employing whole cells are not new—for is substantial ongoing work in oncology, the majority of programs example, techniques based on cultured autologous epidermal cells (65%) across the combined pipeline are in non-oncology indications. for burn treatment and chondrocytes for knee cartilage repair have The value picture reveals a similar overall distribution—indications been available for more than a decade. Gene therapy and other gene outside oncology account for 76% of the 2024 forecasted sales transcription and translation-targeted approaches such as RNA inter- value, and only three oncology indications are included in the top ference (RNAi) are a much more recent addition to the therapeutic 20 indications by 2024 forecast sales (Fig. 2). The top 20 list reveals a arsenal, and coupled with the high-profile arrival of chimeric antigen wide variety of indications, including SMA, amyloidosis, hemophilia receptor (CAR)-T cells are ushering in a new era for cell-based and A and B, sickle cell disease, Huntington’s disease and amyotrophic gene-based medicine. lateral sclerosis. Logically, nucleic acid approaches are on the whole These groundbreaking scientific advances have also brought with focused on those diseases with a clearer genetic basis, whereas cell them intense debate about payment models and affordability, add- therapies are being explored in oncology and those indications with ing fuel to the broader fire raging around drug pricing. -

Rebateable Manufacturers
Rebateable Labelers – July 2021 Manufacturers are responsible for updating their eligible drugs and pricing with CMS. Montana Healthcare Programs will not pay for an NDC not updated with CMS. Note: Some manufacturers on this list may have some NDCs that are covered and others that are not. Manufacturer ID Manufacturer Name 00002 ELI LILLY AND COMPANY 00003 E.R. SQUIBB & SONS, LLC. 00004 HOFFMANN-LA ROCHE 00006 MERCK & CO., INC. 00007 GLAXOSMITHKLINE 00008 WYETH PHARMACEUTICALS LLC, 00009 PHARMACIA AND UPJOHN COMPANY LLC 00013 PFIZER LABORATORIES DIV PFIZER INC 00015 MEAD JOHNSON AND COMPANY 00023 ALLERGAN INC 00024 SANOFI-AVENTIS, US LLC 00025 PFIZER LABORATORIES DIV PFIZER INC 00026 BAYER HEALTHCARE LLC 00032 ABBVIE INC. 00037 MEDA PHARMACEUTICALS, INC. 00039 SANOFI-AVENTIS, US LLC 00046 WYETH PHARMACEUTICALS INC. 00049 ROERIG 00051 ABBVIE INC 00052 ORGANON USA INC. 00053 CSL BEHRING L.L.C. 00054 HIKMA PHARMACEUTICAL USA, INC. 00056 BRISTOL-MYERS SQUIBB PHARMA CO. 00065 ALCON LABORATORIES, INC. 00068 AVENTIS PHARMACEUTICALS 00069 PFIZER LABORATORIES DIV PFIZER INC 00071 PARKE-DAVIS DIV OF PFIZER 00074 ABBVIE INC 00075 AVENTIS PHARMACEUTICALS, INC. 00078 NOVARTIS 00085 SCHERING CORPORATION 00087 BRISTOL-MYERS SQUIBB COMPANY 00088 AVENTIS PHARMACEUTICALS 00093 TEVA PHARMACEUTICALS USA, INC. 00095 BAUSCH HEALTH US, LLC Page 1 of 19 Manufacturer ID Manufacturer Name 00096 PERSON & COVEY, INC. 00113 L. PERRIGO COMPANY 00115 IMPAX GENERICS 00116 XTTRIUM LABORATORIES, INC. 00121 PHARMACEUTICAL ASSOCIATES, INC. 00131 UCB, INC. 00132 C B FLEET COMPANY INC 00143 HIKMA PHARMACEUTICAL USA, INC. 00145 STIEFEL LABORATORIES, INC, 00168 E FOUGERA AND CO. 00169 NOVO NORDISK, INC. 00172 TEVA PHARMACEUTICALS USA, INC 00173 GLAXOSMITHKLINE 00178 MISSION PHARMACAL COMPANY 00185 EON LABS, INC. -

Current Sustaining Member Companies
CURRENT SUSTAINING MEMBER COMPANIES MEMBER FOR OVER: 10 Years 25 Years 50 Years Member Since (alphabetical order) 1976 3M Medical Solutions Division 2018 Coherus Biosciences 2019 Ipsen Biopharmaceuticals, Inc. 2011 Remund Group, LLC 1985 Abbott Laboratories, Inc. 2017 Cook Medical, LLC 2018 IT Cadre 2018 Rigel Pharmaceuticals 2013 AbbVie Inc. 2020 D2 Pharma Consulting, LLC 1989 J & J Health Care Systems, Inc. 2000 Sanofi 2021 Adaptive Biotechnologies 2007 Daiichi Sankyo, Inc. 2014 Jazz Pharmaceuticals Inc. 2020 Seattle Genetics 2017 ACADIA Pharmaceuticals, Inc. 2020 Deciphera Pharmaceuticals, LLC 2007 Karl Storz Endoscopy America 2004 Siemens Medical Solutions 2020 AcelRx Pharmaceuticals, Inc. 2009 Deloitte 2020 Lipogems 2019 SK Life Science, Inc. 2020 Acorda Therapeutics 2020 Dexcom, Inc. 2010 LLC Federal Solutions 2002 Smith & Nephew, Inc. 2019 Aimmune 2020 Drip Drop Hydration 2014 Lovell Government Services LLC 2019 Sobi Inc. 2003 Alcon Laboratories, Inc. 2017 Eagle Pharmaceuticals, Inc. 2014 Mallinckrodt Pharmaceuticals 2013 Stryker Orthopaedics 2019 Alexion Pharmaceuticals, Inc. 2005 Eisai, Inc. 2020 MannKind Corporation 2018 Sun Pharmaceutical 2017 Alkermes, Inc. 2019 electroCore, Inc. 1999 Marketing Assessment, Inc. 1999 Sunovion Pharmaceuticals, Inc. 2019 Alnylam Pharmaceuticals 2010 Endo Pharmaceuticals 2009 Masimo Corporation 2016 Taiho Oncology, Inc. 2019 Altarum Institute 2017 Exelixis 2019 Medical Strategies International, LLC 2015 Takeda Oncology 2020 Amarin Corporation 2016 Express Scripts Federal Pharmacy 2016 Melling Medical 2000 Takeda Pharmaceutical USA, Inc. 1994 AmerisourceBergen 2010 Federal Practitioner 1954 Merck & Co., Inc. 2020 Telemynd 1992 Amgen 2018 Foundation Medicine, Inc. 2002 MerzNorth America 2020 TerSera Therapeutics 2020 Amneal Pharmaceutical 2021 Frontier Technology Inc. (FTI) 2018 Mitsubishi Tanabe Pharma America 1990 Teva 2019 Aptive Resources LLC 2020 Fresenius Medical Care North America 2014 Nationwide Pharmaceutical LLC 2019 The Coalition for Government Procurement 2011 Arbor Pharmaceuticals, LLC 1989 Genentech Inc. -

Alnylam Prepares to Land First Rnai Drug Approval
NEWS & ANALYSIS Nature Reviews Drug Discovery | Published online 28 Feb 2018; doi:10.1038/nrd.2018.20 “We’ve had our near-death experiences,” concedes Maraganore. Alnylam prepares to land first Merck continued to outwardly express enthusiasm for RNAi for a few years longer, but never moved any RNAi therapies into its RNAi drug approval publicly disclosed pipeline, and eventually With Alnylam’s rare disease drug candidate patisiran nearing the regulatory sold its Sirna intellectual property (IP) to finish line, the RNA interference community is now turning its attention to once-arch-rival Alnylam in early 2014 for less next-generation delivery technology to solidify the future of the emerging modality. than a sixth of the Sirna purchase price. “I think that large companies, and large pharma in particular, really stink at Chris Morrison start-ups captured the imaginations and innovation around platforms, and we saw enthusiasm of venture capitalists and public that with RNAi,” Maraganore says. The Drug developers have been fishing in the investors, and industry’s largest companies near-death experiences that strengthened bumpy RNA interference (RNAi) waters for eventually bought into the hope and hype as Alnylam’s resolve are culturally incompatible years without a catch in sight. They probably well. Novartis committed hundreds of millions with large organizations, he argues. And so won’t have to wait much longer. In December of US dollars for access to Alnylam’s platform when early generation RNAi candidates 2017, RNAi pioneer Alnylam Pharmaceuticals in 2005, and Roche followed suit in 2007. In failed to deliver on their promise, it was finalized its regulatory submissions to the 2006, Merck & Co. -

Current Sustaining Member Companies
CURRENT SUSTAINING MEMBER COMPANIES MEMBER FOR OVER: 10 Years 25 Years 50 Years Member Since (alphabetical order) 1976 3M Medical Solutions Division 2018 Coherus Biosciences 2019 Ipsen Biopharmaceuticals, Inc. 2011 Remund Group, LLC 1985 Abbott Laboratories, Inc. 2017 Cook Medical, LLC 2018 IT Cadre 2018 Rigel Pharmaceuticals 2013 AbbVie Inc. 2020 D2 Pharma Consulting, LLC 1989 J & J Health Care Systems, Inc. 2000 Sanofi 2021 Adaptive Biotechnologies 2007 Daiichi Sankyo, Inc. 2014 Jazz Pharmaceuticals Inc. 2020 Seattle Genetics 2017 ACADIA Pharmaceuticals, Inc. 2020 Deciphera Pharmaceuticals, LLC 2007 Karl Storz Endoscopy America 2004 Siemens Medical Solutions 2020 AcelRx Pharmaceuticals, Inc. 2009 Deloitte 2021 Lantheus Holdings 2019 SK Life Science, Inc. 2020 Acorda Therapeutics 2020 Dexcom, Inc. 2020 Lipogems 2002 Smith & Nephew, Inc. 2019 Aimmune 2020 Drip Drop Hydration 2010 LLC Federal Solutions 2019 Sobi Inc. 2003 Alcon Laboratories, Inc. 2017 Eagle Pharmaceuticals, Inc. 2014 Lovell Government Services LLC 2013 Stryker Orthopaedics 2019 Alexion Pharmaceuticals, Inc. 2005 Eisai, Inc. 2014 Mallinckrodt Pharmaceuticals 2018 Sun Pharmaceutical 2017 Alkermes, Inc. 2019 electroCore, Inc. 2020 MannKind Corporation 1999 Sunovion Pharmaceuticals, Inc. 2019 Alnylam Pharmaceuticals 2010 Endo Pharmaceuticals 1999 Marketing Assessment, Inc. 2016 Taiho Oncology, Inc. 2019 Altarum Institute 2017 Exelixis 2009 Masimo Corporation 2015 Takeda Oncology 2020 Amarin Corporation 2016 Express Scripts Federal Pharmacy 2019 Medical Strategies International, LLC 2000 Takeda Pharmaceutical USA, Inc. 1994 AmerisourceBergen 2010 Federal Practitioner 2016 Melling Medical 2020 Telemynd 1992 Amgen 2021 Ferring Pharmaceuticals Inc. 1954 Merck & Co., Inc. 2020 TerSera Therapeutics 2020 Amneal Pharmaceutical 2018 Foundation Medicine, Inc. 2002 MerzNorth America 1990 Teva 2019 Aptive Resources LLC 2021 Frontier Technology Inc. -

CY 2020 CDER Drug and Biologic Calendar Year Approvals As of December 31, 2020
CY 2020 CDER Drug and Biologic Calendar Year Approvals As of December 31, 2020 This report reflects the data shown as it is identified in the database. Selection Criteria: User Response: Start Date: 1/1/2020 End Date: 12/31/2020 Sort Order: Approval Date New Drug Application (NDA) Approvals: APPLICATION REVIEW 505(B)(2) PROPRIETARY NAME ESTABLISHED NAME APPLICANT APPROVAL DATE NUMBER CLASSIFICATION APPROVAL NDA 212608 AYVAKIT AVAPRITINIB BLUEPRINT MEDICINES CORP P,O 1/9/2020 CODY LABORATORIES INC A WHOLLY OWNED NDA 209575 NUMBRINO COCAINE HYDROCHLORIDE SUBSIDIARY OF LANNETT CO INC S Y 1/10/2020 NDA 211635 VALTOCO DIAZEPAM NEURELIS INC S,O Y 1/10/2020 NDA 208171 MONOFER FERRIC DERISOMALTOSE PHARMACOSMOS AS S 1/16/2020 NDA 211723 TAZVERIK TAZEMETOSTAT EPIZYME INC P,O 1/23/2020 NDA 213138 DIFICID FIDAXOMICIN CUBIST PHARMACEUTICALS LLC P,O 1/24/2020 EMPAGLIFLOZIN, LINAGLIPTIN, AND BOEHRINGER INGELHEIM PHARMACEUTICALS NDA 212614 TRIJARDY XR METFORMIN HYDROCHLORIDE INC S 1/27/2020 NDA 213224 BYNEFEZIA PEN OCTREOTIDE ACETATE SUN PHARMACEUTICAL INDUSTRIES LTD S Y 1/28/2020 NDA 211281 PIZENSY LACTITOL BRAINTREE LABORATORIES INC S Y 2/12/2020 ETHINYL ESTRADIOL AND NDA 204017 TWIRLA LEVONORGESTREL AGILE THERAPEUTICS INC S Y 2/14/2020 NDA 213491 PROCYSBI CYSTEAMINE BITARTRATE HORIZON PHARMA USA INC S,O Y 2/14/2020 NDA 210583 ANJESO MELOXICAM BAUDAX BIO INC S Y 2/20/2020 NDA 211616 NEXLETOL BEMPEDOIC ACID ESPERION THERAPEUTICS INC S 2/21/2020 NDA 209510 BARHEMSYS AMISULPRIDE ACACIA PHARMA LTD S Y 2/26/2020 NDA 211617 NEXLIZET BEMPEDOIC ACID AND EZETIMIBE -

Table of Contents
Table of contents Executive Summary Chapter 1 – Introduction Chapter 2 – Trends in drug delivery dealmaking 2.1. Introduction 2.2. Drug delivery partnering over the years 2.3. Bigpharma drug delivery dealmaking activity 2.4. Big biotech drug delivery dealmaking activity 2.5. Most active drug delivery dealmakers 2.6 Drug delivery partnering by deal type 2.7. Drug delivery partnering by disease type 2.8. Partnering by drug delivery technology type 2.9. Average deal terms for drug delivery partnering 2.9.1 Drug delivery headline values 2.9.2 Drug delivery upfront payments 2.9.3 Drug delivery milestone payments 2.9.4 Drug delivery royalty rates 2.10. The anatomy of drug delivery partnering 2.11. Drug delivery or specialty pharma? 2.11.1. Is specialty pharma the only way for drug delivery? 2.11.2. Best practice for optimizing drug delivery program development 2.11.3. The anatomy of a drug delivery deal 2.11.3.a. Case study 1: Alpharma – Durect 2.11.3.b. Case study 2: Bayer – MDRNA 2.11.3.c. Case study 3: Endo Pharmaceuticals – BioDelivery Sciences Chapter 3 – Leading drug delivery deals 3.1. Introduction 3.2. Top drug delivery deals by value Chapter 4 – Bigpharma drug delivery deals 4.1. Introduction 4.2. How to use bigpharma drug delivery partnering deals 4.3. Big pharma drug delivery partnering company profiles Abbott Actavis Inc (formerly Watson Pharmaceuticals) Actavis (merged with Watson Pharmaceuticals Oct 2012) Actelion Allergan Amgen Astellas AstraZeneca Baxter International Bayer Biogen Idec Boehringer Ingelheim Bristol-Myers Squibb Celgene CSL Daiichi Sankyo Dainippon Sumitomo Eisai Eli Lilly Endo Pharmaceuticals Forest Laboratories Galderma Gilead Sciences GlaxoSmithKline Grifols Hospira Johnson & Johnson Kyowa Hakko Kirin Lundbeck Menarini Merck & Co Merck KGaA Mylan Novartis Novo Nordisk Otsuka Pfizer Purdue Roche Sanofi Shionogi Shire Takeda Teva UCB Valeant Warner Chilcott Chapter 5 – Bigbiotech drug delivery deals 5.1. -

2021 Annual Meeting of Shareholders TABLE of CONTENTS
2021 Annual Meeting of Shareholders TABLE OF CONTENTS Bristol Myers 3 Squibb: The Story Who We Are: 2021 4 Director Nominees Majority Vote Standard and Mandatory Resignation Policy 10 How We Are Criteria for Board Membership 10 Selected and Director Independence 11 Director Succession Planning and Identification of Board Candidates 11 Elected Annual Evaluation Process 13 Active Board Oversight of Our Governance 14 How We Govern Board’s Role in Strategic Planning and Risk Oversight 14 and Are Governed Risk Assessment of Compensation Policies and Practices 15 Meetings of Our Board & Director Engagement 16 Annual Meeting of Shareholders 16 Codes of Conduct 16 Related Party Transactions 17 Disclosure Regarding Political Activities 18 Global Corporate Citizenship & Sustainability 18 Responsible Drug Pricing Strategy & Transparency 19 Board Leadership Structure 21 How We Are Committees of Our Board 23 Organized Written Communication 27 How to Proactive Shareholder Engagement 27 Communicate Responsiveness to Shareholder Feedback 28 With Us How We Are Paid Compensation of Directors 29 Message form the Compensation and Management Development Committee Chair 33 Executive Compensation Discussion and Analysis 34 Compensation Business Overview 34 2020 Named Executive Officers 35 2020 Business Results 35 Company Response to COVID-19 37 Commitment to Diversity & Inclusion 38 Human Capital Management 39 2020 Executive Compensation Program Overview 41 2020 Compensation Program - Named Executive Officers 44 Annual Incentive Plan Program Outcomes 48 2020